Abstract
Neuroinflammatory disorders preferentially impair the higher cognitive and executive functions of the prefrontal cortex (PFC). This includes such challenging disorders as delirium, perioperative neurocognitive disorder, and the sustained cognitive deficits from “long-COVID” or traumatic brain injury. There are no FDA-approved treatments for these symptoms; thus, understanding their etiology is important for generating therapeutic strategies. The current review describes the molecular rationale for why PFC circuits are especially vulnerable to inflammation, and how α2A-adrenoceptor (α2A-AR) actions throughout the nervous and immune systems can benefit the circuits in PFC needed for higher cognition. The layer III circuits in the dorsolateral PFC (dlPFC) that generate and sustain the mental representations needed for higher cognition have unusual neurotransmission and neuromodulation. They are wholly dependent on NMDAR neurotransmission, with little AMPAR contribution, and thus are especially vulnerable to kynurenic acid inflammatory signaling which blocks NMDAR. Layer III dlPFC spines also have unusual neuromodulation, with cAMP magnification of calcium signaling in spines, which opens nearby potassium channels to rapidly weaken connectivity and reduce neuronal firing. This process must be tightly regulated, e.g. by mGluR3 or α2A-AR on spines, to prevent loss of firing. However, the production of GCPII inflammatory signaling reduces mGluR3 actions and markedly diminishes dlPFC network firing. Both basic and clinical studies show that α2A-AR agonists such as guanfacine can restore dlPFC network firing and cognitive function, through direct actions in the dlPFC, but also by reducing the activity of stress-related circuits, e.g. in the locus coeruleus and amygdala, and by having anti-inflammatory actions in the immune system. This information is particularly timely, as guanfacine is currently the focus of large clinical trials for the treatment of delirium, and in open label studies for the treatment of cognitive deficits from long-COVID.
Similar content being viewed by others
Introduction
Stress and inflammation can profoundly alter the nervous and immune systems, creating long-term impairments in cognitive functioning. In particular, the cognitive functions of the prefrontal cortex (PFC) are impaired in a wide range of neuroinflammatory disorders, including in Alzheimer’s disease (AD) [1], traumatic brain injury (TBI) [2], and perioperative neurocognitive disorder (PND) [3]. The PFC subserves abstract reasoning and the executive functions, where deficits can be remarkably debilitating, interfering with the ability to work or care for families [4]. There is a great need for treatment, especially in the wake of COVID-19 infection, where cognitive deficits from “long-COVID” are prevalent [5]. However, there are no FDA-approved medications for treating neuroinflammatory cognitive disorders.
New research has shown that the recently evolved circuits in the primate PFC have unusual molecular needs that support higher cognitive operations, but render these circuits particularly vulnerable to disruption from neuroinflammation [6]. In particular, these circuits express the molecular machinery for cAMP to magnify calcium signaling to help sustain prolonged neuron firing needed to represent information without sensory stimulation. However, magnified cAMP-calcium signaling is readily dysregulated by stress and inflammation, leading to atrophy, tau phosphorylation and impaired PFC cognitive functioning. Thus, medications that can restore regulation of cAMP-calcium signaling may be especially helpful in restoring cognitive abilities.
As will be described in detail below, research has shown that the selective noradrenergic α2A-adrenoceptor (α2A-AR) agonist, guanfacine, can strengthen PFC network connections and improve PFC cognitive functioning by regulating cAMP-calcium signaling [7]. Based on this research, extended release guanfacine was approved by the FDA in 2009 for the treatment of Attention Deficit Hyperactivity Disorder, which is characterized by PFC deficits. Guanfacine is also being used off-label and/or being tested to treat cognitive deficits in a variety of neuroinflammatory disorders including traumatic brain injury (TBI), delirium (post-anesthetic or infectious), and cognitive deficits from long-COVID (“brain fog”). However, the scientific bases for guanfacine’s actions in these disorders are generally not understood, as this research has arisen from multiple, and often disparate, disciplines. While many scientists and physicians are aware of how stimulation of presynaptic α2A-AR autoreceptors reduces NE release from the sympathetic nervous system [8], they are often unaware of important, post-synaptic α2A-AR actions in brain that are especially relevant to cognitive functioning. The current review describes new data on why PFC circuits are so vulnerable to neuroinflammation, and how α2A-AR stimulation can coordinate a “safety signal” across the neuroaxis and the immune system that helps to restore normative brain and inflammatory functioning needed for healthy cognition.
The functions of the prefrontal cortex
The PFC enlarges greatly in primates and is topographically organized, with the dorsal and lateral regions (dlPFC) subserving cognitive functioning, and the ventral (i.e. orbital) and medial regions (vmPFC) regulating emotional states [4, 9,10,11]. These areas are tightly interconnected, e.g. with adaptable evaluations of reward values being conveyed from the vmPFC to the dlPFC, and the dlPFC providing top-down control of emotion via projections to the vmPFC [12].
dlPFC circuits have the extraordinary ability to generate, sustain, and manipulate representations of information in the absence of sensory inputs, the foundation of abstract thought and flexible behavioral responding [13]. These capabilities arise from extensive, recurrent excitatory connections on glutamate synapses in layer III that allow the PFC to sustain information without the need for sensory stimulation [13]. The dlPFC subserves higher order cognitive functions such as working memory, recall memory (but not recognition memory, which is more dependent on medial temporal lobe), abstract reasoning, and the executive functions e.g. planning and organization, and the regulation of attention and action [4, 14]. For example, dlPFC networks are needed to effectively divide or focus attention, suppressing interference and noise, and to inhibit inappropriate responses. They contribute to the brain networks that govern complex decision-making, social cognition and self-regulation. In humans, the lateral PFC also generates language, with verbal content generated in the dominant hemisphere, and emotional content generated in the nondominant hemisphere [4]. The most rostral PFC areas in the frontal pole [15] subserve metacognitive functions such as insight and judgment, and metamemory, i.e. remembering to remember. The frontal pole and the dlPFC provide important regulation of emotional states (motivation, anxiety, aggression, depression) through connections with the vmPFC. For example, dlPFC activity and/or synaptic integrity is related to the ability to overcome fatigue [16], stress [17, 18], and depression [19], emphasizing its important, top-down control of emotional state.
Prefrontal functions are impaired in a large number of neuroinflammatory disorders
PFC functioning is impaired in many neuroinflammatory disorders, even when it is not the primary/initial site of the insult. For example, in rat models, TBI to the posterior cortex impairs PFC function through a number of molecular changes in PFC in response to the distant injury [20,21,22,23]. PFC cognitive deficits can range from being relatively mild (although still debilitating), e.g. with executive dysfunction as the primary complaint, to very severe, e.g. profound deficits in delirium. Although delirium involves global deficits in multiple cognitive domains [24], mediated by multiple brain areas, those governed by the PFC can be particularly important to a coherent cognitive state. The following briefly reviews PFC cognitive dysfunction associated with common neuroinflammatory conditions.
Traumatic brain injury and chronic traumatic encephalopathy
The prevalence of PFC cognitive deficits following mild TBI has been appreciated for decades [25,26,27], including deficits in executive function as reflected in persistent impairment in performance of the Stroop interference task [28]. TBI also increases risk of depression and/or PTSD [29], a phenomenon also seen in rodents [30]. As described in more detail below, studies in rodents have shown that TBI to the posterior cortex evokes chemical changes in the PFC that impair working memory, even though the initial insult was distant from the PFC [20]. Thus, head injuries to nonfrontal aspects of the head can still result in impaired PFC functioning. Impaired PFC functions are also a major component of chronic traumatic encephalopathy (CTE) [31, 32], where the loss of inhibitory control over aggressive impulses and the increased prevalence of depression have received particular media attention.
Anesthesia and surgery
Some inhalational anesthetics produce residual cognitive deficits, especially in the elderly and/or young patients with repeated use [33] and reviewed in [34]. Pre-morbid impairments in PFC function (executive function, depression) are a risk factor for post-operative emergence delirium immediately after surgery [35]. In addition, postoperative cognitive disturbances, i.e. PND, can sometimes continue for months. The tasks most commonly used to assess pre- vs. post-operative cognitive performance are those that depend on the functional integrity of the PFC, e.g. tests of working memory, the Trails B test of flexible attention and inhibitory control, and the Stroop interference task [3]. However, recent data suggest that acute exposure to anesthesia alone, in the absence of surgery, did not impair cognition [36, 37], suggesting that the trauma of the surgical procedure itself is a critical interacting factor.
Hypoxia
The cognitive deficits following hypoxic events are variable based on the cause and duration of the hypoxia, but reviews describe that either acute or chronic hypoxia can impair attention, working/recall memory and executive functioning [38, 39]. Controlled experiments in rats show that chronic exposure to hypoxia impairs working memory in rats, and that it is associated with calcium dysregulation and dendritic spine loss from PFC neurons, i.e. loss of PFC connections [40].
Cognitive deficits from long-COVID
Patients often describe “brain fog” as a residual and persistent symptom of SARS-CoV-2 infection. It is noteworthy that these cognitive deficits often occur in patients who were never hospitalized with respiratory issues, indicating that they can occur independent of the hypoxia that accompanies severe COVID-19 illness [41]. These cognitive symptoms consistently include impairments in working memory, recall memory, abstract reasoning and the executive abilities, interfering with top-down control of attention, action and emotion [5, 41,42,43]. The sparing of recognition memory in long-COVID is consistent with the memory functions of the medial temporal lobe being less afflicted compared to operations dependent on the PFC [42]. Depression and anxiety are also common features of long-COVID [41], consistent with reduced regulation of emotion.
Delirium arising from critical illness
In contrast to long-COVID where cognitive deficits outlast the initial infection, the more severe cognitive deficits of delirium often occur during an active, systemic infection. By definition, delirium involves global deficits in multiple cognitive/attention domains [44]. However, the operations governed by the PFC may be particularly important for calming an agitated individual, and for effective communication [45]. The elderly are at much greater risk of delirium [24], and this may be related to the dysregulation of calcium signaling and rise in neuroinflammation in the aged PFC [6, 46, 47]. As described below, the α2A-adrenoceptor agonist, guanfacine, is currently being tested as a treatment for delirium in the context of critical illness, and its ability to reestablish PFC functioning may be an important beneficial component.
Unusual neurotransmission and neuromodulation renders dlPFC circuits especially vulnerable to neuroinflammation
The following sections describe the unique molecular characteristics of PFC circuits that render them so vulnerable to neuroinflammation, and which make them amenable to guanfacine treatment. Although this is an arena where there is still much to be learned, it is already evident that two major features of layer III dlPFC circuits confer vulnerability: 1) they have unique neurotransmission [48, 49] that makes them especially vulnerable to kynurenine inflammatory signaling, and 2) they have unusual neuromodulation, where feedforward cAMP-calcium signaling opens K+ channels to reduce neuronal firing, a process that can lead to toxic actions when regulation is weakened by inflammatory changes [6].
PFC circuits have unique neurotransmission that would be especially vulnerable to kynurenic acid inflammatory signaling
Unusual neurotransmission in dlPFC
Traditional glutamate neurotransmission requires AMPAR stimulation, which depolarizes the synaptic membrane, relieving the magnesium block of the NMDAR channel, and thus permitting and/or facilitating NMDAR neurotransmission [50, 51] (Fig. 1A). Thus, the depolarizing effects of AMPAR are considered “permissive” for NMDAR actions. Most AMPAR flux sodium but not calcium, and have rapid on/off characteristics that are especially amenable to coding sensory events. However, the synapses in layer III of dlPFC have very different neurotransmission, likely reflecting their need to sustain the neuronal firing of recurrent excitatory circuits for many seconds. As schematized in Fig. 1B, these neurons depend on NMDAR, with surprisingly little contributions of AMPAR stimulation [48]. Instead, the permissive excitation of the synaptic membrane is performed by acetylcholine stimulation of nic-α7R, which reside within the glutamate synapse [49]. The reliance on acetylcholine may be particularly important for coordinating dlPFC actions with arousal state, as acetylcholine is released during waking (conscious), but not deep sleep (unconscious). Studies in monkeys have shown that local blockade of NMDAR or nic-α7R markedly reduces the dlPFC neuronal firing needed for working memory, while systemic administration of NMDAR blockers impairs cognitive performance in monkeys and humans [48, 52, 53], and that cholinergic depletion of the dlPFC is devastating to working memory [54], demonstrating the importance of both NMDAR and cholinergic receptors to higher cognitive abilities.
A In a classic glutamate synapse, neurotransmission depends on AMPA receptors, which depolarize the postsynaptic membrane to eject Mg2+ from the NMDAR pore and allow NMDAR neurotransmission (i.e.”permissive” actions). The calcium entry through NMDAR can drive cAMP-PKA signaling to increase neuroplasticity and strengthen connections. cAMP is catabolized by PDE4s, which reduce memory formation. In traditional glutamate synapses, mGluR3 are often presynaptic, where they reduce glutamate release. B In contrast to traditional glutamate circuits which depend heavily on AMPAR, layer III dlPFC circuits have little AMPAR dependence, and instead rely most heavily on NMDAR and nic-α7R, which reside within the glutamate synapse and help to depolarize the postsynaptic membrane, needed to eject the Mg2+ for NMDAR actions. Depolarization may also be supported by high levels of calcium, including cAMP-PKA magnification of calcium release from the smooth endoplasmic reticulum (SER), shown in pink. Calcium in turn drives cAMP production, leading to feedforward signaling. Higher levels of cAMP-PKA-calcium signaling open K+ channels to weaken connectivity and have dynamic changes in synaptic strength, reducing firing under conditions of high cAMP-calcium signaling (see Fig. 2). Under healthy conditions, feedforward cAMP-PKA-calcium-K+ signaling is tightly regulated, by postsynaptic mGluR3 and α2A-AR inhibition of cAMP synthesis, by PDE4 catabolism of cAMP, and calbindin binding of cytosolic calcium.
Kynurenine inflammatory signaling
Under conditions of inflammation, there are large increases in the production of kynurenine. Kynurenine is metabolized from tryptophan in the immune system (e.g. by macrophages [55]) and in microglia [56], and may provide a source of cellular energy (nicotinamide adenine dinucleotide, i.e. NAD + ) [57]. Plasma kynurenine is actively taken up into brain [58], and thus peripheral insults can have indirect but large effects on brain functioning. Kynurenine can be further metabolized to quinolinic acid (QUIN), which kills neurons, or to kynurenic acid (KYNA) (Fig. 2), which blocks both NMDAR and nic-α7R [59]. (As charged metabolites (e.g. KYNA, QUIN) do not normally cross the blood-brain barrier, it can be difficult to glean possible CNS actions from serum levels of metabolites). Although neuronal apoptosis induced by QUIN may occur in some extreme conditions as described below, many chronic neuroinflammatory disorders with pronounced cognitive deficits are not associated with neuron death. In these disorders, high levels of KYNA may be responsible for cognitive deficits through KYNA blockade of NMDAR and nic-α7R. As the higher cognitive circuits of the dlPFC depend on these two receptors for neurotransmission, KYNA may disproportionately impair dlPFC functioning, producing the patterns of dlPFC cognitive deficits described above. In support of this hypothesis, inhibition of KYNA production in brain improved working memory in aged monkeys [60].
Kynurenine is made and released under inflammatory conditions and metabolized to KYNA in brain, where it blocks NMDAR and nic-α7R, which would greatly reduce dlPFC neurotransmission. Reactive microglia and astroctyes make and release GCPII, which catabolizes NAAG and thus reduces mGluR3 regulation of cAMP synthesis. There also can be loss of PDE4s and calbindin (not shown, see text). Psychological and physiological stress release high levels of catecholamines in PFC, that drive cAMP-PKA-calcium signaling; anesthesia can also increase calcium release from the SER. Dysregulated cAMP-PKA-calcium signaling leads to: 1) loss of neuronal firing via opening of K+ channels, 2) calcium overload of mitochondria, initiating inflammatory signaling including signals to microglia to remove synapses, and 3) tau hyperphosphorylation, e.g. through calpain 2 cleavage and activation of GSK3β and cdk5, the primary kinases that phosphorylate tau.
Neuroinflammatory disorders associated with elevated kynurenine signaling
Increased plasma kynurenine and/or KYNA levels in brain or CSF have been reported in a number of neuroinflammatory disorders, and with advancing age in humans [61]. The COVID-19 pandemic has brought increased attention to this mechanism, as infection by SARS-CoV-2 greatly increases plasma kynurenine levels [62,63,64]. Particularly relevant to the current review, cognitive deficits associated with “long-COVID” correlate with continued elevations of kynurenine in blood [65]. Assays of the brains of patients who have died from COVID-19 show large increases in KYNA [66], consistent with uptake and further metabolism in brain. It is likely that these findings with SARS-CoV-2 generalize to other types of infection that induce cognitive changes, as levels of delirium during critical illness also correlate with plasma kynurenine levels [67]. Elevated kynurenine signaling may also be related to post-surgical cognitive deficits, as presurgical elevations in plasma kynurenine correlated with post-surgical deficits in executive function and memory [68]. TBI is also associated with elevated kynurenine in patients and in animal models [69]. High levels of QUIN in CSF during the initial days after the injury are associated with more serious outcomes, including death [70]. However, there has been less research on CSF levels of kynurenine and its metabolites in chronic cognitive disorders associated with TBI where there is little evidence of apoptotic cell death.
PFC circuits have unique neuromodulation that magnifies toxic calcium actions and reduces neuronal firing under inflammatory conditions
Unusual neuromodulation in dlPFC
In addition to atypical neurotransmission, layer III pyramidal cells in the dlPFC also have unusual neuromodulation (Fig. 1B), where magnified calcium signaling is needed to support persistent neuronal firing, but high levels open potassium (K+) channels that markedly reduce neuronal firing, creating a narrow inverted-U [6]. These include cAMP opening of HCN and Slack channels [71, 72], PKA opening of KCNQ2 channels [46, 73, 74], and calcium opening of SK channels (Arnsten, unpublished). This differs from traditional neuromodulatory actions, where cAMP-calcium signaling produces a more uniform enhancement in neurotransmission [51] and enhances neuroplasticity [75, 76] (Fig. 1A).
As schematized in Fig. 1B, layer III dlPFC synapses express the molecular machinery for cAMP-PKA signaling to magnify calcium within the cytosol of layer III spines, including increasing internal calcium release from the smooth endoplasmic reticulum (SER), and by phosphorylating NMDAR and voltage-gated calcium channels to increase calcium entry. Calcium in turn promotes cAMP formation, leading to feedforward signaling. Layer III dlPFC spines also express a number of K+ channels that are opened by cAMP, PKA or calcium. Moderate levels of cAMP-calcium-K+ channel opening allows dynamic changes in network strength (Fig. 1B), as well as negative feedback to prevent seizures [6, 77], providing flexible, “top-down control” of our thoughts, actions and emotions when we feel safe, alert and interested (Fig. 3A). However, high levels of cAMP-calcium-K+ signaling, e.g. during stress and/or inflammation, functionally disconnects dlPFC synapses, greatly reducing neuronal firing (Fig. 2). This mechanism allows the dlPFC to be rapidly disconnected and silenced during an uncontrollable stressor, switching control of behavior to more primitive brain circuits that mediate habitual and emotional responding (Fig. 3B). This would have survival value in many dangerous conditions, e.g. being cut off on the highway while driving, but is detrimental when higher cognitive functions are needed to thrive [78, 79].
A Under nonstressful, healthy conditions, moderate levels of NE release engage high affinity α2A-ARs, strengthening the PFC and weakening the amygdala. Thus, there is strong top-down control of attention, action and emotion. B Under conditions of physiological or psychological stress, high levels of NE release activate low affinity α1-AR and β-AR, which weaken the PFC and strengthen the amygdala, switching the brain into a more primitive state. Treatment with the α2A-AR agonist, guanfacine, can transition the brain back into a regulated state.
Under conditions of psychological or physiological stress, high levels of norepinephrine (NE) are released in the PFC [80, 81] (Fig. 2). For example, studies in rats have shown that high levels of catecholamines are released in the PFC with traumatic brain injury, even though the concussion occurs at a large distance from the PFC [82]. High levels of NE engage low affinity receptors (e.g. α1A-AR) that drive calcium-cAMP opening of K+ channels (Fig. 2), rapidly taking the PFC “off-line” [83, 84] (Fig. 3B). α1-AR expression is also increased in the rat mPFC following TBI [22].
Under healthy conditions, feedforward cAMP-calcium signaling is regulated by post-synaptic mGluR3 and α2A-AR (Fig. 1B). These receptors are localized on layer III spines, and they inhibit cAMP-calcium opening of K+ channels, strengthening network connectivity and enhancing the dlPFC neuronal firing needed for higher cognition. mGluR3 are primarily post-synaptic in the primate dlPFC, and are not only stimulated by glutamate, but by N-acetylaspartylglutamate (NAAG), which is co-released with glutamate and is selective for mGluR3 [85, 86]. α2A-ARs are often pre-synaptic receptors, but also play a major post-synaptic role in primate dlPFC where they are concentrated on dendritic spines near HCN channels [71]. As α2A-ARs have high affinity for NE (Fig. 3A), they are engaged under nonstress conditions with moderate NE release [87]. As described below, α2A-AR stimulation can also weaken the emotional responding of the amygdala, and regulate the firing of NE neurons in the locus coeruleus (LC), thus helping to promote dlPFC top-down control (Fig. 3A). Feedforward cAMP-calcium signaling is also regulated by the phosphodiesterases (PDE4s) which catabolize cAMP and are anchored to the SER by DISC1 [77], and by the calcium binding protein, calbindin, which is expressed in the cytosol of a subset of layer III dlPFC pyramidal cells [88]. These regulatory mechanisms can restore and strengthen dlPFC function.
Neuroinflammation increases calcium-cAMP stress signaling pathways
With chronic psychological stress and/or inflammation, the regulatory pathways that would normally limit or reverse the stress response are weakened, leading to toxic calcium actions such as tau hyperphosphorylation, Aβ generation and removal of synapses (Fig. 2) [6, 89, 90]. High levels of cytosolic calcium activate calpains, which cleave and disinhibit the kinases that hyperphosphorylate tau (Fig. 2) [89]. High levels of calcium release from the SER can also cause calcium overload of mitochondria, leading to further inflammatory events, including complement signaling to microglia to remove synapses (Fig. 2) [90]. The PFC appears to be particularly vulnerable to these actions in rodents, monkeys and humans, which likely relates to its built-in mechanisms to magnify calcium and weaken synaptic connectivity.
Research in aged rhesus monkeys has already revealed at least three ways in which inflammation can dysregulate cAMP-calcium stress signaling (Fig. 2), and there are likely many more. Especially important to primate dlPFC, mGluR3 regulation of cAMP-calcium signaling is greatly reduced by inflammatory increases in glutamate carboxypeptidase II (GCPII) [91, 92], which catabolizes NAAG and thus reduces mGluR3 inhibition of cAMP signaling (Fig. 2). GCPII is synthesized and released by glia, including large increases in GCPII expression by reactive microglia under conditions of inflammation [91, 92]. Physiological studies in aged monkeys show that GCPII markedly lowers the dlPFC neuronal firing needed for higher cognition [86]. PDE4s are also lost with age in primate dlPFC [88, 93], and this may involve MK2 inflammatory signaling unanchoring PDE4 from DISC1 [94]. Finally, calbindin is normally protective against neuronal damage [95], but calbindin levels are lost with early life stress [96], COVID-19 infection [66], or advanced age;[88, 97] the loss of calbindin in the aging dlPFC is selective to layer III pyramidal cells [88], leaving them more vulnerable to calcium toxic actions and tau pathology [98]. The specific molecular mechanisms leading to calbindin loss are not currently known, but would be an important area for future research. Calcium dysregulation can in turn drive more inflammatory signaling, driving vicious cycles [90, 99]. The reduced regulation of cAMP-calcium actions would allow stress signaling to proceed unimpeded, eroding connections and neuronal firing, and building tau pathology within dendrites, increasing risk of future Alzheimer’s disease.
Examples of neuroinflammatory disorders with increased calcium-cAMP signaling
A number of neuroinflammatory conditions are associated with calcium dysregulation. For example, anesthetics such as sevoflurane can increase calcium efflux from the SER and induce tau hyperphosphorylation [100,101,102,103]. In rodent models, TBI to the posterior cortex causes increased PKA signaling in the PFC that is accompanied by loss of dendritic spines [104]. A similar profile of calcium dysregulation and spine loss is seen in rats exposed to chronic hypoxia [105], where upregulation of GCPII expression contributes to the loss of calcium regulation [106]. Elevated GCPII has been found in mouse models of a variety of disorders, including TBI, ischemia, multiple sclerosis and ALS [107,108,109,110,111,112,113]. Calcium dysregulation and tau hyperphosphorylation are also seen in rodent models of repeated head injury [114, 115], consistent with the extensive calcium toxicity and tau pathology seen in human brains with CTE [32, 116]. Finally, SARS-CoV-2 infection greatly increased cAMP-calcium signaling and tau phosphorylation in brain, and was associated with large increases in GCPII expression [66]. Thus, a constellation of elevated GCPII, calcium dysregulation, tau pathology and synapse loss is common to many neuroinflammatory conditions (Fig. 2). It should be noted that GCPII inhibitors are currently under development to treat neuroinflammatory conditions, but existing compounds have relatively poor brain penetration [86, 112, 117].
Guanfacine beneficial mechanisms
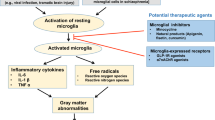
The α2A-AR agonist, guanfacine, is being used off-label and/or tested in a variety of neuroinflammatory cognitive disorders. This section describes both the direct and indirect ways that guanfacine can strengthen PFC cognition and calming effects, summarized in Fig. 4. Although many scientists and physicians are aware of α2A-AR presynaptic actions that reduce catecholamine release e.g. [118], the majority of α2A-ARs are actually post-synaptic in brain [119], including the powerful, post-synaptic effects in PFC that contribute to the calming effects of α2A-AR agonists [7, 71, 120]. Table 1 describes the affinities of commonly used α2-AR agonists for α2-AR subtypes [121, 122]. Guanfacine is the most selective α2A-AR agonist currently available (Table 1), and it is also the least sedating, likely related to its subtype selectivity [123]. In contrast, clonidine and dexmedetomidine have high affinity for all α2-AR subtypes (Table 1), and have prominent sedation. The following section reviews the biological mechanisms through which α2-AR agonists, and guanfacine in particular, may be helpful in treating the cognitive deficits of neuroinflammatory disorders. In addition to traditional presynaptic actions, guanfacine may be especially helpful by restoring regulation of cAMP-calcium-K+ signaling in the dlPFC, by weakening the amygdala, and by its anti-inflammatory actions, inhibiting the reactivity of microglia and macrophages, all of which are reviewed below.
Strengthening and protection of prefrontal cortex
As schematically illustrated in Fig. 4, guanfacine can protect and fortify dlPFC circuits by inhibiting feedforward cAMP-calcium signaling, closing nearby K+ channels to strengthen synaptic connectivity and enhance neuronal firing needed for working memory and top-down control [7]. For example, immunoelectron microscopy has demonstrated α2A-AR localized post-synaptically on layer III dendritic spines in the primate dlPFC, next to HCN channels whose open state weakens neuronal firing [71]. Local iontophoresis of guanfacine onto dlPFC neurons enhanced neuronal firing during working memory by inhibiting cAMP signaling [71], and was particularly effective in neurons with dysregulated cAMP-calcium-K+ signaling, e.g. due to advancing age [46]. Consistent with the electrophysiological results, either local infusion of guanfacine into the PFC [124,125,126], or systemic administration of guanfacine, improved a range of cognitive functions in monkeys, promoting flexible regulation of behavior, and reduced distraction and aggression [123, 127,128,129,130,131,132,133]. Systemic administration of guanfacine also increased regional cerebral blood flow in the dlPFC as monkeys performed a working memory task [134]. As the dlPFC has direct projections to the LC [135], and indirect projections to regulate the amygdala through the vmPFC [12], restoring dlPFC function may have widespread effects on top-down control.
The enhancing effects of α2A-AR stimulation can also be seen in rat medial PFC, where intraPFC infusion of an α2A-AR agonist improves working memory [126] and reduces anxiety-like behaviors [136]. Studies in rats also show that systemic guanfacine treatment protects the PFC from psychological or physiological stress exposure. Guanfacine pretreatment protects working memory performance from acute stress [137], and also protects working memory and PFC dendritic spines from chronic psychological stress [138] or chronic hypoxia [40, 105], including reducing caspase 3 levels within the PFC [105]. The protection of connections on dendritic spines may be particularly important for guanfacine’s therapeutic effects in stress-related disorders.
Weakening or regulating the amygdala and locus coeruleus to reduce anxiety/stress
Guanfacine’s calming effects also likely involve additional actions throughout the nervous and immune systems, summarized in Fig. 5. For example, guanfacine may reduce anxiety and emotional reactions by weakening the functions of the amygdala and the extended amygdala (i.e. the bed nucleus of the stria terminalis; BNST). As described above, inhibition of the amygdala may be performed in part from stronger top-down regulation by the PFC. However, there are also strong data showing that α2-AR stimulation directly within the amygdala and/or the BNST reduces fear and anxiety [139], including reduction in plasticity [140], and inhibition of stress-related inputs [141]. Mouse models also show that guanfacine can have anti-depressant like effects through actions within the amygdala [142]. As the amygdala and BNST can activate the LC to initiate a neurochemical stress response [81, 143], deactivation of the amygdala by α2-AR agonists may also have global effects in reducing the stress response.
α2-AR agonists can also have direct effects on the NE system to reduce LC neuronal firing and decrease release from noradrenergic axon terminals. The early, pioneering work of George Aghajanian showed that clonidine reduced LC firing [144]. Both clonidine [145] and guanfacine [146] have been shown to reduce stress-induced increases in catecholamine release. As these high levels of NE release simultaneously impair PFC function [78] and strengthen amygdala via α1-AR and β-AR [147, 148], reducing stress-induced catecholamine release can help to switch the brain back into a regulated state (Fig. 3; [78]). Guanfacine is weaker than clonidine in reducing LC neuronal firing and reducing NE release [149], and recent evidence indicates that chronic guanfacine treatment can actually increase NE release in cortex [150]. These data suggest that reduced NE tone may not be the cause of guanfacine’s sustained calming effects.
In summary, the degree of NE release can act as a chemical switch to determine which circuits are in control of our behavior [87]. As shown in Fig. 3A, moderate levels of NE release under nonstress conditions engage high affinity α2A-ARs to strengthen PFC and weaken amygdala, allowing extensive top-down control. In contrast, high levels of NE release during physiological or psychological stress engage low affinity α1-AR and β-AR to weaken PFC and strengthen amygdala (Fig. 3B), switching the brain into a more primitive state [78]. Thus, treatment with the α2A-AR agonist, guanfacine, can help to transition the brain back into a pattern of connectivity that allows more thoughtful, top-down regulation by the PFC. As discussed below, parallel effects may occur in the immune system, with α2-AR stimulation having an anti-inflammatory response.
Potential sedative effects through the thalamus
α2-AR agonists can produce sedation, which is a side effect when used to treat ADHD, but helpful when used as an anesthetic, e.g., dexmedetomidine [151]. While presynaptic α2A-AR actions appear to contribute to a sleep state [152], they are unlikely the whole story in primates, as the α2A-AR selective agonist, guanfacine, has little sedative actions, while the very sedating dexmedetomidine is a full agonist at the α2B-AR subtype, and only a partial agonist at the α2A-AR and the α2C-AR subtypes (Table 1) [153]. This suggests that the α2B-AR may also provide a large contribution to sedative actions, as least in primates. One possibility is that stimulation of α2B-AR in thalamus produces sedation, as stimulation of post-synaptic α2-AR actions in thalamus induce a sleep state [154], and the thalamus is enriched in α2B-AR [155, 156]. However, this hypothesis has never been actively tested. As the pattern of α2B-AR expression is more extensive in primates than in mice (www.proteinatlas.org/ENSG00000274286-ADRA2B/brain), knockout mouse models may be less useful in determining mechanisms in primates.
Analgesic actions in the spinal cord
α2-AR agonists have analgesic properties that can be helpful in many medical conditions associated with impaired cognition [157]. At least some of these analgesic actions appear to involve α2-AR stimulation in spinal cord, reducing pain pathway transmission. Descending NE pathways from the LC release NE onto both presynaptic α2-AR on C fiber terminals arising from the dorsal root ganglia, and postsynaptic α2-AR on spinal neurons to reduce the transmission of painful stimuli [158]. For example, dexmedetomidine inhibits the activity of the nociceptive receptors TRPV1 (transient receptor potential vanilloid subtype 1) [159], and the ATP purine receptor P2RX3 [160] in primary sensory neurons in the dorsal root ganglia through an α2A-AR mechanism. Pain may also be diminished through α2-AR anti-inflammatory actions [161] (and see below). It should be noted that in addition to spinal mechanisms, PFC top-down control can also reduce the response to pain [162], and thus α2A-AR actions in PFC may contribute to analgesia as well.
Anti-inflammatory properties
As schematically illustrated in Fig. 4, α2-AR agonists such as guanfacine, clonidine and dexmedetomidine can have anti-inflammatory actions. In particular, dexmedetomidine has been shown to reduce plasma measures of inflammation during surgery or sepsis [163,164,165,166]. The cellular bases for these anti-inflammatory actions are a topic of current research. Most previous research has focused on the roles of β-ARs in regulating the immune system, e.g. as reviewed in [167]. However, dexmedetomidine has been shown to reduce the secretion of the proinflammatory factor, HMGB1 (High mobility group box 1) from LPS-activated macrophages [168]. HMGB1 is a critical proinflammatory factor that has been associated with mortality in sepsis patients. Previous studies have demonstrated that dexmedetomidine can inhibit the secretion of HMGB1 in macrophages induced by lipopolysaccharide (LPS) [168]. Specifically, dexmedetomidine can prevent the translocation of HMGB1 from the nucleus to the cytoplasm and the expression of HMGB1 mRNA. These findings suggest that dexmedetomidine has anti-inflammatory effects and could potentially be used to mitigate the harmful effects of HMGB1 in sepsis. Dexmedetomidine has also been shown to inhibit LPS-induced inflammatory responses by activating PPARγ (peroxisome proliferator-activated receptor gamma) in macrophages [169]. α2A-AR agonists may also reduce inflammation in brain directly, as α2A-AR stimulation causes retraction of reactive microglia [170], which may contribute to guanfacine’s ability to protect dendritic spines from phagocytosis during chronic stress [138] or hypoxia [105]. In rodent models of TBI, dexmedetomidine was shown to reduce monocyte-derived macrophage infiltration into brain [171], and to reduce autophagy and neuroinflammation [172]. α2A-AR are also expressed by retinal ganglion cells, and basic research indicates that α2-AR stimulation in retina is neuroprotective [173]. Thus, α2A-AR agonists may protect against cell death under severe conditions, but may also protect neuronal function needed for higher cognition under more mild conditions by reducing the production of kynurenine and/or GCPII from macrophages and microglia by producing an anti-inflammatory state.
Guanfacine has beneficial actions in patients
Guanfacine, clonidine and dexmedetomidine are all in widespread clinical use, with the α2A-AR agonist guanfacine being used more prominently for nonsurgical/daytime use due to its less sedating properties. The FDA approved extended release guanfacine (Intuniv™) in 2009 for treating ADHD in children and adolescents, and its approval has been extended to adults with ADHD in Japan [174]. However, guanfacine is also used extensively off-label in a number of conditions that involve PFC dysfunction, including PTSD [175], conduct disorder [176], and autism spectrum disorders [177, 178]. Guanfacine also reduces self-injurious behavior, agitation/aggression and attention/impulse control in patients with Prader-Willi Syndrome [179], similar to its effects in monkeys [132, 180].
In addition to these conditions, guanfacine has been in experimental use, and/or being formally tested, for treating the cognitive disorders discussed in this review. Guanfacine is being used off-label to treat cognitive deficits following TBI, including evidence of enhanced PFC activity and improved working memory with guanfacine treatment [26, 181]. Guanfacine has also been shown to improve attention in patients with contralateral neglect from strokes in the right parietal association cortex [182, 183], and to improve attentional regulation in a patient following encephalomyelitis [184]. Guanfacine, in combination with N-acetylcysteine, is also being used off label to treat cognitive deficits associated with “long-COVID” [185]. It is noteworthy that both COVID-19 infection and TBI increase risk of Alzheimer’s neuropathology, and guanfacine is currently being tested as a potential add-on treatment for early AD [186].
As described above, dexmedetomidine is already in extensive use in the ICU in ventilated patients and in surgery as an anesthetic, and can help diminish delirium in vulnerable subjects [44, 163, 165, 187], including recent data using α2-AR agonists to treat delirium associated with acute COVID-19 infection [188]. However, dexmedetomidine has potent sedating effects that are problematic when the patients need to proceed to a coherent, waking state. Open label data suggest that guanfacine may be particularly useful in this regard, especially in agitated, hyperactive delirium [189,190,191], where guanfacine’s calming effects may involve many of the mechanisms described above. Intravenous and oral formulations of guanfacine are currently being tested for their effects on delirium from critical illness in large clinical trials (NCT04742673, NCT04578886).
Summary
In summary, NE stimulation of high affinity α2-ARs normally occurs under conditions of safety, when moderate levels of NE release preferentially engage α2-ARs compared to other adrenoceptors, and are able to coordinate the nervous and immune systems into a nonstressed state. Thus, medications that stimulate α2-ARs receptors may help to restore the brain and body into a healthier configuration. In particular, the ability of the α2A-AR-selective agonist, guanfacine, to restore top-down PFC regulation of behavior with minimal sedation, in addition to its anti-inflammatory properties, provides strong scientific rationale for its daily use in cognitive disorders associated with neuroinflammation.
References
Kirova AM, Bays RB, Lagalwar S. Working memory and executive function decline across normal aging, mild cognitive impairment, and Alzheimer’s disease. Biomed Res Int. 2015;2015:748212.
McDonald B, Flashman L, Saykin AJ. Executive dysfunction following traumatic brain injury: neural substrates and treatment strategies. NeuroRehabilitation. 2002;17:33–44.
Rundshagen I. Postoperative cognitive dysfunction. Dtsch Arztebl Int. 2014;111:119–25.
Szczepanski SM, Knight RT. Insights into human behavior from lesions to the prefrontal cortex. Neuron. 2014;83:1002–18.
Hellmuth J, Barnett TA, Asken BM, Kelly JD, Torres L, Stephens ML, et al. Persistent COVID-19-associated neurocognitive symptoms in non-hospitalized patients. J Neurovirol. 2021;27:191–5.
Arnsten AFT, Datta D, Wang M. The Genie in the Bottle- Magnified calcium signaling in dorsolateral prefrontal cortex. Mol Psychiatry. 2021;26:3684–3700.
Arnsten AFT. Guanfacine’s mechanism of action in treating prefrontal cortical disorders: Successful translation across species. Neurobiol Learn Mem. 2020;176:107327.
Göthert M. Role of autoreceptors in the function of the peripheral and central nervous system. Arzneimittelforschung. 1985;35:1909–16.
Goldman-Rakic PS. Circuitry of the primate prefrontal cortex and the regulation of behavior by representational memory. In: Plum F, editor. Handbook of Physiology, The Nervous System, Higher Functions of the Brain, vol. V. Bethesda MD, USA: American Physiological Society, 1987, pp 373–417.
Ongür D, Price JL. The organization of networks within the orbital and medial prefrontal cortex of rats, monkeys and humans. Cereb Cortex. 2000;10:206–19.
Wise SP. Forward frontal fields: phylogeny and fundamental function. Trends Neurosci. 2008;31:599–608.
Joyce MK, Garcia-Cabezas MA, John Y, Barbas H. Serial prefrontal pathways are positioned to balance cognition and emotion in primates. J Neurosci. 2020;40:8306–28.
Goldman-Rakic P. Cellular Basis of Working Memory. Neuron. 1995;14:477–85.
Arnsten AFT, Cools R. Neuromodulation of prefrontal cortex cognitive function in primates: The powerful roles of monoamines and acetylcholine. Neuropsychopharmacology. 2022;47:309–28.
Tsujimoto S, Genovesio A, Wise SP. Frontal pole cortex: encoding ends at the end of the endbrain. Trends Cogn Sci. 2011;15:169–76.
Wylie GR, Pra Sisto AJ, Genova HM, DeLuca J. Fatigue Across the Lifespan in Men and Women: State vs. Trait. Front Hum Neurosci. 2022;16:790006.
Aupperle RL, Allard CB, Grimes EM, Simmons AN, Flagan T, Behrooznia M, et al. Dorsolateral prefrontal cortex activation during emotional anticipation and neuropsychological performance in posttraumatic stress disorder. Arch Gen Psychiatry. 2012;69:360–71.
Sinha R, Lacadie CM, Constable RT, Seo D. Dynamic neural activity during stress signals resilient coping. Proc Natl Acad Sci USA. 2016;113:8837–42.
Holmes SE, Scheinost D, Finnema SJ, Naganawa M, Davis MT, DellaGioia N, et al. Lower synaptic density is associated with depression severity and network alterations. Nat Commun. 2019;10:1529.
Hoskison MM, Moore AN, Hu B, Orsi SA, Kobori N, Dash PK. Persistent working memory dysfunction following traumatic brain injury: evidence for a time-dependent mechanism. Neuroscience. 2009;159:483–91.
Dash PK, Johnson D, Clark J, Orsi SA, Zhang M, Zhao J, et al. Involvement of the glycogen synthase kinase-3 signaling pathway in TBI pathology and neurocognitive outcome. PLoS One. 2011;6:e24648.
Kobori N, Hu B, Dash PK. Altered adrenergic receptor signaling following traumatic brain injury contributes to working memory dysfunction. Neuroscience. 2011;172:293–302.
Kobori N, Moore AN, Dash PK. Altered regulation of protein kinase a activity in the medial prefrontal cortex of normal and brain-injured animals actively engaged in a working memory task. J Neurotrauma. 2015;32:139–48.
Inouye SK. Delirium in Older Persons. N. Engl J Med. 2006;354:1157–65.
Ylvisaker M, Feeney TJ. Executive functions after traumatic brain injury: supported cognition and self-advocacy. Semin Speech Lang. 1996;17:217–32.
McAllister TW, Flashman LA, Sparling MB, Saykin AJ. Working memory deficits after traumatic brain injury: catecholaminergic mechanisms and prospects for treatment - a review. Brain Inj. 2004;18:331–50.
Levin HS, Hanten G. Executive functions after traumatic brain injury in children. Pediatr Neurol. 2005;33:79–93.
Bohnen N, Twijnstra A, Jolles J. Performance in the Stroop color word test in relationship to the persistence of symptoms following mild head injury. Acta Neurol Scand. 1992;85:116–21.
Stein MB, Jain S, Giacino JT, Levin H, Dikmen S, Nelson LD, et al. Risk of Posttraumatic Stress Disorder and Major Depression in Civilian Patients After Mild Traumatic Brain Injury: A TRACK-TBI Study. JAMA Psychiatry. 2019;76:249–58.
Fesharaki-Zadeh A, Miyauchi JT, St Laurent-Arriot K, Tsirka SE, Bergold PJ. Increased Behavioral Deficits and Inflammation in a Mouse Model of Co-Morbid Traumatic Brain Injury and Post-Traumatic Stress Disorder. ASN Neuro. 2020;12:1759091420979567.
Stern RA, Riley DO, Daneshvar DH, Nowinski CJ, Cantu RC, McKee AC. Long-term consequences of repetitive brain trauma: chronic traumatic encephalopathy. PMR. 2011;3:S460–467.
McKee AC, Stein TD, Nowinski CJ, Stern RA, Daneshvar DH, Alvarez VE, et al. The spectrum of disease in chronic traumatic encephalopathy. Brain. 2013;136:43–64.
Moller JT, Cluitmans P, Rasmussen LS. ISPOCD investigators ISoP-OCD. Long-term postoperative cognitive dysfunction in the elderly ISPOCD1 study. Lancet. 1998;351:857–61.
Vutskits L, Xie Z. Lasting impact of general anaesthesia on the brain: mechanisms and relevance. Nat Rev Neurosci. 2016;17:705–17.
Greene NH, Attix DK, Weldon BC, Smith PJ, McDonagh DL, Monk TG. Measures of executive function and depression identify patients at risk for postoperative delirium. Anesthesiology. 2009;110:788–95.
Mashour GA, Palanca BJ, Basner M, Li D, Wang W, Blain-Moraes S, et al. Recovery of consciousness and cognition after general anesthesia in humans. Elife. 2021;10:e59525.
Baxter MG, Mincer JS, Brallier JW, Schwartz AB, Ahn H, Nir T, et al. Cognitive Recovery by Decade in Healthy 40- to 80-Year-Old Volunteers After Anesthesia Without Surgery. Anesth Analg. 2022;134:389–99.
Brownlee NNM, Wilson FC, Curran DB, Lyttle N, McCann JP. Neurocognitive outcomes in adults following cerebral hypoxia: A systematic literature review. NeuroRehabilitation. 2020;47:83–97.
Wang X, Cui L, Ji X. Cognitive impairment caused by hypoxia: from clinical evidences to molecular mechanisms. Metab Brain Dis. 2022;37:51–66.
Kauser H, Sahu S, Kumar S, Panjwani U. Guanfacine is an effective countermeasure for hypobaric hypoxia-induced cognitive decline. Neuroscience. 2013;254:110–9.
Vanderlind WM, Rabinovitz BB, Miao IY, Oberlin LE, Bueno-Castellano C, Fridman C, et al. A systematic review of neuropsychological and psychiatric sequalae of COVID-19: implications for treatment. Curr Opin Psychiatry. 2021;4:420–33.
Becker JH, Lin JJ, Doernberg M, Stone K, Navis A, Festa JR, et al. Assessment of Cognitive Function in Patients After COVID-19 Infection. JAMA Netw Open. 2021;4:e2130645.
Hampshire A, Trender W, Chamberlain SR, Jolly AE, Grant JE, Patrick F, et al. Cognitive deficits in people who have recovered from COVID-19. EClinicalMedicine. 2021;39:101044.
Hayhurst CJ, Pandharipande PP, Hughes CG. Intensive Care Unit Delirium: A Review of Diagnosis, Prevention, and Treatment. Anesthesiology. 2016;125:1229–41.
Carrarini C, Russo M, Dono F, Barbone F, Rispoli MG, Ferri L, et al. Agitation and Dementia: Prevention and Treatment Strategies in Acute and Chronic Conditions. Front Neurol. 2021;12:644317.
Wang M, Gamo NJ, Yang Y, Jin LE, Wang XJ, Laubach M, et al. Neuronal basis of age-related working memory decline. Nature. 2011;476:210–3.
Datta D, Leslie SN, Morozov YM, Duque A, Rakic P, van Dyck CH, et al. Classical complement cascade initiating C1q protein within neurons in the aged rhesus macaque dorsolateral prefrontal cortex. J Neuroinflammation. 2020;17:8.
Wang M, Yang Y, Wang CJ, Gamo NJ, Jin LE, Mazer JA, et al. NMDA receptors subserve working memory persistent neuronal firing In dorsolateral prefrontal cortex. Neuron. 2013;77:736–49.
Yang Y, Paspalas CD, Jin LE, Picciotto MR, Arnsten AFT, Wang M. Nicotinic α7 receptors enhance NMDA cognitive circuits in dorsolateral prefrontal cortex. Proc Nat Acad Sci USA. 2013;110:12078–83.
Isaac JT, Nicoll RA, Malenka RC. Evidence for silent synapses: implications for the expression of LTP. Neuron. 1995;15:427–34.
Yang ST, Wang M, Paspalas CP, Crimins JL, Altman MT, Mazer JA, et al. Core differences in synaptic signaling between primary visual and dorsolateral prefrontal cortex. Cereb Cortex. 2018;28:1458–71.
Skoblenick K, Everling S. NMDA antagonist ketamine reduces task selectivity in macaque dorsolateral prefrontal neurons and impairs performance of randomly interleaved prosaccades and antisaccades. J Neurosci. 2012;32:12018–27.
Driesen NR, McCarthy G, Bhagwagar Z, Bloch MH, Calhoun VD, D’Souza DC, et al. The impact of NMDA receptor blockade on human working memory-related prefrontal function and connectivity. Neuropsychopharmacology. 2013;38:2613–22.
Croxson PL, Kyriazis DA, Baxter MG. Cholinergic modulation of a specific memory function of prefrontal cortex. Nat Neurosci. 2011;14:1510–2.
Lim CK, Yap MM, Kent SJ, Gras G, Samah B, Batten JC, et al. Characterization of the kynurenine pathway and quinolinic Acid production in macaque macrophages. Int J Tryptophan Res. 2013;6:7–19.
Garrison AM, Parrott JM, Tuñon A, Delgado J, Redus L, O’Connor JC. Kynurenine pathway metabolic balance influences microglia activity: Targeting kynurenine monooxygenase to dampen neuroinflammation. Psychoneuroendocrinology. 2018;94:1–10.
Savitz J. The kynurenine pathway: a finger in every pie. Mol Psychiatry. 2020;25:131–47.
Fukui S, Schwarcz R, Rapoport SI, Takada Y, Smith QR. Blood-brain barrier transport of kynurenines: implications for brain synthesis and metabolism. J Neurochem. 1991;56:2007–17.
Schwarcz R, Bruno JP, Muchowski PJ, Wu HQ. Kynurenines in the mammalian brain: when physiology meets pathology. Nat Rev Neurosci. 2012;13:465–77.
Kozak R, Campbell BM, Strick CA, Horner W, Hoffmann WE, Kiss T, et al. Reduction of brain kynurenic acid improves cognitive function. J Neurosci. 2014;34:10592–602.
Kepplinger B, Baran H, Kainz A, Ferraz-Leite H, Newcombe J, Kalina P. Age-related increase of kynurenic acid in human cerebrospinal fluid - IgG and beta2-microglobulin changes. Neurosignals. 2005;14:126–35.
Thomas T, Stefanoni D, Reisz JA, Nemkov T, Bertolone L, Francis RO, et al. COVID-19 infection alters kynurenine and fatty acid metabolism, correlating with IL-6 levels and renal status. JCI Insight. 2020;5:e140327.
Cai Y, Kim DJ, Takahashi T, Broadhurst DI, Yan H, Ma S, et al. Kynurenic acid may underlie sex-specific immune responses to COVID-19. Sci Signal. 2021;14:eabf8483.
Lawler NG, Gray N, Kimhofer T, Boughton B, Gay M, Yang R, et al. Systemic Perturbations in Amine and Kynurenine Metabolism Associated with Acute SARS-CoV-2 Infection and Inflammatory Cytokine Responses. J Proteome Res. 2021;20:2796–2711.
Cysique LA, Jakabek D, Bracken SG, Allen-Davidian Y, Heng B, Chow S, et al. Post-acute COVID-19 cognitive impairment and decline uniquely associate with kynurenine pathway activation: a longitudinal observational study. medRxiv. 2022. https://doi.org/10.1101/2022.06.07.22276020.
Reiken S, Sittenfeld L, Dridi H, Liu Y, Liu X, Marks AR. Alzheimer’s-like signaling in brains of COVID-19 patients. Alzheimers Dement. 2022;18:955–65.
Adams Wilson JR, Morandi A, Girard TD, Thompson JL, Boomershine CS, Shintani AK, et al. The association of the kynurenine pathway of tryptophan metabolism with acute brain dysfunction during critical illness. Crit Care Med. 2012;40:835–41.
Forrest CM, Mackay GM, Oxford L, Millar K, Darlington LG, Higgins MJ, et al. Kynurenine metabolism predicts cognitive function in patients following cardiac bypass and thoracic surgery. J Neurochem. 2011;119:136–52.
Meier TB, Savitz J. The Kynurenine Pathway in Traumatic Brain Injury: Implications for Psychiatric Outcomes. Biol Psychiatry. 2022;91:449–58.
Yan EB, Frugier T, Lim CK, Heng B, Sundaram G, Tan M, et al. Activation of the kynurenine pathway and increased production of the excitotoxin quinolinic acid following traumatic brain injury in humans. J Neuroinflammation. 2015;12:110.
Wang M, Ramos B, Paspalas C, Shu Y, Simen A, Duque A, et al. Alpha2A-adrenoceptor stimulation strengthens working memory networks by inhibiting cAMP-HCN channel signaling in prefrontal cortex. Cell. 2007;129:397–410.
Wu J, El-Hassar L, Datta D, Thomas M, Zhang Y, David PJ, et al. Interaction Between HCN and Slack Channels Regulates mPFC Pyramidal Cell Excitability and Working Memory. bioRxiv. 2023. https://www.biorxiv.org/content/10.1101/2023.03.04.529157v1.
Arnsten AFT, Jin LE, Gamo NJ, Ramos B, Paspalas CD, Morozov Y, et al. Role of KCNQ potassium channels in stress-induced deficit of working memory. Neurobio Stress. 2019;11:100187.
Galvin VC, Yang S-T, Paspalas CD, Yang Y, Jin LE, Datta D, et al. Muscarinic M1 receptors modulate working memory performance and activity via KCNQ potassium channels in primate prefrontal cortex. Neuron. 2020;106:649–61.
Abel T, Nguyen PV, Barad M, Deuel TA, Kandel ER, Bourtchouladze R. Genetic demonstration of a role for PKA in the late phase of LTP and in hippocampus-based long-term memory. Cell. 1997;88:615–26.
Havekes R, Park AJ, Tolentino RE, Bruinenberg VM, Tudor JC, Lee Y, et al. Compartmentalized PDE4A5 Signaling Impairs Hippocampal Synaptic Plasticity and Long-Term Memory. J Neurosci. 2016;36:8936–46.
Arnsten AFT, Wang M, Paspalas CD. Neuromodulation of thought: Flexibilities and vulnerabilities in prefrontal cortical network synapses. Neuron. 2012;76:223–39.
Arnsten AFT. Stress signaling pathways that impair prefrontal cortex structure and function. Nat Rev Neurosci. 2009;10:410–22.
Datta D, Arnsten AFT. Loss of Prefrontal Cortical Higher Cognition with Uncontrollable Stress: Molecular Mechanisms, Changes with Age, and Relevance to Treatment. Brain Sci. 2019;9:113.
Finlay JM, Zigmond MJ, Abercrombie ED. Increased dopamine and norepinephrine release in medial prefrontal cortex induced by acute and chronic stress: effects of diazepam. Neuroscience. 1995;64:619–28.
Goldstein LE, Rasmusson AM, Bunney SB, Roth RH. Role of the amygdala in the coordination of behavioral, neuroendocrine and prefrontal cortical monoamine responses to psychological stress in the rat. J Neurosci. 1996;16:4787–98.
Kobori N, Clifton GL, Dash PK. Enhanced catecholamine synthesis in the prefrontal cortex after traumatic brain injury: implications for prefrontal dysfunction. J Neurotrauma. 2006;23:1094–102.
Birnbaum SB, Yuan P, Wang M, Vijayraghavan S, Bloom A, Davis D, et al. Protein kinase C overactivity impairs prefrontal cortical regulation of working memory. Science. 2004;306:882–4.
Datta D, Yang ST, Galvin VC, Solder J, Luo F, Morozov YM, et al. Noradrenergic α1-Adrenoceptor Actions in the Primate Dorsolateral Prefrontal Cortex. J Neurosci. 2019;39:2722–34.
Jin LE, Wang M, Galvin VC, Lightbourne TC, Conn PJ, Arnsten AFT, et al. mGluR2 vs. mGluR3 in Primate Prefrontal Cortex: Postsynaptic mGluR3 Strengthen Cognitive Networks. Cereb Cortex. 2018;28:974–87.
Yang S, Datta D, Woo E, Duque A, Morozov YM, Arellano J, et al. Inhibition of glutamate-carboxypeptidase-II in dorsolateral prefrontal cortex: potential therapeutic target for neuroinflammatory cognitive disorders. Mol Psychiatry. 2022:27:4252–63.
Arnsten AFT. Through the looking glass: Differential noradrenergic modulation of prefrontal cortical function. Neural Plasticity. 2000;7:133–46.
Datta D, Leslie S, Wang M, Yang S-T, Morozov Y, Mentone S, et al. Age-related calcium dysregulation linked with tau pathology and impaired cognition in non-human primates. Alzheimer’s Dement. 2021;17:920–32.
Arnsten AFT, Datta D, Del Tredici K, Braak H. Hypothesis: Tau Pathology is an Initiating Factor In Sporadic Alzheimer’s Disease. Alzheimer’s Dement. 2021;17:115–24.
Woo E, Sansing LH, Arnsten AFT, Datta D. Chronic Stress Weakens Connectivity in the Prefrontal Cortex: Architectural and Molecular Changes. Chronic Stress. 2021;5:24705470211029254.
Zhang Z, Bassam B, Thomas AG, Williams M, Liu J, Nance E, et al. Maternal inflammation leads to impaired glutamate homeostasis and up-regulation of glutamate carboxypeptidase II in activated microglia in the fetal/newborn rabbit brain. Neurobiol Dis. 2016;94:116–28.
Hollinger KR, Sharma A, Tallon C, Lovell L, Thomas AG, Zhu X, et al. Dendrimer-2PMPA selectively blocks upregulated microglial GCPII activity and improves cognition in a mouse model of multiple sclerosis. Nanotheranostics. 2022;6:126–42.
Carlyle BC, Nairn AC, Wang M, Yang Y, Jin LE, Simen AA, et al. cAMP-PKA phosphorylation of tau confers risk for degeneration in aging association cortex. Proc Natl Acad Sci USA. 2014;111:5036–41.
MacKenzie KF, Wallace DA, Hill EV, Anthony DF, Henderson DJ, Houslay DM, et al. Phosphorylation of cAMP-specific PDE4A5 (phosphodiesterase-4A5) by MK2 (MAPKAPK2) attenuates its activation through protein kinase A phosphorylation. Biochem J. 2011;435:755–69.
Guo Q, Christakos S, Robinson N, Mattson MP. Calbindin D28k blocks the proapoptotic actions of mutant presenilin 1: reduced oxidative stress and preserved mitochondrial function. Proc Natl Acad Sci USA. 1998;95:3227–32.
Li JT, Xie XM, Yu JY, Sun YX, Liao XM, Wang XX, et al. Suppressed Calbindin Levels in Hippocampal Excitatory Neurons Mediate Stress-Induced Memory Loss. Cell Rep. 2017;21:891–900.
Erraji-Benchekroun L, Underwood MD, Arango V, Galfalvy H, Pavlidis P, Smyrniotopoulos P, et al. Molecular aging in human prefrontal cortex is selective and continuous throughout adult life. Biol Psychiatry. 2005;57:549–58.
Hof PR, Morrison JH. Neocortical neuronal subpopulations labeled by a monoclonal antibody to calbindin exhibit differential vulnerability in Alzheimer’s disease. Exp Neurol. 1991;111:293–301.
Arnsten AFT, Woo E, Yang S, Wang M, Datta D. Unusual Molecular Regulation of Dorsolateral Prefrontal Cortex Layer III Synapses Increases Vulnerability to Genetic and Environmental Insults in Schizophrenia. Biol Psychiatry. 2022.
Wei H, Xie Z. Anesthesia, calcium homeostasis and Alzheimer’s disease. Curr Alzheimer Res. 2009;6:30–35.
Tao G, Zhang J, Zhang L, Dong Y, Yu B, Crosby G, et al. Sevoflurane induces tau phosphorylation and glycogen synthase kinase 3β activation in young mice. Anesthesiology. 2014;121:510–27.
Belrose JC, Noppens RR. Anesthesiology and cognitive impairment: a narrative review of current clinical literature. BMC Anesthesiol. 2019;19:241.
Dong Y, Liang F, Huang L, Fang F, Yang G, Tanzi RE, et al. The anesthetic sevoflurane induces tau trafficking from neurons to microglia. Commun Biol. 2021;4:560.
Zhao J, Huynh J, Hylin MJ, O’Malley JJ, Perez A, Moore AN, et al. Mild Traumatic Brain Injury Reduces Spine Density of Projection Neurons in the Medial Prefrontal Cortex and Impairs Extinction of Contextual Fear Memory. J Neurotrauma. 2018;35:149–56.
Kauser H, Sahu S, Panjwani U. Guanfacine promotes neuronal survival in medial prefrontal cortex under hypobaric hypoxia. Brain Res. 2016;1636:152–60.
Zhang W, Zhang Z, Wu L, Qiu Y, Lin Y. Suppression of Glutamate Carboxypeptidase II Ameliorates Neuronal Apoptosis from Ischemic Brain Injury. J Stroke Cerebrovasc Dis. 2016;25:1599–605.
Zhong C, Zhao X, Van KC, Bzdega T, Smyth A, Zhou J, et al. NAAG peptidase inhibitor increases dialysate NAAG and reduces glutamate, aspartate and GABA levels in the dorsal hippocampus following fluid percussion injury in the rat. J Neurochem. 2006;97:1015–25.
Sácha P, Zámecník J, Barinka C, Hlouchová K, Vícha A, Mlcochová P, et al. Expression of glutamate carboxypeptidase II in human brain. Neuroscience. 2007;144:1361–72.
Rahn KA, Watkins CC, Alt J, Rais R, Stathis M, Grishkan I, et al. Inhibition of glutamate carboxypeptidase II (GCPII) activity as a treatment for cognitive impairment in multiple sclerosis. Proc Natl Acad Sci USA. 2012;109:20101–6.
Cao Y, Gao Y, Xu S, Cui Z, Zhang M, Lin Y, et al. Mice lacking glutamate carboxypeptidase II develop normally, but are less susceptible to traumatic brain injury. J Neurochem. 2015;134:340–53.
Cao Y, Gao Y, Xu S, Bao J, Lin Y, Luo X, et al. Glutamate carboxypeptidase II gene knockout attenuates oxidative stress and cortical apoptosis after traumatic brain injury. BMC Neurosci. 2016;17:15.
Neale JH, Olszewski R. A role for N-acetylaspartylglutamate (NAAG) and mGluR3 in cognition. Neurobiol Learn Mem. 2019;158:9–13.
Neale JH, Yamamoto T. N-acetylaspartylglutamate (NAAG) and glutamate carboxypeptidase II: An abundant peptide neurotransmitter-enzyme system with multiple clinical applications. Prog Neurobiol. 2020;184:101722.
Wang Y, Hall RA, Lee M, Kamgar-Parsi A, Bi X, Baudry M. The tyrosine phosphatase PTPN13/FAP-1 links calpain-2, TBI and tau tyrosine phosphorylation. Sci Rep. 2017;7:11771.
Wang Y, Liu Y, Nham A, Sherbaf A, Quach D, Yahya E, et al. Calpain-2 as a therapeutic target in repeated concussion-induced neuropathy and behavioral impairment. Sci Adv. 2020;6:eaba5547.
Siman R, Giovannone N, Hanten G, Wilde EA, McCauley SR, Hunter JV, et al. Evidence That the Blood Biomarker SNTF Predicts Brain Imaging Changes and Persistent Cognitive Dysfunction in Mild TBI Patients. Front Neurol. 2013;4:190.
Vornov JJ, Hollinger KR, Jackson PF, Wozniak KM, Farah MH, Majer P, et al. Still NAAG’ing After All These Years: The Continuing Pursuit of GCPII Inhibitors. Adv Pharm. 2016;76:215–55.
Urban R, Szabo B, Starke K. Involvement of peripheral presynaptic inhibition in the reduction of sympathetic tone by moxonidine, rilmenidine and UK 14304. Eur J Pharm. 1995;282:29–37.
U’Prichard DC, Bechtel WD, Rouot BM, Snyder SH. Multiple apparent alpha-noradrenergic receptor binding sites in rat brain: effect of 6-hydroxydopamine. Mol Pharm. 1979;16:47–60.
Arnsten AFT, Goldman-Rakic PS. Alpha-2 adrenergic mechanisms in prefrontal cortex associated with cognitive decline in aged nonhuman primates. Science. 1985;230:1273–6.
Uhlen S, Wikberg JES. Delineation of rat kidney alpha 2A and alpha 2B-adrenoceptors with [3H]RX821002 radioligand binding: computer modeling reveals that guanfacine is an alpha-2A-selective compound. Eur J Pharm. 1991;202:235–43.
Uhlen S, Xia Y, Chhajlani V, Felder CC, Wikberg JES. [3H]MK912 binding delineates 2 a-2-adrenoceptor subtypes in rat CNS one of which is identical with the cloned pA2d a-2- adrenoceptor. Br J Pharm. 1992;106:986–95.
Arnsten AFT, Cai JX, Goldman-Rakic PS. The alpha-2 adrenergic agonist guanfacine improves memory in aged monkeys without sedative or hypotensive side effects. J Neurosci. 1988;8:4287–98.
Mao Z-M, Arnsten AFT, Li B-M. Local infusion of alpha-1 adrenergic agonist into the prefrontal cortex impairs spatial working memory performance in monkeys. Biol Psychiatry. 1999;46:1259–65.
Wang M, Tang ZX, Li BM. Enhanced visuomotor associative learning following stimulation of alpha 2A-adrenoceptors in the ventral prefrontal cortex in monkeys. Brain Res. 2004;1024:176–82.
Ramos B, Stark D, Verduzco L, van Dyck CH, Arnsten AFT. Alpha-2A-adrenoceptor stimulation improves prefrontal cortical regulation of behavior through inhibition of cAMP signaling in aging animals. Learn Mem. 2006;13:770–6.
Arnsten AFT, Contant TA. Alpha-2 adrenergic agonists decrease distractability in aged monkeys performing a delayed response task. Psychopharmacology. 1992;108:159–69.
Arnsten AFT, Steere JC, Hunt RD. The contribution of alpha-2 noradrenergic mechanisms to prefrontal cortical cognitive function: potential significance to Attention Deficit Hyperactivity Disorder. Arch Gen Psychiatry. 1996;53:448–55.
Steere JC, Arnsten AFT. The alpha-2A noradrenergic agonist, guanfacine, improves visual object discrimination reversal performance in rhesus monkeys. Behav Neurosci. 1997;111:1–9.
Franowicz JCS, Arnsten AFT. The alpha-2A noradrenergic agonist, guanfacine, improves delayed response performance in young adult rhesus monkeys. Psychopharmacology. 1998;136:8–14.
O’Neill J, Fitten LJ, Siembieda DW, Ortiz F, Halgren E. Effects of guanfacine on three forms of distraction in the aging macaque. Life Sci. 2000;67:877–85.
Macy JDJ, Beattie TA, Morgenstern SE, Arnsten AF. Use of guanfacine to control self-injurious behavior in two rhesus macaques (Macaca mulatta) and one baboon (Papio anubis). Comp Med. 2000;50:419–25.
Wang M, Ji JZ, Li BM. The alpha(2A)-adrenergic agonist guanfacine improves visuomotor associative learning in monkeys. Neuropsychopharmacology. 2004;29:86–92.
Avery RA, Franowicz JS, Studholme C, van Dyck CH, Arnsten AFT. The alpha-2A-adenoceptor agonist, guanfacine, increases regional cerebral blood flow in dorsolateral prefrontal cortex of monkeys performing a spatial working memory task. Neuropsychopharmacology. 2000;23:240–9.
Arnsten AFT, Goldman-Rakic PS. Selective prefrontal cortical projections to the region of the locus coeruleus and raphe nuclei in the rhesus monkey. Brain Res. 1984;306:9–18.
Wu Z, Wang T, Li L, Hui Y, Zhang Q, Yuan H. Activation and blockade of α2-adrenoceptors in the prelimbic cortex regulate anxiety-like behaviors in hemiparkinsonian rats. Biochem Biophys Res Commun. 2019;519:697–704.
Birnbaum SG, Podell DM, Arnsten AFT. Noradrenergic alpha-2 receptor agonists reverse working memory deficits induced by the anxiogenic drug, FG7142, in rats. Pharm Biochem Behav. 2000;67:397–403.
Hains AB, Yabe Y, Arnsten AFT. Chronic stimulation of alpha-2A-adrenoceptors with guanfacine protects rodent prefrontal cortex dendritic spines and cognition from the effects of chronic stress. Neurobiol Stress. 2015;2:1–9.
Schweimer J, Fendt M, Schnitzler HU. Effects of clonidine injections into the bed nucleus of the stria terminalis on fear and anxiety behavior in rats. Eur J Pharm. 2005;507:117–24.
DeBock F, Kurz J, Azad SC, Parsons CG, Hapfelmeier G, Zieglgansberger W, et al. Alpha2-adrenoreceptor activation inhibits LTP and LTD in the basolateral amygdala: involvement of Gi/o-protein-mediated modulation of Ca2+-channels and inwardly rectifying K+-channels in LTD. Eur J Neurosci. 2003;17:1411–24.
Flavin SA, Matthews RT, Wang Q, Muly EC, Winder DG. α(2A)-adrenergic receptors filter parabrachial inputs to the bed nucleus of the stria terminalis. J Neurosci. 2014;34:9319–31.
Mineur YS, Cahuzac EL, Mose TN, Bentham MP, Plantenga ME, Thompson DC, et al. Interaction between noradrenergic and cholinergic signaling in amygdala regulates anxiety- and depression-related behaviors in mice. Neuropsychopharmacology. 2018;43:2118–25.
Valentino RJ, Curtis AL, Page ME, Pavcovich LA, Florin-Lechner SM. Activation of the locus coeruleus brain noradrenergic system during stress: Circuitry, consequences, and regulation. Adv Pharm. 1998;42:781–4.
Cedarbaum JM, Aghajanian GK. Catecholamine receptors on locus coeruleus neurons: pharmacological characterization. Eur J Pharm. 1977;44:375–85.
Ida Y, Elsworth J, Roth RH. Anxiogenic beta carboline FG7142 produces activation of NE neurons in specific brain regions of rats. Pharm Biochem Behav. 1991;39:791–3.
Morrow BA, George TP, Roth RH. Noradrenergic alpha-2 agonists have anxiolytic-like actions on stress-related behavior and mesoprefrontal dopamine biochemistry. Brain Res. 2004;1027:173–8.
Phelps EA, LeDoux JE. Contributions of the amygdala to emotion processing: from animal models to human behavior. Neuron. 2005;48:175–87.
Roozendaal B, McGaugh JL. Memory modulation. Behav Neurosci. 2011;125:797–824.
Engberg G, Eriksson E. Effects of alpha-2-adrenoceptor agonists on locus coeruleus firing rate and brain noradrenaline turnover in EEDQ-treated rats. Naunyn-Schmiedebergs Arch Pharm. 1991;343:472–7.
Fukuyama K, Nakano T, Shiroyama T, Okada M. Chronic Administrations of Guanfacine on Mesocortical Catecholaminergic and Thalamocortical Glutamatergic Transmissions. Int J Mol Sci. 2021;22:4122.
Ballesteros JJ, Briscoe JB, Ishizawa Y. Neural signatures of α2-Adrenergic agonist-induced unconsciousness and awakening by antagonist. Elife. 2020;9:e57670.
Nelson LE, Lu J, Guo T, Saper CB, Franks NP, Maze M. The alpha2-adrenoceptor agonist dexmedetomidine converges on an endogenous sleep-promoting pathway to exert its sedative effects. Anesthesiology. 2003;98:428–36.
Jansson CC, Pohjanoksa K, Lang J, Wurster S, Savola JM, Scheinin M. Alpha2-adrenoceptor agonists stimulate high-affinity GTPase activity in a receptor subtype-selective manner. Eur J Pharm. 1999;374:137–46.
Buzsaki G, Kennedy B, Solt VB, Ziegler M. Noradrenergic control of thalamic oscillation: The role of alpha-2 receptors. Eur J Neuro. 1991;3:222–9.
Nicholas AP, Pieribone V, Hökfelt T. Distributions of mRNAs for alpha-2 adrenergic receptor subtypes in rat brain: an in situ hybridization study. J Comp Neurol. 1993;328:575–94.
MacDonald E, Scheinin M. Distribution and pharmacology of alpha 2-adrenoceptors in the central nervous system. J Physiol Pharm. 1995;46:241–58.
Zhao Y, He J, Yu N, Jia C, Wang S. Mechanisms of Dexmedetomidine in Neuropathic Pain. Front Neurosci. 2020;14:330.
Bahari Z, Meftahi GH. Spinal α2 -adrenoceptors and neuropathic pain modulation; therapeutic target. Br J Pharm. 2019;176:2366–81.
Lee BM, Jang Y, Park G, Kim K, Oh SH, Shin TJ, et al. Dexmedetomidine modulates transient receptor potential vanilloid subtype 1. Biochem Biophys Res Commun. 2020;522:832–7.
Hao JW, Qiao WL, Li Q, Wei S, Liu TT, Qiu CY, et al. Suppression of P2X3 receptor-mediated currents by the activation of α2A -adrenergic receptors in rat dorsal root ganglion neurons. CNS Neurosci Ther. 2022;28:289–97.
Farghaly HS, Mahmoud AM, Abdel-Sater KA. Effect of dexmedetomidine and cold stress in a rat model of neuropathic pain: Role of interleukin-6 and tumor necrosis factor-α. Eur J Pharm. 2016;776:139–45.
Kummer KK, Mitrić M, Kalpachidou T, Kress M. The Medial Prefrontal Cortex as a Central Hub for Mental Comorbidities Associated with Chronic Pain. Int J Mol Sci. 2020;21:3440.
Zhang W, Wang TJ, Wang G, Yang M, Zhou Y, Yuan Y. Effects of Dexmedetomidine on Postoperative Delirium and Expression of IL-1β, IL-6, and TNF-α in Elderly Patients After Hip Fracture Operation. Front Pharm. 2020;11:678.
Chen R, Kang Z, Wang Y, Zhao J, Li S. The Anti-inflammatory Effect of Dexmedetomidine Administration on Patients Undergoing Intestinal Surgery: A Randomized Study. Drugs R D. 2021;21:445–53.
Lankadeva YR, Shehabi Y, Deane AM, Plummer MP, Bellomo R, May CN. Emerging benefits and drawbacks of α2 -adrenoceptor agonists in the management of sepsis and critical illness. Br J Pharm. 2021;178:1407–25.
Ding M, Xu X, Xia L, Cao Y. Magnetic Resonance Imaging Characteristic Evaluation of Dexmedetomidine on Neurocognitive Dysfunction in Elderly Patients with Colorectal Tumors after Laparoscopic Operation. Comput Math Methods Med. 2022;2022:1345695.
Scanzano A, Cosentino M. Adrenergic regulation of innate immunity: a review. Front Pharm. 2015;6:171.
Chang Y, Huang X, Liu Z, Han G, Huang L, Xiong YC, et al. Dexmedetomidine inhibits the secretion of high mobility group box 1 from lipopolysaccharide-activated macrophages in vitro. J Surg Res. 2013;181:308–14.
Fujimoto M, Higuchi H, Honda-Wakasugi Y, Miyake S, Nishioka Y, Yabuki-Kawase A, et al. Dexmedetomidine inhibits LPS-induced inflammatory responses through peroxisome proliferator-activated receptor gamma (PPARγ) activation following binding to α2 adrenoceptors. Eur J Pharm. 2021;892:173733.
Gyoneva S, Traynelis SF. Norepinephrine modulates the motility of resting and activated microglia via different adrenergic receptors. J Biol Chem. 2013;288:15291–302.
Kii N, Sawada A, Yoshikawa Y, Tachibana S, Yamakage M. Dexmedetomidine Ameliorates Perioperative Neurocognitive Disorders by Suppressing Monocyte-Derived Macrophages in Mice With Preexisting Traumatic Brain Injury. Anesth Analg. 2022;134:869–80.
Feng X, Ma W, Zhu J, Jiao W, Wang Y. Dexmedetomidine alleviates early brain injury following traumatic brain injury by inhibiting autophagy and neuroinflammation through the ROS/Nrf2 signaling pathway. Mol Med Rep. 2021;24:661.
Ruan Y, Böhmer T, Jiang S, Gericke A. The role of adrenoceptors in the retina. Cells. 2020;9:2594.
Ota T, Yamamuro K, Okazaki K, Kishimoto T. Evaluating Guanfacine Hydrochloride in the Treatment of Attention Deficit Hyperactivity Disorder (ADHD) in Adult Patients: Design, Development and Place in Therapy. Drug Des Devel Ther. 2021;15:1965–9.
Connor DF, Grasso DJ, Slivinsky MD, Pearson GS, Banga A. An open-label study of guanfacine extended release for traumatic stress related symptoms in children and adolescents. J Child Adolesc Psychopharmacol. 2013;23:244–51.
Connor DF, Findling RL, Kollins SH, Sallee F, López FA, Lyne A, et al. Effects of guanfacine extended release on oppositional symptoms in children aged 6-12 years with attention-deficit hyperactivity disorder and oppositional symptoms: a randomized, double-blind, placebo-controlled trial. CNS Drugs. 2010;24:755–68.
McCracken JT, Aman MG, McDougle CJ, Tierney E, Shiraga S, Whelan F, et al. Possible influence of variant of the P-glycoprotein gene (MDR1/ABCB1) on clinical response to guanfacine in children with pervasive developmental disorders and hyperactivity. J Child Adolesc Psychopharmacol. 2010;20:1–5. PMCID: PMC2835389
Politte LC, Scahill L, Figueroa J, McCracken JT, King B, McDougle CJ. A randomized, placebo-controlled trial of extended-release guanfacine in children with autism spectrum disorder and ADHD symptoms: an analysis of secondary outcome measures. Neuropsychopharmacology. 2018;43:1772–8.
Singh D, Wakimoto Y, Filangieri C, Pinkhasov A, Angulo M. Guanfacine Extended Release for the Reduction of Aggression, Attention-Deficit/Hyperactivity Disorder Symptoms, and Self-Injurious Behavior in Prader-Willi Syndrome-A Retrospective Cohort Study. J Child Adolesc Psychopharmacol. 2019;29:313–7.
Freeman ZT, Rice KA, Soto PL, Pate KA, Weed MR, Ator NA, et al. Neurocognitive dysfunction and pharmacological intervention using guanfacine in a rhesus macaque model of self-injurious behavior. Transl Psychiatry. 2015;5:e567.
McAllister TW, McDonald BC, Flashman LA, Ferrell RB, Tosteson TD, Yanofsky NN, et al. Alpha-2 adrenergic challenge with guanfacine one month after mild traumatic brain injury: Altered working memory and BOLD response. Int J Psychophysiol. 2011;82:107–14.
Malhotra PA, Parton AD, Greenwood R, Husain M. Noradrenergic modulation of space exploration in visual neglect. Ann Neurol. 2006;59:186–90.
Dalmaijer ES, Li KMS, Gorgoraptis N, Leff AP, Cohen DL, Parton AD, et al. Randomised, double-blind, placebo-controlled crossover study of single-dose guanfacine in unilateral neglect following stroke. J Neurol Neurosurg Psychiatry. 2018;89:593–8.
Singh-Curry V, Malhotra P, Farmer SF, Husain M. Attention deficits following ADEM ameliorated by guanfacine. J Neurol Neurosurg Psychiatry. 2011;82:688–90.
Fesharaki-Zadeh A, Lowe N, Arnsten AFT. Clinical experience with the α2A-adrenoceptor agonist, guanfacine, and N-acetylcysteine for the treatment of cognitive deficits in “Long-COVID19”. Neuroimmunol Rep. 2023;3:100154.
Hoang K, Watt H, Golemme M, Perry RJ, Ritchie C, Wilson D, et al. Noradrenergic Add-on Therapy with Extended-Release Guanfacine in Alzheimer’s Disease (NorAD): study protocol for a randomised clinical trial and COVID-19 amendments. Trials. 2022;23:623.
Pandharipande PP, Pun BT, Herr DL, Maze M, Girard TD, Miller RR, et al. Effect of sedation with dexmedetomidine vs lorazepam on acute brain dysfunction in mechanically ventilated patients: the MENDS randomized controlled trial. JAMA. 2007;298:2644–53.
Bauer SC, Moral F, Preloger E, Spindler A, Roman M, Logan A, et al. Pediatric COVID-19 Delirium: Case Report of 2 Adolescents. WMJ. 2021;120:131–6.
Srour H, Pandya K, Flannery A, Hatton K. Enteral Guanfacine to Treat Severe Anxiety and Agitation Complicating Critical Care After Cardiac Surgery. Semin Cardiothorac Vasc Anesth. 2018;22:403–6.
Sher Y, Rabkin B, Maldonado JR, Mohabir P. COVID-19-Associated Hyperactive Intensive Care Unit Delirium With Proposed Pathophysiology and Treatment: A Case Report. Psychosomatics. 2020;61:544–50.
Jiang S, Czuma R, Cohen-Oram A, Hartney K, Stern TA. Guanfacine for Hyperactive Delirium: A Case Series. J Acad Consult Liaison Psychiatry. 2021;62:83–88.
Acknowledgements
AFTA is supported by R01AG061190; ZX is supported by R01AG062509 and R01AG041274.
Author information
Authors and Affiliations
Contributions
All authors contributed to the writing of this manuscript. AFTA is an expert on the molecular regulation of prefrontal cortex, while YI and ZX are experts on inflammation and anesthesia.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Arnsten, A.F.T., Ishizawa, Y. & Xie, Z. Scientific rationale for the use of α2A-adrenoceptor agonists in treating neuroinflammatory cognitive disorders. Mol Psychiatry 28, 4540–4552 (2023). https://doi.org/10.1038/s41380-023-02057-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41380-023-02057-4