Abstract
Erectile dysfunction (ED), the second most common male sexual disorder, has an important impact on man sexuality and quality of life affecting also female partner’s sexual life. ED is usually related to cardiovascular disease or is an iatrogenic cause of pelvic surgery. Many non-surgical treatments have been developed with results that are controversial, while surgical treatment has reached high levels of satisfaction. The aim is to evaluate outcomes and complications related to prosthesis implant in patients suffering from ED not responding to conventional medical therapy or reporting side effects with such a therapy. One hundred eighty Caucasian male suffering from ED were selected. The patient population were divided into two groups: 84 patients with diabetes and metabolic syndrome (group A) and 96 patients with dysfunction following laparoscopic radical prostatectomy for prostate cancer (group B). All subjects underwent primary inflatable penile prosthesis implant with an infrapubic minimally invasive approach. During 12 months of follow-up, we reported 3 (1.67%) explants for infection, 1 (0.56%) urethral erosion, 1 (0.56%) prosthesis extrusion while no intraoperative complications were reported. Mean International Index of Erectile Function-5 (IIEF-5) was 8.2±4.0 and after the surgery (12 months later) was 20.6±2.7. The improvement after the implant is significant in both groups without a statistically significant difference between the two groups (P-value 0.65). Mean Erectile Dysfunction Inventory of Treatment Satisfaction (EDITS) score 1 year after the implant is 72.2±20.7, and there was no statistically significant difference between groups A and B (P-value 0.55). Implantation of an inflatable prosthesis, for treatment of ED, is a safe and efficacious approach; and the patient and partner satisfaction is very high. Surgical technique should be minimally invasive and latest technology equipment should be implanted in order to decrease after surgery common complications (infection and mechanical failure).
Similar content being viewed by others
Introduction
After premature ejaculation, erectile dysfunction (ED) is the most common male sexual disorder.1 ED is described as persistent inability to obtain and maintain an erection sufficient to permit satisfactory sexual performance. It is associated with age and has an incidence between 2–28.9% in the age group from 30 to 39 and 41.9–83% in the age group from 70 to 80.2 ED has an important impact on man sexuality and quality of life (QoL), but also affect female partner’s sexual life.3
ED’s main risk factors are related to cardiovascular disease and specifically have been found to be sedentary lifestyle, obesity, smoking, hypercholesterolemia, metabolic syndrome and diabetes.4 Besides medical comorbidity, one of the main causes of ED is iatrogenesis following pelvic surgery. Radical prostatectomy, even when a bilateral nerve-sparing technique is applied, is connected with an incidence of ED of up to 44%.5, 6 In cases not suitable for a nerve-sparing procedure, sexual potency is preserved in only 0–17% of patients.7
To date, many non-surgical treatments have been developed with results that are controversial. When first-line pharmaceuticals such as phosphodiesterase type 5 (PDE5) inhibitors fail, intracavernous injection (ICI), vacuum devices or intraurethral alprostadil are options considered. Medical therapy can help in improving QoL and erectile function, but unfortunately the literature describes a drop-out rate of up to 80%.8, 9 Surgical treatment, usually performed after the failure of medical therapy, has reached high levels of satisfaction albeit at the cost of undergoing surgery. Inflatable penile prostheses (IPP) implant, although invasive, is associated with better sexual function, perception and with patient and partner’s high satisfaction.10, 11 Penile prosthesis implantation can lead to complications that require prosthesis repair, explants or replacement. Fluid leak from the device, supersonic transport deformity, cylinder’s aneurismal dilatation and extrusion are reported as the most common mechanical failures.12 On the other hand, infections remain the most common and serious surgical complications with the risk of further penile shortening, urethral injury with erosion and tissue loss.13, 14 Patients affected by diabetes, immunosuppression or spinal cord injury are at increased risk of infectious complications.15 In the case of prosthesis failure, in order to avoid infectious risk, it has been suggested to perform a complete replacement of the equipment.12 Infectious mechanisms have been well studied, and are characterized by bacterial implantation on the surface of the device creating a biofilm that avoid the immune system and antibiotics to exert their effect.16 At this time cylinders, pump and tubing of the three-piece IPP are impregnated with antibiotics (rifampicin and minocycline), which have been associated with the reduction in postoperative infections.17
The aim of the study is to report outcomes of prosthesis implant in patients suffering from ED not responding to conventional medical therapy or reporting side effects with such a therapy. We investigate intraoperative and postoperative complications with infrapubic inflatable prosthesis implantation. As a secondary outcome, patient satisfaction and erectile function are reported.
Materials and methods
This was a single-center study conducted from June 2011 to December 2013 on 180 Caucasian male patients with a median age of 64.7 years suffering from ED. The patient population, divided into two groups, included 84 patients with diabetes and metabolic syndrome (group A) and 96 patients with dysfunction following video-assisted laparoscopic radical prostatectomy (VLRP) for prostate cancer (group B). Twelve of the group B suffered from diabetes or metabolic syndrome. All radical prostatectomies have been performed in the same hospital by the same surgeon using the same laparoscopic technique. All patients included in the study underwent a non-nerve sparing procedure because of their oncologic status. Both groups, before surgery, were treated with oral therapy, ICI or vacuum device. Our institute prescribes oral therapy to men undergoing prostatectomy, even in non-nerve sparing cases, to avoid penile deformities and penile smooth muscle fibrosis.18 All subjects underwent primary penile prosthesis implant and all the procedures had been carried out at Department of Urological Sciences of Sapienza Rome University by a single surgeon. The prostheses were either the AMS 700 CX (AMS, Minnetonka, MN, USA) or the Coloplast Titan OTR (Coloplast Corporation, Minneapolis, MN, USA) with controlled expansion cylinders optimize girth.19 The AMS prostheses are connected with an AMS Conceal low profile reservoir coated with parylene, and are characterized by Momentary Squeeze pump with one-touch button designed for easy deflation and lock-out valve designed to resist auto-inflation; InhibiZone (AMS, Minnetonka, MN, USA) antibiotic treatment (minocycline and rifampicin) creates a zone of inhibition effective against the bacteria commonly associated with inflatable prosthesis infections. The Coloplast prostheses are connected with Coloplast Titan CL reservoir with a four-leaf clover shape, and are characterized by lock-out safety valve (Coloplast, Minneapolis, MN, USA) designed to prevent auto-inflation and One Touch Release (OTR) for easy deflation of the device; hydrophilic coating decreases infection risk.
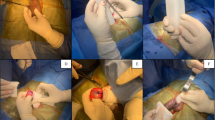
The implants were performed by a minimally invasive technique and, after the patient was shaved, the skin pepped for 10 min with a poviodone-iodine solution and intravenous cefazolin was administered. The first step is induction of an artificial erection that allows to identify any pathology needing correction, verifies 'true' dilation of the corpora supplanting serial dilations and facilitates the identification of the dorsal nerve and lateral placement of stay sutures. An infrapubic 3 cm skin incision followed by 1.5 cm bilateral corporotomy incision is applied (Figure 1). Using the Furlow, the proximal and distal corpora cavernosa are measured and dilated (Figure 2). We place color-coded stay sutures in the corpora, lateral to the dorsal nerve and using a 3½ inch nasal speculum created a space for the reservoir (filled with 100 ml of saline solution), posterior to transversalis fascia in cephalad to caudal position (Figure 3). After exposure, cylinders are placed using stay sutures for retraction and functional/cosmetic result is checked by rapidly inflating the prosthesis (Figure 4). Once again, the nasal speculum is utilized, this time, to develop the subdartos pouch into dependant portion of scrotum. After performing the hydraulic test (Figure 5), we finally close the corporotomies using the stay suture previously placed. We then connected the appropriate tubing and as standard of our care a Jackson-Pratt drain is placed in dependent portion of scrotum and skin incision closed with subcuticular sutures.20 On average, the size of the cylinders of group B patients was slightly shorter than group A; this shortening is likely due to the hypoxia and the following fibrosis that occurs in the corpora of patients submitted to radical prostatectomy. Usually we keep the prosthesis 80% activated for 72 h in order to avoid contraction. Following the implant regular follow-up controls were scheduled; the first activation of the prosthesis is applied 8–10 days after the implantation and the patient starts sexual intercourse after 6 weeks. After surgery, 10 days of cefazolin and a single dose of gentamycin are administered.
Preoperative, intraoperative and postoperative data were analyzed with a follow-up period of 12 months. Preimplant data collected were age, marital status, etiology of ED, time from ED onset to prosthesis placement and previous ED treatments. Intraoperative data included complications and postoperative data included complications and ED outcomes. Postoperative ED was evaluated using the validated, self-administered International Index of Erectile Function-5 (IIEF-5) that is based on five questions about erectile function, with a score ranging between 5 and 25, and Erectile Dysfunction Inventory of Treatment Satisfaction (EDITS) that is based on 16 items about erectile function and sexual intercourse satisfaction after the treatment, divided into 11 questions for the patient and 5 for the partner, with a score ranging between 0 and 100.
The study protocol was approved by our internal ethics committee and the committee for human subjects research (Sapienza Rome University, Department of Gynecological-Obstetric Sciences and Urological Sciences, Ethical Committee). All treatments applied are part of routine standard care, and the study was conducted in line with European Urology and Good Clinical Practice guidelines, with ethical principles laid down in the latest version of the Declaration of Helsinki. Every patient has been informed and signed consent to participate in the study.
Statistical analysis was performed with BMDP statistical software, version 7 (Statistical Solutions, Saugus, MA, USA) and SPSS (Chicago, IL, USA, version 15.00 for Windows). Statistical significance was achieved, if the P-value was <0.05. All reported P-values are one-tailed.
Results
A total of 180 patients underwent IPP implantation and were enrolled in the study. The surgical procedure was the same and carried out by the same surgeon, two different kinds of equipment were implanted. All the patients accepted to participate in the study and signed informed consent. The median age was 64.7 years (52–69), and 144 patients (80%) were married while 36 were single (20%). The etiology of ED was divided between 84 patients (46.67%) affected by diabetes mellitus and metabolic syndrome and 96 patients (53.33%) with ED following non-nerve sparing radical prostatectomy. Mean duration of ED before implant was respectively 24.5±18.6 months for VLRP patients and 74.5±50.1 months for diabetic patients and the difference between the two groups is statistically significant (P<0.005). Regarding previous ED treatments are as follows: oral therapy in 60 patients (71.43%) for group A and 72 (75%) for group B without a statistically significant difference; ICI in 42 patients (50%) of group A and 84 (87.5%) of group B with a statistically significant difference; vacuum device in 18 patients (21.43%) of group A and 30 (31.25%) of group B without a statistically significant difference. Zero patients had no previous treatment. The success rate of groups A and B was 44% (37 pts) and 8.3% (8 pts), respectively to oral therapy, 77.3% (65 pts) and 67.7% to ICI (65 pts) and 63% (53 pts) and 43.7% (42 pts) to vacuum device.
There were no reported intraoperative complications and the median time to complete the implant was 39 min (26–74).
During 12 months of follow-up, we reported 3 (1.67%) explants for infection, 1 (0.56%) urethral erosion and 1 (0.56%) prosthesis extrusion. During the day after the surgery, 12 cases (6.67%) of scrotal hematoma were reported (Table 1). The drain was removed the day after the procedure in 144 cases (80%) and 2 days after in 36 cases (20%). All the patients were discharged the day after the surgery.
To evaluate post-surgical results, two validated questionnaires were used: IIEF-5 and EDITS (Table 1).
Mean IIEF-5 was 8.2±4.0 and after the surgery (12 months later) was 20.6±2.7. The improvement after the implant is significant in both groups without a statistically significant difference between the two groups (P-value 0.65).
Mean EDITS score 1 year after the implant is 72.2±20.7, and there was no statistically significant difference between groups A and B (P-value 0.55). Stratifying cases by there score (0–20: very unsatisfied, 21–40: moderately unsatisfied, 41–60: moderately satisfied, 61–80: very satisfied and 81–100 completely satisfied) showed that 12 patients were moderately unsatisfied, 48 were moderately satisfied, 108 were very satisfied and 12 were completely satisfied (Table 2).
Discussion
ED, a common cause of impaired QoL, can be a result of a vascular or neurogenic insult that can be both organic and iatrogenic in nature. Radical prostatectomy, the most prevalent cause of erectile function impairment, depending on surgical technique (nerve-sparing or non-nerve sparing), has an impotence rate of 40–100%.5, 6, 21 Neurovascular bundle dissection or damage causes neuro-apraxia that can last up to 18 months, leading in some cases to lacunar fibrosis and ultimately a decline in erectile function.22, 23 PDE5 inhibitors are first-line treatment for ED and have demonstrated efficacy, ease of use, good tolerability, excellent safety and positive impact on QoL. Even though PDE5i are indicated in all causes of ED, post-RP patients can be poor responders to these drugs. In particular, the efficacy is reported only with whom underwent a nerve-sparing procedure, and sildenafil is the most efficacious molecule at this regard. The rationale of high-dose sildenafil after RP is the preservation of smooth muscle within the corpora cavernosa with a better return to spontaneous normal erectile function.24 The response rate to sildenafil treatment for ED after RP in different trials ranges from 35% to 75% among those who underwent nerve-sparing radical prostatectomy and from 0% to 15% among those who underwent non-nerve sparing technique.25, 26 Furthermore, a discontinuation rate of 53%, mainly due to efficacy below expectation, is reported by Jiann et al.27
Patients not responding to oral therapy may be offered ICIs, and prostaglandin E1 (alprostadil) is the most common drug; different formulations include Bimix (papaverine and phentolamine) and Trimix (alprostadil, papaverine and phentolamine). ICI is associated with high efficacy rates in the general ED populations (>70%) as well as good intercourse satisfaction, ranging from 87% to 93.5% for the patient and from 86% to 90.3% for the partner.28, 29 Even for ICI, high discontinuation rate exists up to 67% of the time and is due to side effects (pain, prolonged erection, priapism and fibrosis) and discomfort related to medically induced sexual function.30 Vacuum devices, as a second-line therapy choice, are characterized by optimal efficacy as high as 90% regardless of the cause of ED, with a satisfaction rate ranging between 27 and 94%.31 Discontinuation rate is still high, and is up to 64% with most common side effects being inability to ejaculate, petechiae, skin necrosis, bruising and numbness.32, 33
In patients not responding to first- and second-line therapy, dissatisfied with their side effects or that prefers a permanent solution, penile prosthesis implant may be considered. IPPs are characterized by improved flaccidity and rigidity, and are usually preferred by patients because of the more 'natural' erection obtained.34, 35 To evaluate after surgery results usually self-administered questionnaire are used; in particular, IIEF and EDITS are the most common.36 Patients overall satisfaction rate after an implant is high and is better with three-piece devices in comparison with two-piece ones: 97 and 81%, respectively.37 Mulhall et al.36 reported, after implant, an improvement in IIEF and EDITS that continue to increase even after 3 months till up to 9–12 months. In a meta-analysis, Bernal and Henry38 analyzed 20 years of literature and reached the conclusion that despite the variability of used methods and lack of approved questionnaire, patients are satisfied with the implant and with the subsequent sexual activity. Even partners are reported satisfied and Moskovic et al.39 in their paper conclude that male satisfaction correlates positively with female satisfaction, while unsatisfied men have a relation with female suffering from sexual activity quality. Comparing patients with different ED origins, Akin-Olugbade et al.40 reported an IIEF before implant that was different between patients that underwent a radical prostatectomy compared with organic ED, while after the surgery the IIEF score is comparable between the two groups.
Complications related to penile prosthesis implant are nowadays reported less than 5% of the time and is in part due to standardization of surgical technique and improvements in the device. Risk of infection is reported to be between 1.7 and 1.8% with an antibiotic prophylaxis against Gram-positive and Gram-negative bacteria and with the usage of antibiotic impregnated or hydrophilic-coated prosthesis (the mode of insertion does not affect infection risk).41 Even mechanical failure is reported low and is <5% at 5 years.35, 36
Our results confirm that penile prosthesis implant is a safe procedure that leads to improved satisfaction, with 5 (2.78%) reported complications in our series. Regardless of ED origin, we reported an average increase in IIEF score of more than 12 points and patients responded to EDITS survey with a median score of 72.2 that belong to the 'very satisfied' category. In our series, three infections, one urethral erosion and one prosthesis extrusion were reported. Furthermore, no surgical complications were reported, and only 12 scrotal hematoma occurred. We can define our approach as a minimally invasive surgical technique as our infrapubic skin incision is only 3 cm and our bilateral corporotomy is only 1.5 cm. The corpora cavernosa are dilated only with a Furlow dilator, and cavernosal artery and cavernosal tissue are preserved. This approach avoids the sensation of 'cold penis' and allow accessory erections.
All of these results are part of a system that consists of an experienced surgical staff, a safe, rapid and minimally invasive surgical technique and the usage of the latest technology in prosthesis equipment.
Conclusions
ED, regardless of the cause, can be effectively treated with implantation of an inflatable three-piece prosthesis. This is a safe and efficacious approach, and the patient and partner satisfaction is very high. Surgical technique should be minimally invasive and latest technology equipment should be implanted in order to decrease after surgery common complications.
References
Lindau ST, Schumm LP, Laumann EO, Levinson W, O'Muircheartaigh CA, Waite LJ . A study of sexuality and health among older adults in the United States. N Engl J Med 2007; 357: 762–774.
Porst H, Sharlip I . History and epidemiology of male sexual dysfunction. In: Porst H, Buval J eds. Standard Practice in Sexual Medicine. Blackwell Publishing: Malden, MA, USA, 2006; 43–48.
Feldman HA, Goldstein I, Hatzichristou DG, Krane RJ, McKinlay JB . Impotence and its medical and psychosocial correlates: results of the Massachusetts Male Aging Study. J Urol 1994; 151: 54–61.
Lee JC, Benard F, Carrier S, Talwar V, Defoy I . Do men with mild erectile dysfunction have the same risk factors as the general erectile dysfunction clinical trial population? BJU Int 2011; 107: 956–960.
Stanford JL, Feng Z, As Hamilton, Gilliland FD, Stephenson RA, Eley JW et al. Urinary and sexual function after radical prostatectomy for clinically localized prostate cancer: the Prostate Cancer Outcomes Study. JAMA 2000; 283: 354–360.
Schiavina R, Borghesi M, Dababneh H, Pultrone CV, Chessa F, Concetti S et al. Survival, Cotinence and Potency (SCP) recovery after radical retropubic prostatectomy. A long-term combined evaluation of surgical outcomes. Eur J Surg Oncol 2014; 40: 1716–1723.
Dubbelman YD, Dohle GR, Schroder FH . Sexual function before and after radical retropubic prostatectomy: a systematic review of prognostic indicators for a successful outcome. Eur Urol 2006; 50: 711–720.
Mulhall JP, Bella AJ, Briganti A, McCullough A, Brock G . Erectile function rehabilitation in the radical prostatectomy patient. J Sex Med 2010; 7: 1687–1698.
Gontero P, Fontana F, Zitella A, Montorsi F, Frea B . A prospective evaluation of efficacy and compliance with a multistep treatment approach for erectile dysfunction in patients after non-nerve sparing radical prostatectomy. BJU Int 2005; 95: 359–365.
Bettocchi C, Palumbo F, Spilotros M, Lucarelli G, Palazzo S, Battaglia M et al. Patient and partner satisfaction after AMS inflatable penile prosthesis implant. J Sex Med 2010; 7: 304–309.
Minervini A, Ralph DJ, Pryor JP . Outcome of penile prosthesis implantation for treating erectile dysfunction: Experience with 504 procedures. BJU Int 2006; 97: 129–133.
Henry GD, Wilson SK, Delk JR 2nd, Carson CC, Wiygul J, Tornehl C et al. Revision washout decreases penile prosthesis infection in revision surgery: a multicenter study. J Urol 2005; 173: 89–92.
Carson CC . Diagnosis, treatment and prevention of penile prosthesis infection. Int J Impot Res 2003; 15: S139–S146.
Montague DK, Angermeier KW, Lakin MM . Penile prosthesis infections. Int J Impot Res 2001; 13: 326–328.
Carson CC . Infections in genitourinary prostheses. Urol Clin North Am 1988; 16: 139–147.
Wilson SK, Costerton JW . Biofilm and penile prosthesis infections in the era of coated implants; a review. J Sex Med 2012; 9: 44–53.
Wilson SK, Zumbe J, Henry GD, Salem EA, Delk JR, Cleves MA . Infection reduction using antibiotic-coated inflatable penile prosthesis. Urology 2007; 70: 337–340.
Chung E, Brock G . Sexual rehabilitation and cancer survivorship: a state of art review of current literature and management strategies in male sexual dysfunction among prostate cancer survivors. J Sex Med 2013; 10: 102–111.
Montorsi F, Rigatti P, Carmignani G, Corbu C, Campo B, Ordesi G et al. AMS three-piece inflatable implants for erectile dysfunction: a long-term multi-institutional study in 200 consecutive patients. Eur Urol 2000; 37: 50–55.
Perito PE . Minimally invasive infrapubic inflatable penile implant. J Sex Med 2008; 5: 27–30.
Zippe CD, Pahlajani G . Penile rehabilitation following radical prostatectomy: role of early intervention and chronic therapy. Urol Clin North Am 2007; 34: 601–618.
Fraiman MC, Lepor H, McCullough AR . Changes in penile morphometrics in men with erectile dysfunction after nerve-sparing radical retropubic prostatectomy. Mol Urol 1999; 3: 109–115.
Megas G, Papadopoulos G, Stathouros G, Moschonas D, Gkialas I, Ntoumas K . Comparison of efficacy and satisfaction profile, between penile prosthesis implantation and oral PDE5 inhibitor Tadalafil therapy, in men with nerve-sparing radical prostatectomy erectile dysfunction. BJU Int 2012; 112: E169–E176.
Schwartz EJ, Wong P, Graydon RJ . Sildenafil preserves intracorporeal smooth muscle after radical retropubis prostatectomy. J Urol 2004; 171: 771–774.
Padma-Nathan H, McCullough AR, Levine LA, Lipshultz LI, Siegel R, Montorsi F . Randomized, double-blind, placebo-controlled study of postoperative nightly sildenafil citrate for the prevention of erectile dysfunction after bilateral nerve-sparing radical prostatectomy. Int J Impot Res 2008; 20: 479–486.
Raina R, Lakin MM, Agarwal A, Mascha E, Montague DK, Klein E et al. Efficacy and factors associated with successful outcome of sildenafil citrate use for erectile dysfunction after radical prostatectomy. Urology 2004; 63: 960–966.
Jiann BP, Yu CC, Su CC, Tsai JY . Compliance of Sildenafil treatment for erectile dysfunction and factors affecting it. Int J Impot Res 2006; 18: 146–149.
Linet OI, Ogrinc FG . Efficacy and safety of intracavernosal alprostadil in men with erectile dysfunction. The Alprostadil Study Group. N Engl J Med 1996; 334: 873–877.
Porst H . The rationale for prostaglandin E1 in erectile failure: a survey of worldwide experience. J Urol 1996; 155: 802–815.
Lehmann K, Casella R, Blochlinger A, Gasser TC . Reasons for discontinuing intracevernous injection therapy with prostaglandin E1 (Alprostadil). Urology 1999; 53: 397–400.
Levine LA, Dimitriou RJ . Vacuum constriction and external erection devices in erectile dysfunction. Urol Clin North Am 2001; 28: 335–341.
Cookson MS, Nadig PW . Long-term results with vacuum constriction device. J Urol 1993; 149: 290–294.
Lewis RW, Witherington R . External vacuum therapy for erectile dysfunction: use and results. World J Urol 1997; 15: 78–82.
Mulcahy JJ, Austoni E, Barada JH, Choi HK, Hellstrom WJ, Krishnamurti S et al. The penile implant for erectile dysfunction. J Sex Med 2004; 1: 98–109.
Montague DK, Angermeier KW . Penile prosthesis implantation. Urol Clin North Am 2001; 28: 355–361.
Mulhall JP, Ahmed A, Branch J, Parker M . Serial assessment of efficacy and satisfaction profiles following penile prosthesis surgery. J Urol 2003; 169: 1429–1433.
Natali A, Olianas R, Fisch M . Penile implantation in Europe: successes and complications with 253 implants in Italy and Germany. J Sex Med 2008; 5: 1503–1512.
Bernal RM, Henry GD . Contemporary patient satisfaction rates for three-piece inflatable penile prosthesis. Adv Urol 2012; 2012: 707321.
Moskovic DJ, Gittens P, Avila D Jr, Chandrashekar A, Khera M, Lipshultz LI . Favorable female sexual function is associated with patient satisfaction after inflatable penile prosthesis implantation. J Sex Med 2011; 8: 1996–2001.
Akin-Olugbade O, Parker M, Guhring P, Mulhall J . Determinants of patient satisfaction following penile prosthesis surgery. J Sex Med 2006; 3: 743–748.
Carson CC . Efficacy of antibiotic impregnation of inflatable penile prosthesis in decreasing infection in original implant. J Urol 2004; 171: 1611–1614.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-nd/4.0/
About this article
Cite this article
Antonini, G., Busetto, G., De Berardinis, E. et al. Minimally invasive infrapubic inflatable penile prosthesis implant for erectile dysfunction: evaluation of efficacy, satisfaction profile and complications. Int J Impot Res 28, 4–8 (2016). https://doi.org/10.1038/ijir.2015.33
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/ijir.2015.33
This article is cited by
-
Analysis of the effects of different surgical approaches on corporotomy localization in inflatable penile implant surgery performed by expert implant surgeons
International Journal of Impotence Research (2023)
-
The good, the bad, and the ugly about surgical approaches for inflatable penile prosthesis implantation
International Journal of Impotence Research (2022)
-
A systematic review of penile prosthesis infection and meta-analysis of diabetes mellitus role
BMC Urology (2021)
-
Laparoscopic treatment of pudendal nerve and artery entrapment improves erectile dysfunction in healthy young males
International Journal of Impotence Research (2021)
-
Alternative surgical approach for inflatable penile prosthesis removal
Basic and Clinical Andrology (2020)