Abstract
Background
To assess the potential impact of azithromycin treatment in the first week following birth on 2-year outcomes in preterm infants with and without Ureaplasma respiratory colonization who participated in a double-blind, placebo-controlled randomized controlled trial.
Methods
Respiratory morbidity was assessed at NICU discharge and at 6, 12, and 22–26 months corrected age using pulmonary questionnaires. Comprehensive neurodevelopmental assessments were completed between 22 and 26 months corrected age. The primary and secondary composite outcomes were death or severe respiratory morbidity and death or moderate–severe neurodevelopmental impairment, respectively, at 22–26 months corrected age.
Results
One hundred and twenty-one randomized participants (azithromycin, N = 60; placebo, N = 61) were included in the intent-to-treat analysis. There were no significant differences in death or serious respiratory morbidity (34.8 vs 30.4%, p = 0.67) or death or moderate–severe neurodevelopmental impairment (47 vs 33%, p = 0.11) between the azithromycin and placebo groups. Among all trial participants, tracheal aspirate Ureaplasma-positive infants experienced a higher frequency of death or serious respiratory morbidity at 22–26 months corrected age (58%) than tracheal aspirate Ureaplasma-negative infants (34%) or non-intubated infants (21%) (p = 0.028).
Conclusions
We did not observe strong evidence of a difference in long-term pulmonary and neurodevelopment outcomes in preterm infants treated with azithromycin in the first week of life compared to placebo.
Impact
-
No strong evidence of a difference in long-term pulmonary and neurodevelopment outcomes was identified at 22–26 months corrected age in infants treated with azithromycin in the first week of life compared to placebo.
-
The RCT is the first study of 2-year pulmonary and neurodevelopmental outcomes of azithromycin treatment in ELGANs.
-
Provides evidence that ELGANs with lower respiratory tract Ureaplasma have the most frequent serious respiratory morbidity in the first 2 years of life, suggesting that a Phase III trial of azithromycin to prevent BPD targeting this population is warranted.
Similar content being viewed by others
Introduction
Infants with bronchopulmonary dysplasia (BPD) are at risk for adverse pulmonary outcomes during childhood and into adulthood.1,2,3 Up to 50% of BPD infants require re-hospitalization in the first year of life.4,5,6 Since respiratory health may continue to evolve over the first few years of life and BPD and adverse neurodevelopmental outcomes are closely linked,7,8 it is essential to include long-term pulmonary and neurodevelopmental assessments as part of any neonatal clinical trial to prevent BPD.
The genital mollicute species Ureaplasma parvum and Ureaplasma urealyticum are associated with adverse pregnancy outcomes9 and morbidities of prematurity, including BPD,10 necrotizing enterocolitis,11 and severe intraventricular hemorrhage (IVH).12,13,14 Although macrolides have antimicrobial and immmumodulatory properties making them ideal therapeutic candidates for Ureaplasma eradication, none of the prior studies of macrolides for prevention of BPD included long-term follow-up.15,16,17
We conducted a series of pharmacokinetic/pharmacodynamic open-label studies of intravenous azithromycin (AZM)18,19,20 to select a safe, effective dose for the recently completed pilot (Phase IIb) randomized clinical trial of multi-dose AZM (20 mg/kg × 3 days) in extremely low gestational age newborns (ELGANs, 24–28 weeks gestation).21 The results of this trial demonstrated that (1) a 3-day course of AZM effectively eradicated Ureaplasma in ELGAN infants and (2) perinatal mortality and prolonged respiratory support are concentrated in ELGANs who have Ureaplasma in the lower respiratory tract. To determine the long-term safety of neonatal AZM therapy and the potential impact on long-term outcomes, pulmonary and neurodevelopmental outcomes were assessed at 22–26 months corrected age in participants of the randomized controlled trial (RCT).
Methods
Study design
The study design was a prospective, randomized, double-blind, placebo-controlled trial (clinicaltrials.gov NCT01778634) as recently described.21 The sample size for the trial was calculated to provide good power to detect moderate differences in the primary outcome of Ureaplasma-free survival to discharge. The U.S. Food and Drug Administration (IND78990) and the Institutional Review Board of each participating institution approved the study protocol including follow-up. Written parental consent was obtained for all participants prior to randomization. One hundred and twenty-one ELGAN infants (gestational age 240 to 286 weeks) were enrolled and randomized at 7 U.S. centers between July 2013 and August 2016.21 After baseline respiratory samples were obtained, participants were randomized to receive either intravenous AZM (American Pharmaceuticals Partners, Schaumburg, IL) 20 mg/kg at a concentration of 2 mg/ml in 5% dextrose water or equal volume of 5% dextrose water (10 ml/kg) as a placebo administered every 24 h for 3 doses. Randomization was performed using permuted block design with stratification by site and gestational age (240–266 vs 270–286 weeks) and assigned in 1:1 ratio to AZM or placebo with twins assigned to the same treatment. Since rapid diagnostic testing for Ureaplasma spp. was not feasible, presence of Ureaplasma colonization was unknown prior to dosing. All tracheal and nasopharyngeal aspirate samples were frozen at −80 °C at each study site and batch-shipped to the University of Alabama at Birmingham Diagnostic Mycoplasma Laboratory for Ureaplasma culture, species-specific real-time PCR and AZM susceptibility testing. Ureaplasma eradication was defined as three negative cultures post-treatment.21
Assessments
Data collected at baseline and during hospitalization included demographic variables such as gestational age, birth weight, sex, race, and ethnicity, and neonatal morbidities, including IVH grade, periventricular leukomalacia, necrotizing enterocolitis stage, late-onset sepsis, patent ductus arteriosus, retinopathy of prematurity stage, and postnatal steroid use, tracheostomy placement, postmenstrual age (PMA) at the time of discharge to home, and modes and duration of respiratory support.21 BPD was classified as physiologic based on a room air challenge,22 modified Shennan based on supplemental oxygen use at 36 weeks PMA or time of transfer prior to 36 weeks PMA,23 and NIH BPD severity definitions.24 Socioeconomic factors, including insurance status, maternal education and marital status, and primary language spoken at home were collected at the 22–26-month corrected age visit. For all neonatal intensive care unit (NICU) and follow-up assessments, the examiners were masked to treatment assignment and Ureaplasma colonization status. Only the pharmacists at each site were unblinded to treatment assignment.
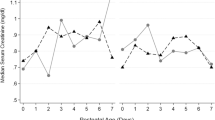
Pulmonary questionnaires
Structured parental interviews were conducted before discharge and by follow-up phone interviews at 6, 12, and 22–26 months corrected age using the validated Tucson Children’s Respiratory Study questionnaires.25,26,27 Follow-up interview windows were 5–9 months corrected age with an ideal interview date at 6 months corrected age, 10–18 months with an ideal interview date at 12 months, and 19–30 months with the ideal date at 24 months corrected age. At the time of each parental interview, the parent/caregiver was asked to provide responses based on the interval since the last interview. Information was elicited on family history of asthma and atopy, the home environment such as presence of pets and tobacco smoke exposure, the frequency and characteristics of wheezing and cough, use of respiratory medications including diuretics, nebulized bronchodilators, inhaled or systemic steroids, supplemental oxygen, and respiratory illness-related hospitalizations, physician visits, or emergency room (ER) visits. Parental report of their child experiencing cough without a cold “most of the time” during an interval was classified as chronic cough and parental report of wheezing “almost every day” during an interval was classified as chronic wheezing.
Neurodevelopmental assessments
Surviving infants completed comprehensive neurodevelopmental assessments between 22 and 26 months corrected age. Neurologic examinations28 that included a standardized assessment of reflexes, muscle tone, and strength were classified as normal, suspect (mildly abnormal neurologic exam without functional impairment), abnormal with functional impairment due to noncerebral palsy, or abnormal due to cerebral palsy (CP). Gross motor performance was evaluated using the modified Gross Motor Function Classification System (GMFCS) with scores ranging from 0 (normal) to 5 (most impaired).29 CP severity was classified as mild (GMFCS level 1), moderate (GMFSC levels 2–3), or severe (GMFCS levels 4–5).30 Certified examiners assessed cognitive function using the Bayley Scales of Infant and Toddler Development, third edition (BSID-III).31 For participants whose parents were unable to bring them to the clinic for in-person assessments, a parental phone interview was conducted to complete the Ages and Stages Questionnaire, Third Edition (ASQ3) to score developmental milestones in five domains (communication, fine motor, gross motor, problem-solving ability, and personal–social functioning).32 Hearing impairment (inability to understand the examiner’s verbal directions and to communicate, with or without amplification) were assessed by observation, parental report, or follow-up audiologic assessments.33 Vision impairment defined as vision worse than 20/200 was obtained by parental report or post-discharge eye exams. If unable to complete either in-person assessments or the phone interview ASQ3, information was extracted from chart review to classify the child for neurodevelopmental impairment (NDI).
Outcomes
The primary outcome for the follow-up phase of the trial was the composite outcome of death prior to 26 months corrected age or serious respiratory morbidity, defined as the occurrence of one or more of the following: tracheostomy; continued hospitalization for respiratory reasons at or beyond 50 weeks PMA, use of supplemental oxygen or respiratory support at 22–26 months corrected age, or ≥2 rehospitalizations for respiratory illness.34 The secondary outcome was the composite outcome of death prior to 26 months corrected age or moderate-to-severe NDI at 22–26 months corrected age defined as any one of the following: BSID-III cognitive composite score <85 or ASQ score >2 SD below the mean on any domain,32 GMFCS score ≥2, moderate or severe CP, blindness, and/or severe hearing impairment that cannot be corrected by amplification.30 Other secondary outcomes included mortality, the components of the pulmonary and neurodevelopmental composite outcomes, parental report of chronic wheezing or cough, doctor/ER visits for respiratory illness, and respiratory medication use during the first 22–26 months corrected age.
Statistical analysis
For the efficacy analysis, we compared the composite outcome death or serious respiratory morbidity at 22–26 months corrected age and other outcomes among all randomized participants according to the principle of intention-to-treat and in the subgroups of Ureaplasma-positive and negative participants. To account for possible correlation between outcomes in twins, we used generalized estimating equations35 and multiple outputation to calculate p values and confidence intervals.36 When observed counts were small, we used exact methods without accounting for twinning to calculate p values.
We did not collect a 22–26 month lung assessment for 15 of the children. To retain these children in the analyses described above, we multiply imputed the outcomes based on information gathered in the 6- and 12-month follow-up surveys and on respiratory variables observed prior to discharge. Binary outcomes were imputed based on their estimated probability. Twenty-five data sets with imputations were created and the final results were combined using Rubins approach.37
Treatment groups were compared with respect to the median value of several quantitative outcomes, including PMA at discharge to home and when supplemental oxygen was discontinued. To include children who died during the NICU hospitalization in the analysis appropriately, we used a rank-based (Wilcoxon test) analysis and gave these children the worst ranks.
In post hoc analyses, we explored the impact of upper and lower respiratory tract Ureaplasma colonization on the follow-up primary and major secondary outcomes.
All analyses were performed using SAS 9.4.
Results
Characteristics of the study population
Of the 121 ELGAN infants randomized, 60 were assigned to AZM and 61 to placebo; 119 (98%) received at least one dose of the assigned treatment (Fig. 1).21 One placebo-assigned infant who was nasopharyngeal Ureaplasma positive received a single dose of AZM due to pharmacy error. The baseline characteristics of the study cohort and when stratified by Ureaplasma colonization status were similar between treatment arms, except for an imbalance in race distribution that occurred with 40% non-white in the AZM vs 75% in the placebo group (Table 1). Forty-four of the 121 (36%) participants were Ureaplasma positive at one or more timepoints with 19 randomized to AZM and 25 to placebo (Table 1).
One participant in each treatment arm did not receive assigned treatment. Asterisk (*): one participant assigned to the placebo group, received one dose of azithromycin due to investigational pharmacy error but received placebo for other 2 doses. All participants were included in intent-to-treat analysis.
Eleven participants died prior to discharge from the NICU (AZM, N = 5; placebo, N = 6) and 1 AZM-assigned participant died after discharge and prior to 22–26-month corrected age. At least one post-discharge questionnaire was completed for 105/109 survivors (96%). At 22–26 months corrected age, 94 (86%) completed pulmonary assessments and 95 (87%) completed neurodevelopmental assessments (Fig. 1). Socioeconomic factors such as frequency of medical assistance insurance and maternal education and environmental factors such as daycare attendance and tobacco smoke exposure were similar between treatment arms. Family history of asthma and atopy was common for participants in both treatment arms.
Primary pulmonary outcome
The primary composite pulmonary outcome of death prior to 22–26 months corrected age or serious respiratory morbidity was similar in the AZM (34.8%) compared to the placebo (30.4%) group (risk difference 4%, 95% confidence interval −14 to 21%, p = 0.67; Table 2) and in analyses stratified by race (Supplemental Table 1). The distribution of the components of the serious respiratory morbidity outcome was similar between the treatment groups (Supplemental Fig. 1). There were no differences in PMA at the time of discharge to home or when supplemental oxygen was discontinued. Among those positive for Ureaplasma, AZM-assigned participants had similar mortality (16% both groups) but significantly higher incidence of serious respiratory morbidity than placebo-assigned participants (45 vs 15%) (p = 0.036; Table 2). There was no difference in incidence of serious respiratory morbidity in Ureaplasma-negative infants. Parental report of chronic cough or wheezing was similar in both the treatment groups. Use of one or more respiratory medication during any interval in the first 2 years was high in both the groups (AZM, 65%; placebo, 62%), with nebulized albuterol as the most frequent medication used in both the groups. There were no appreciable differences in percentage of children who were hospitalized one or more times for respiratory illness between treatment arms and when stratified by Ureaplasma status.
Neurodevelopmental outcomes
NDI classification was successfully assigned for 93/109 (85%) survivors (BSID-III, N = 43; ASQ3, N = 44; and medical record review, N = 6; Table 3). The observed frequency of the composite outcome of death or moderate-to-severe NDI was 47% for the AZM treatment and 33% for the placebo arms for the entire cohort with risk difference 16% after adjusting for twins (95% confidence interval −2 to 34%, p = 0.11). There were no significant differences in composite outcome of death or moderate–severe NDI when stratified by Ureaplasma respiratory colonization status (Table 3) or race (Supplemental Table 1). There were no significant differences between treatment arms for the individual components of NDI, including the frequency of BSID-III composite cognitive score <85 or ASQ3 >2 SD below the mean in any domain and moderate–severe CP or GMFCS score ≥2. In addition, there was no difference between groups for BSID-III cognitive composite score using cutoff <70. Of note, infants who had any grade IVH had a significantly increased risk for moderate-to-severe NDI and cognitive impairment than infants without IVH after controlling for treatment in logistic regression analysis (p = 0.024) (Supplemental Fig. 2). No surviving participant was blind or had disabling hearing impairment.
Post hoc analyses
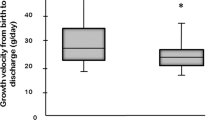
We had previously observed that Ureaplasma-free survival, overall survival, and physiologic BPD-free survival were lower and durations of hospitalization, mechanical ventilation and supplemental oxygen, and postnatal steroid exposure were higher in intubated patients with lower respiratory tract Ureaplasma colonization compared to intubated infants without lower tract involvement or non-intubated infants.21 At follow-up, differences in unfavorable pulmonary outcomes persisted in children who had lower respiratory tract Ureaplasma colonization. Tracheal aspirate Ureaplasma-positive infants were discharged to home and supplemental oxygen was discontinued at later PMA and they experienced a higher frequency of the composite outcome death or serious respiratory morbidity at 22–26 months corrected age than tracheal aspirate Ureaplasma-negative infants and non-intubated infants (Table 4). There were no differences among the three groups for death or moderate-to-severe NDI. To assess the long-term effect of neonatal lower respiratory tract Ureaplasma colonization in the absence of treatment, we compared outcomes of placebo-treated tracheal aspirate Ureaplasma-positive and Ureaplasma-negative infants (Supplemental Table 2). Placebo-treated tracheal aspirate Ureaplasma-positive infants were discharged to home at a later PMA. Although the differences were not statistically significant, all-cause mortality (36 vs 9%, p = 0.07) and mortality from respiratory causes (18 vs 0%, p = 0.098) was greater in the Ureaplasma-positive group than for infants assigned to placebo. In patients with lower respiratory tract Ureaplasma colonization, death or serious respiratory morbidity was 60% (6/10) in AZM-treated vs 56% (6/11) in placebo-treated infants (p = 0.61; Table 5).
Discussion
We conducted 22–26-month corrected age follow-up for this Phase IIb RCT to assess the potential impact of AZM therapy on long-term pulmonary and neurodevelopmental outcomes. We have previously published the primary efficacy outcome analysis showing that intravenous AZM 20 mg/kg for 3 days effectively eradicates Ureaplasma respiratory colonization.21 In the follow-up study, we did not find strong evidence for an impact of neonatal exposure to AZM on later pulmonary and neurodevelopment outcomes. Based on the 95% confidence interval (−14 to 21%), our data do not rule out either a moderately reduced or moderately increased risk of death or serious respiratory morbidity at 22–26 months corrected age in those receiving AZM relative to placebo. Similarly, the 95% confidence interval for difference in death or NDI between treatment groups is broad (−2 to 34%). Importantly, we observed that infants who had lower respiratory tract Ureaplasma colonization in the neonatal period had persistent adverse pulmonary outcomes, including greater risk for the composite outcome death or serious respiratory morbidity, suggesting that these infants should be targeted in future trials.
Since the widely used BPD definitions are poor predictors of subsequent respiratory illness later in childhood, consensus is lacking among neonatologists on which clinically meaningful short- and long-term endpoints should be targeted in clinical trials of BPD prevention.23,38,39,40 In the current follow-up study, we chose the composite outcome of death or serious respiratory morbidity defined by Jensen et al.34 as the primary outcome. The components of the serious respiratory morbidity definition could be ascertained from the electronic medical records for the majority of subjects and they represent meaningful clinical outcomes7 and are factors that impact parents’ perceptions of quality of life for their children41 and inform healthcare providers.5 Jensen et al.34 determined that a revised BPD definition that categorized lung disease severity according to mode of respiratory support at 36 weeks PMA rather than supplemental oxygen best predicted serious respiratory morbidity in the first 2 years of life in preterm infants born <27 weeks gestation.
Questionnaires that rely on parental recall of respiratory symptoms, medication use, and physician visits have been commonly used in studies of pulmonary outcomes in preterm infants.27,42,43 The potential for parental recall bias of respiratory symptoms such as wheezing has been debated in previous studies.44,45 To reduce recall bias in the current study, we used the validated Tucson Children’s Respiratory Study questionnaires administered by trained personnel at 4 timepoints during the first 2 years of life. Approximately two-thirds of parents reported family history of asthma and/or atopy. Respiratory medication use prevalence was ~65% in surviving children in both treatment arms with nebulized albuterol the most frequently reported medication. Respiratory medication use was similar to rates reported in other ELGAN cohorts during the first few years of life.27,34,43 Whether these medications were prescribed for BPD or viral infection-related wheezing is not known.
Ureaplasma respiratory tract colonization has been proposed as an etiologic factor in reactive airway disease in young infants. Wheezing in infants and children <3 years of age has been associated with isolation of Ureaplasma from the upper respiratory tract.46 There was no significant difference in parental-reported chronic cough or wheezing in children who were Ureaplasma tracheal aspirate positive compared to those children who had been tracheal aspirate negative or never intubated. In post hoc analysis of placebo-treated intubated infants with and without lower tract Ureaplasma colonization, Ureaplasma-colonized infants were discharged to home at later PMA, suggesting a more complicated NICU course in colonized infants.
We examined the impact of AZM treatment in the first few days of life on later NDI, a treatment effect that has not been previously reported. The rate of death or moderate-to-severe NDI in the current study cohort is similar to rates reported in other neonatal cohorts.30,34 Although AZM has been proposed as a neuroprotective agent in neonatal animal models,47 there was no apparent benefit in neurodevelopmental measures by treatment group or when stratified by Ureaplasma status. Despite worse pulmonary morbidity, infants with lower respiratory tract Ureaplasma infection had similar rate of death or moderate–severe NDI as intubated infants without lower tract involvement or non-intubated infants. In multiple previous studies, BPD severity was a risk factor for adverse neurodevelopmental outcomes.7,8 However, in a recent single-center birth cohort, BSID-III cognitive scores were not associated with BPD severity.48
AZM has a low incidence of side effects in adults and children aged >2 years, primarily gastrointestinal symptoms.49 The safety of AZM in preterm infants has been assessed in a systematic review of 11 neonatal RCTs and observational studies.17 The majority of adverse events in the neonatal period were related to prematurity and were assessed as unlikely associated with AZM treatment. Although infantile hypertrophic pyloric stenosis has been associated with AZM exposure in the first few weeks of life,50,51 only 4 cases were identified in 473 infants included in the systematic review and there were no cases in the current trial. In addition, AZM is pro-arrhythmogenic with prior reports of occurrences of QT-interval prolongation and torsade’s de pointes in adults52 but has not been observed in neonates treated with therapeutic doses.
Long-term safety of neonatal AZM exposure has not been previously addressed. In our small sample of children who were Ureaplasma positive from upper and/or lower airways, there was significantly greater serious respiratory morbidity in the AZM-assigned group than in the placebo-assigned group. A larger trial will be needed to determine whether this finding is directly related to neonatal AZM exposure or is due to random variation. This observation underscores the importance of delaying adopting AZM therapy to prevent BPD into clinical practice until a Phase III RCT is completed. There is an ongoing AZM therapy for chronic lung disease of prematurity (AZTEC) Phase III RCT of a 10-day course of AZM (20 mg/kg × 3 days, followed by 10 mg/kg for a further 7 days) that will enroll 796 preterm infants <30 weeks gestation to determine the safety and efficacy of this regimen to improve survival without BPD.53
Study limitations
Our sample size had good power to detect a treatment effect on the primary outcome of clearance of Ureaplasma, but we had insufficient power to exclude small-to-moderate differences between the groups for long-term pulmonary and neurodevelopmental outcomes. To indicate the range of group differences that could not be ruled out with our data, we presented 95% confidence intervals. Also, we recognize that relationships suggested early in follow-up—close in time to characterization with regard to Ureaplasma or AZM treatment—can be expected to attenuate as other exposures such as viral illnesses and differences in home environment influence pulmonary and neurological outcomes, further eroding statistical power. Attrition at the 22–26-month corrected age assessment timepoint may have introduced ascertainment bias since higher rates of NDI are significantly correlated with increased loss to follow-up in a systematic review of 43 follow-up studies of ELGAN infants.54
Study implications summary
The results of this trial extend the observation that mortality and prolonged respiratory support are concentrated in ELGANs who have Ureaplasma in the lower respiratory tract and inform the design of a future Phase III trial targeting Ureaplasma-colonized infants. An adequately powered Phase III clinical trial limited to ELGAN infants with PCR-confirmed lower respiratory tract Ureaplasma would determine whether or not a 3-day course of AZM is of clinical benefit to reduce short- and long-term pulmonary morbidity.
References
Sillers, L., Alexiou, S. & Jensen, E. A. Lifelong pulmonary sequelae of bronchopulmonary dysplasia. Curr. Opin. Pediatr. 32, 252–260 (2020).
Yang, J. et al. Lung function of adults born at very low birth weight. Pediatrics 145, e20192359 (2020).
Gibbons, J. T. D., Wilson, A. C. & Simpson, S. J. Predicting lung health trajectories for survivors of preterm birth. Front. Pediatr. 8, 318 (2020).
Hibbs, A. M. et al. One-year respiratory outcomes of preterm infants enrolled in the nitric oxide (to prevent) chronic lung disease trial. J. Pediatr. 153, 525–529 (2008).
Ambalavanan, N. et al. Identification of extremely premature infants at high risk of rehospitalization. Pediatrics 128, e1216–e1225 (2011).
Greenough, A. Long-term respiratory consequences of premature birth at less than 32 weeks of gestation. Early Hum. Dev. 89(Suppl 2), S25–S27 (2013).
Zhang, H. et al. Prolonged respiratory support of any type impacts outcomes of extremely low birth weight infants. Pediatr. Pulmonol. 53, 1447–1455 (2018).
Cheong, J. L. Y. & Doyle, L. W. An update on pulmonary and neurodevelopmental outcomes of bronchopulmonary dysplasia. Semin. Perinatol. 42, 478–484 (2018).
Murtha, A. P. & Edwards, J. M. The role of mycoplasma and ureaplasma in adverse pregnancy outcomes. Obstet. Gynecol. Clin. North Am. 41, 615–627 (2014).
Lowe, J. et al. Association between pulmonary ureaplasma colonization and bronchopulmonary dysplasia in preterm infants: updated systematic review and meta-analysis. Pediatr. Infect. Dis. J. 33, 697–702 (2014).
Okogbule-Wonodi, A. C. et al. Necrotizing enterocolitis is associated with ureaplasma colonization in preterm infants. Pediatr. Res. 69, 442–447 (2011).
Viscardi, R. M. et al. Incidence of invasive ureaplasma in VLBW infants: relationship to severe intraventricular hemorrhage. J. Perinatol. 28, 759–765 (2008).
Kasper, D. C. et al. In utero exposure to ureaplasma spp. Is associated with increased rate of bronchopulmonary dysplasia and intraventricular hemorrhage in preterm infants. J. Perinat. Med. 39, 331–336 (2011).
Huang, J. et al. Antenatal infection and intraventricular hemorrhage in preterm infants: a meta-analysis. Medicine 98, e16665 (2019).
Ozdemir, R. et al. Clarithromycin in preventing bronchopulmonary dysplasia in Ureaplasma urealyticum-positive preterm infants. Pediatrics 128, e1496–e1501 (2011).
Nair, V., Loganathan, P. & Soraisham, A. S. Azithromycin and other macrolides for prevention of bronchopulmonary dysplasia: a systematic review and meta-analysis. Neonatology 106, 337–347 (2014).
Smith, C. et al. Use and safety of azithromycin in neonates: a systematic review. BMJ Open 5, e008194 (2015).
Hassan, H. E. et al. Pharmacokinetics, safety, and biologic effects of azithromycin in extremely preterm infants at risk for ureaplasma colonization and bronchopulmonary dysplasia. J. Clin. Pharmacol. 51, 1264–1275 (2011).
Viscardi, R. M. et al. Azithromycin to prevent bronchopulmonary dysplasia in ureaplasma-infected preterm infants: pharmacokinetics, safety, microbial response, and clinical outcomes with a 20-milligram-per-kilogram single intravenous dose. Antimicrob. Agents Chemother. 57, 2127–2133 (2013).
Merchan, L. M. et al. Pharmacokinetics, microbial response, and pulmonary outcomes of multidose intravenous azithromycin in preterm infants at risk for ureaplasma respiratory colonization. Antimicrob. Agents Chemother. 59, 570–578 (2015).
Viscardi, R. M. et al. Randomised trial of azithromycin to eradicate ureaplasma in preterm infants. Arch. Dis. Child. Fetal Neonatal Ed. https://doi.org/10.1136/fetalneonatal2019-318122 (2020).
Natarajan, G. et al. Outcomes of extremely low birth weight infants with bronchopulmonary dysplasia: impact of the physiologic definition. Early Hum. Dev. 88, 509–515 (2012).
Poindexter, B. B. et al. Comparisons and limitations of current definitions of bronchopulmonary dysplasia for the prematurity and respiratory outcomes program. Ann. Am. Thorac. Soc. 12, 1822–1830 (2015).
Jobe, A., Ikegami, M., Jacobs, H. & Jones, S. Surfactant and pulmonary blood flow distributions following treatment of premature lambs with natural surfactant. J. Clin. Investig. 73, 848–856 (1984).
Martinez, F. D. et al. Asthma and wheezing in the first six years of life. The group health medical associates. N. Engl. J. Med. 332, 133–138 (1995).
Taussig, L. M. et al. Tucson children’s respiratory study: 1980 to present. J. Allergy Clin. Immunol. 111, 661–675 (2003).
Stevens, T. P. et al. Respiratory outcomes of the surfactant positive pressure and oximetry randomized trial (SUPPORT). J. Pediatr. 165, 240.e4–249.e4 (2014).
Amiel-Tison, C. & Gosselin, J. Neurological Development from Birth to Six Years: Guide for Examination and Evaluation (Johns Hopkins University Press, 2001).
Palisano, R. J. et al. Validation of a model of gross motor function for children with cerebral palsy. Phys. Ther. 80, 974–985 (2000).
Adams-Chapman, I. et al. Neurodevelopmental impairment among extremely preterm infants in the neonatal research network. Pediatrics 141, e20173091 (2018).
Greene, M. M., Patra, K., Nelson, M. N. & Silvestri, J. M. Evaluating preterm infants with the bayley-III: patterns and correlates of development. Res. Dev. Disabil. 33, 1948–1956 (2012).
Kerstjens, J. M. et al. The ages and stages questionnaire and neurodevelopmental impairment in two-year-old preterm-born children. PLoS ONE 10, e0133087 (2015).
Vaucher, Y. E. et al. Neurodevelopmental outcomes in the early cpap and pulse oximetry trial. N. Engl. J. Med. 367, 2495–2504 (2012).
Jensen, E. A. et al. The diagnosis of bronchopulmonary dysplasia in very preterm infants. An evidence-based approach. Am. J. Respir. Crit. Care Med. 200, 751–759 (2019).
Zeger, S. L., Liang, K. Y. & Albert, P. S. Models for longitudinal data: a generalized estimating equation approach. Biometrics 44, 1049–1060 (1988).
Follmann, D., Proschan, M. & Leifer, E. Multiple outputation: inference for complex clustered data by averaging analyses from independent data. Biometrics 59, 420–429 (2003).
Rubin, D. B. Multiple Imputation for Nonresponse in Surveys (Wiley, 1987).
Poindexter, B. B. & Jobe, A. H. The diagnostic conundrum of bronchopulmonary dysplasia. J. Pediatr. 167, 517–518 (2015).
Maitre, N. L. et al. Respiratory consequences of prematurity: evolution of a diagnosis and development of a comprehensive approach. J. Perinatol. 35, 313–321 (2015).
Steinhorn, R. et al. Chronic pulmonary insufficiency of prematurity: developing optimal endpoints for drug development. J. Pediatr. 191, 15–21 e11 (2017).
Brady, J. M., Zhang, H., Kirpalani, H. & DeMauro, S. B. Living with severe bronchopulmonary dysplasia-parental views of their child’s quality of life. J. Pediatr. 207, 117–122 (2019).
Morrow, L. A. et al. Antenatal determinants of bronchopulmonary dysplasia and late respiratory disease in preterm infants. Am. J. Respir. Crit. Care Med. 196, 364–374 (2017).
Ryan, R. M. et al. Respiratory medications in infants <29 weeks during the first year postdischarge: the Prematurity and Respiratory Outcomes Program (prop) Consortium. J. Pediatr. 208, 148.e3–155.e3 (2019).
Brick, T. et al. Parents know it best: prediction of asthma and lung function by parental perception of early wheezing episodes. Pediatr. Allergy Immunol. 30, 795–802 (2019).
Vissing, N. H., Jensen, S. M. & Bisgaard, H. Validity of information on atopic disease and other illness in young children reported by parents in a prospective birth cohort study. BMC Med. Res. Methodol. 12, 160 (2012).
Pinna, G. S., Skevaki, C. L. & Kafetzis, D. A. The significance of Ureaplasma urealyticum as a pathogenic agent in the paediatric population. Curr. Opin. Infect. Dis. 19, 283–289 (2006).
Barks, J. D. E., Liu, Y., Wang, L., Pai, M. P. & Silverstein, F. S. Repurposing azithromycin for neonatal neuroprotection. Pediatr. Res. 86, 444–451 (2019).
Brumbaugh, J. E., Colaizy, T. T., Patel, N. M. & Klein, J. M. The changing relationship between bronchopulmonary dysplasia and cognition in very preterm infants. Acta Paediatr. 107, 1339–1344 (2018).
Ruuskanen, O. Safety and tolerability of azithromycin in pediatric infectious diseases: 2003 update. Pediatr. Infect. Dis. J. 23, S135–S139 (2004).
Eberly, M. D., Eide, M. B., Thompson, J. L. & Nylund, C. M. Azithromycin in early infancy and pyloric stenosis. Pediatrics 135, 483–488 (2015).
Stark, C. M., Rogers, P. L., Eberly, M. D. & Nylund, C. M. Association of prematurity with the development of infantile hypertrophic pyloric stenosis. Pediatr. Res. 78, 218–222 (2015).
Ray, W. A., Murray, K. T., Hall, K., Arbogast, P. G. & Stein, C. M. Azithromycin and the risk of cardiovascular death. N. Engl. J. Med. 366, 1881–1890 (2012).
Lowe, J. et al. Study protocol: azithromycin therapy for chronic lung disease of prematurity (AZTEC) - a randomised, placebo-controlled trial of azithromycin for the prevention of chronic lung disease of prematurity in preterm infants. BMJ Open 10, e041528 (2020).
Guillen, U. et al. Relationship between attrition and neurodevelopmental impairment rates in extremely preterm infants at 18 to 24 months: a systematic review. Arch. Pediatr. Adolesc. Med. 166, 178–184 (2012).
Acknowledgements
We would like to thank the parents of the participants of this trial and staff of participating NICUs and site study coordinators Elise Janofsky, Ashley Bathgate, Jennifer Shepard, Monika J. Thielen, Tara McNair, Amy Mackley, Kelly Gray, and Steven Steele for assistance with patient recruitment. No compensation was received other than salary support for their contribution. We thank the University of Alabama Diagnostic Mycoplasma Laboratory Staff Donna Crabb and Melanie Fecanan for Ureaplasma culture and susceptibility testing and Amy Ratliffe for PCR. We thank the University of Maryland School of Medicine Clinical and Translational Research Informatics Center for data management. This study was funded by NICHD (R01 HD067126).
Author information
Authors and Affiliations
Contributions
R.M.V., M.L.T., and L.S.M. conceptualized and designed the study. R.M.V., S.J.D., K.B.W., M.A., A.A.-A., N.A., D.A.K., P.D., D.J.T., and J.-H.W. collected the data. R.M.V., M.L.T., L.S.M., and N.L.D. analyzed the data. All authors drafted and critically revised the article for important intellectual content and approved the final version to be published.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Patient consent
Written informed parental consent was required for the study. The study protocol was approved by each institutional IRB.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Viscardi, R.M., Terrin, M.L., Magder, L.S. et al. Randomized trial of azithromycin to eradicate Ureaplasma respiratory colonization in preterm infants: 2-year outcomes. Pediatr Res 91, 178–187 (2022). https://doi.org/10.1038/s41390-021-01437-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41390-021-01437-2
This article is cited by
-
Association of Ureaplasma infection pattern and azithromycin treatment effect with bronchopulmonary dysplasia in Ureaplasma positive infants: a cohort study
BMC Pulmonary Medicine (2023)
-
Follow-up study of infants recruited to the randomised, placebo-controlled trial of azithromycin for the prevention of chronic lung disease of prematurity in preterm infants—study protocol for the AZTEC-FU study
Trials (2022)