Abstract
Emotional distress has been associated with a poorer prognosis in myocardial infarction patients. Elevated adrenocorticotrophic hormone (ACTH), lower cortisol, dehydroepiandrosterone sulfate (DHEAS) and cortisol:DHEAS, as measures of emotional distress, might correlate with silent myocardial ischemia (SMI) and workload. Thus, we assessed the relationship between emotional distress, SMI and double product (systolic blood pressure (SBP) × heart rate). Cross-sectional South African biethnic single-set cohorts (N=378), aged 44.7±9.52 years, were investigated. Depressive symptoms (Patient Health Questionnaire-9), anthropometric, fasting blood, 24-h double product and 24-h 2-lead electrocardiogram (ST-segment depression) values were obtained. Blacks, mostly men, had increased depressive symptoms, hyperglycemia, SMI, double product, SBP hypertension and ACTH but lower cortisol, DHEAS and cortisol:DHEAS than their White counterparts. Black men had the highest combined SBP hypertension and below-median cortisol prevalence, 38%, compared with 5.9–13.8% in the other groups. Their SMI was associated with ACTH and cortisol:DHEAS (adj. R2 0.29; β 0.27–0.31 (0.12–0.64); P⩽0.05), double product (adj. R2 0.29; β 0.38 (0.18–0.57); P=0.050) and SBP hypertension (area under the curve: 0.68 (95% CI: 0.56, 0.80); P=0.042; sensitivity/specificity 49/85%). Double product was positively associated with central obesity in all sex groups and with cortisol in the Black men (P<0.05). A dysregulated hypothalamic-pituitary-adrenal-axis (HPAA) showed signs of a hyporesponsive adrenal cortex, suggesting chronic emotional stress in the Black male cohort. In this cohort, HPAA dysregulation and compensatory increases in double product occur as a potential defense mechanism to alleviate perfusion deficits, thereby potentiating ischemic heart disease risk.
Similar content being viewed by others
Introduction
Globally, hypertension is responsible for an estimated 45% of deaths because of heart disease and 51% of deaths because of stroke.1 However, increasing concern regarding hypertension prevalence has been raised by findings obtained from the Sympathetic activity and Ambulatory Blood Pressure in Africans (SABPA) prospective study.2, 3 Hamer et al.2 and Malan et al.3 demonstrated higher 24-h hypertension prevalence (66%) in Blacks compared with White teachers (42%).2, 3 Since 1989, various factors have contributed to higher hypertension prevalence in Africans, particularly when exposed to a taxing stressful environment and when acculturation is evident.4, 5 Indeed, emotional stress has been associated with a risk for hypertension3, 5 and ischemic heart disease,6, 7, 8 but is largely understudied in Africa. To date, emotional stress has been associated with left ventricular wall remodeling,7 silent myocardial ischemia (SMI) and vascular disease in a metanalyses8 and in a Black male cohort.7, 9, 10 However, further investigation on the hypothalamic-pituitary-adrenal-axis (HPAA) emotional stress response and cardiomyopathy is warranted.
Prolonged exposure to taxing emotional stress may disrupt the maintenance of normal circulatory levels of cortisol, resulting in dysregulation of the HPAA and adrenal cortex maladaptation.9, 10, 11, 12, 13, 14, 15 Under normal circumstances, HPAA negative feedback responses entail the secretion of hypothalamic corticotrophin‐releasing hormone by parvicellular neurons of the hypothalamic paraventricular nucleus, which stimulates pituitary adrenocorticotrophic hormone (ACTH) secretion and the synthesis and secretion of glucocorticoids by the adrenal cortex.11, 12, 13, 14, 15 A dysregulated HPAA may thus elicit a glucocorticoid response, which impairs the individual’s adaptation to stress to a more non-responsive system or adrenal fatigue. HPAA dysregulation will elevate pituitary production of ACTH albeit lower cortisol and androgen hormone, that is, dehydroepiandrosterone sulfate (DHEAS) levels.13, 14 DHEAS antagonizes the effects of cortisol and lowers the levels of both cortisol and DHEAS. In fact, disrupted cortisol:DHEAS ratios were found among those with depression and adrenal fatigue.13, 14 In hypertensive subjects, relative attenuation in HPAA feedback sensitivity was found following dexamethasone suppression.11 Thus, dysregulation of the HPAA might correlate to myocardial ischemia and volume loading owing to increased metabolic demands. Double product (systolic blood pressure (SBP) × heart rate), acting as an index of myocardial oxygen consumption and workload,16, 17 will increase to alleviate perfusion deficits (ST-segment depression) to maintain homeostasis. Thus, our main aim was to assess the relationships between emotional distress markers resembling HPAA activity (ACTH, cortisol, DHEAS, cortisol:DHEAS, waist circumference (WC)), SMI and double product in a South African biethnic sex cohort.
Methods
Study design and participant selection
Our substudy is nested in the Sympathetic activity and Ambulatory Blood Pressure in Africans (SABPA) study (2008–2009), described in detail elsewhere.18 Black Africans (Blacks) and White Africans (Whites) with similar socioeconomic status included 409 school teachers (aged 20–65 years) from the Dr Kenneth Kaunda Education District, South Africa (Figure 1). Exclusion criteria were tympanum temperature above 37.5 °C, the use of psychotropic substances or α- and β-blockers and blood donors or individuals vaccinated within 3 months before data collection. In addition, we excluded cortisone derivative users (n=3), participants diagnosed with atrial fibrillation (n=16) and clinically diagnosed diabetes (n=12). The final sample consisted of 378 individuals. Participants were fully informed of the study procedure and provided their signed informed consent. The study was approved by the Ethics Committee of the North-West University (NWU-00036-07-A6) and complied with the Declaration of Helsinki criteria for Human Research (revised 2004).
Experimental methods and clinical assessments
Research procedure
The research team was thoroughly trained for the 48 h clinical assessment phase, and all apparatuses were calibrated before use. Between 0700 and 0900 hours on a working day at school, ambulatory blood pressure, electrocardiogram (Cardiotens CE120; Meditech, Budapest, Hungary) and accelerometer apparatuses were applied (Actical; Mini Mitter, Montreal, Quebec). At 1630 hous, participants were transported to the North-West University Metabolic Unit Research Facility, where they were introduced to the experimental setup and underwent further clinical assessments. Participants completed a battery of psychosocial tests under the supervision of a registered clinical psychologist. Participants received a standardized dinner and were requested to go to bed at no later than 2200 hours and to fast overnight. At 0615 hours, the ambulatory blood pressure monitors and accelerometers were removed, followed by anthropometric measurements and blood sampling.
Cardiovascular assessment
The ambulatory blood pressure was fitted to the non-dominant arms of four teachers using an appropriately rectangular cuff size. Blood pressure measurements were obtained every 30 min during the day (0800–2200 hours) and hourly during the night (2200–0600 hours).19 Participants continued their usual daily activities and were asked to record occurrences of stress, physical activity, headache, syncope, dizziness, nausea, palpitations, hot flushes and visual disturbances on their ambulatory diary card. The mean successful inflation rate was lower in Black subjects (men, 75.8% and women, 69.6%) than White subjects (men, 84.5% and women, 84.6%). The observed pronounced troncoconical-shaped arms20 of obese Black women contributed to the lower cuff inflation rate.20, 21
SMI events or perfusion deficits (ST-segment depression) were assessed by two-channel 24-h electrocardiogram recordings (Cardiotens CE120; Meditech) for 20 s at 5 min intervals. Before the start of the ambulatory investigation, the isoelectric reference point (PQ segment), J point and L point (80 ms after the J point), with an ST-segment detection interval of at least 3 mm as the initial ST level, were calculated individually for each patient. An ischemic event was recorded according to the following criteria: horizontal or descending ST-segment depression by at least 1 mm; duration of the ST-segment episode lasting ⩾1 min, and a ⩾1-min interval from the preceding episode.22 In the case of horizontal or descending ST depression (1 mm–1 min duration at a 1- min interval from the preceding episode), an electrocardiogram tracing lasting 60 s was recorded and an additional blood pressure measurement was automatically initiated by the trigger mechanism of the device. The data were analyzed using CardioVisions 1.19 Personal Edition (Meditech). Ambulatory hypertension was defined as systolic and/or diastolic ⩾130/80 mm Hg or the use of antihypertensive medication.
Anthropometric measurements
The Actical accelerometer monitor (Mini Mitter, Bend, OR, USA; Montreal, QC, Canada) measured physical activity for 24 h considering resting metabolic rate. Anthropometric measurements were performed in triplicate by registered anthropometrists (Precision health scale (A & D Company, Tokyo, Japan) and Invicta Stadiometer IP 1465 (Invicta, London, UK)). For standardization purposes, circumference measurements were obtained with a non-extensible and flexible anthropometric tape. WC was obtained at the midpoint between the lower costal rib and iliac crest, perpendicular to the long axis of the trunk, not at the narrowest point. Body surface area was calculated for each participant according to the Mosteller formula. Intra- and interobserver variability was <10%.
Depressive symptoms
Depressive symptoms were assessed using the 9-item Patient Health Questionnaire (PHQ-9),23 which has been validated in various ethnic groups, including sub-Saharan Africans.24 The questionnaire is designed for use in primary health-care settings adapting diagnostic criteria from the DSM-IV (Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition). Each item of the PHQ-9 evaluates the presence of one of the nine DSM-IV criteria of major depression. In the current study, the Cronbach’s α reliability index for the total PHQ-9 score was 0.81. Items on the questionnaire are scored to reflect the frequency of symptom occurrence during the prior 2 weeks. The recommended and established PHQ-9 cutoff point of >10 indicated clinical moderate–severe depression.23, 24
Blood sampling and biochemical analyses
Fasting blood samples were obtained from the antebrachial vein branches with a winged infusion set using a standardized protocol and stored at −80 °C until batch assay. γ-Glutamyl transferase (γ-GT) and cotinine levels were used as proxy biomarkers for alcohol and smoking habits. Sequential multiple analyzers assessed NaF glucose, serum γ-GT, high-sensitivity C-reactive protein, cotinine and HbA1C (glycated hemoglobin) (Konelab 20i (Thermo Scientific, Vantaa, Finland), Unicel DXC 800- Beckman and Coulter (Ludwigsburg, Germany) and Integra 400 (Roche, Switzerland, respectively)). Serum cortisol, DHEAS and ACTH samples were obtained before 0900 hours and analyzed with ECLIA (Elecsys 2014, Roche Basel, Switzerland). Inter- and intrabatch variability was 5.4% and 2.9%, respectively. EDTA plasma HIV infection status was determined using the First Response Kit (PMC Medical, Daman, India) and confirmed using the Pareekshak test (Bhat Biotech, Bengaluru, India).
Statistical analysis
Statsoft (Statistica) version 13 (Statsoft Inc., Tulsa, OK, USA; 2013) and SPSS software package version 22 for Windows (IBM, SPSS, Chicago, IL, USA) were used to perform data analyses. Normality of the data was ascertained with Shapiro–Wilks analyses, and logarithmic transformation was deemed appropriate for C-reactive protein, physical activity, cotinine, γ-GT and SMI. General linear models determined the main effects interaction (ethnic × sex) for cardiometabolic risk markers independent of a priori confounders (age, WC, log physical activity, log cotinine and log γ-GT). Baseline characteristics were compared using Student's t-tests and presented as the median±interquartile ranges. χ2 Tests computed proportions and prevalence. To determine HPAA dysregulation, the cohort was stratified into low (<346.45 nmol l−1) and high (⩾346.45) cortisol levels. Normal reference ranges for fasting serum cortisol when sampled before 0900 hours varies between 171 and 536 nmol l−1.13
The linear association between SMI and 24 h SBP hypertension was determined from the maximum of the Youden index (J) (sensitivity+specificity−1) using nonparametric receiver operating characteristic curves in the biethnic sex groups. Multiple linear regression analyses were computed in several models. Forward stepwise regression analyses determined associations (1) between the dependent (SMI and double product) and independent variables (ACTH, cortisol, depressive symptoms and a priori confounders) and (2) between the dependent (SMI and double product) and independent variables (cortisol:DHEAS, depressive symptoms and a priori confounders). Double product was added as covariate in the SMI models.
Sensitivity analyses
Linear regression analyses were repeated (1) after excluding HIV-infected subjects and (2) hypertensive medication users. The null hypothesis was rejected for values of P⩽0.05.
Results
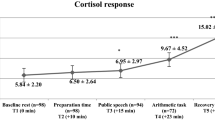
General linear models determined biethnic sex differences for SMI (F1336=13.15, P<0.001) and double product (F1364=15.71, P<0.001) independent of a priori confounders. Biethnic differences existed for ACTH (F1336=19.13, P<0.006) and cortisol (F1364=15.69, P<0.001). Thus, we stratified the participant sample into ethnic × sex subgroups.
In Table 1, Black subjects displayed a shorter stature; cardiometabolic vulnerability (higher alcohol consumption, mean hyperglycemia (HbA1C⩾5.7%), mean low-grade inflammation (C-reactive protein ⩾3 mg l−1)); more emotional stress (higher ACTH, depressive symptoms, lower DHEAS); increased SMI prevalence rate; and higher double product, and BP and heart rate levels than White subjects.
In Table 2, considering confounders, a similar trend but more defined profile of cardiometabolic risk was observed, particularly in Black men. Black men revealed more emotional distress (higher ACTH, lower cortisol and DHEAS, moderate–severe depression), increased SMI, BP, double product and antihypertensive medications usage than White men. Black women displayed less cardiometabolic vulnerability than their male counterparts but demonstrated a higher risk than White women in most cases (P⩽0.05).
SMI was associated with SBP hypertension in Black men (area under the receiver operating characteristic curve=0.68 (95% CI: 0.56, 0.80); P=0.02; sensitivity/specificity 49/85%) (Supplementary Table A1).
In Table 3, positive associations (P⩽0.05) were observed between SMI and emotional distress markers (ACTH and cortisol:DHEAS) in Black men. Double product was positively associated with SMI, cortisol and alcohol intake (γ-GT) in Black men (P⩽0.05). Positive associations were also evident between double product and WC in all ethnic and sex groups, P⩽0.05. Self-reported depressive symptoms were not related to SMI or double product in any of the subgroups. Excluding HIV-infected subjects and antihypertensive medication users from the linear regression analyses did not change the outcome.
In Figure 2, a composite profile of increased risk marker prevalence existed for emotional stress (below-median cortisol,<346.45 nmol l−1), perfusion deficits (SMI) and ambulatory SBP hypertension (12.2–13%) in Black subjects compared with White subjects (5.3–5.9%).
Composite profile of risk marker prevalence in a biethnic single-sex cohort from South Africa with SBP hypertension; SBP hypertension plus 24 h SMI (silent myocardial ischemic events); SBP hypertension plus low cortisol (cortisol below median: <346.45 nmol l−1); or SBP hypertension plus 24 h SMI plus low cortisol (cortisol below median: <346.45 nmol l−1).
Figure 3 provides a graphical presentation of the proposed dysregulated HPAA mechanism in Black men.
A hyporesponsive adrenal cortex suggests chronic emotional distress, suggesting dysregulation of the HPAA in a Black male cohort. Dysregulation of the HPAA and compensatory increases in double product occur as a defense response to alleviate perfusion deficits potentiated ischemic heart disease risk. Any opinion, findings and conclusions or recommendations expressed in this material are those of the author(s) and therefore the funding bodies do not accept any liability in regard thereto. ACTH, adrenocorticotrophic hormone; CRH, corticotrophin‐releasing hormone; DHEAS, dehydroepiandrosterone sulfate; HPAA, hypothalamic-pituitary-adrenal-axis.
Discussion
Overall, dysregulated HPAA suggestive of adrenal hyporesponsiveness and chronic emotional distress was associated with myocardial silent ischemia and increased myocardial workload in a Black African male cohort. Compensatory increases in myocardial oxygen consumption or workload to alleviate perfusion deficits were demonstrated with an increased heart rate and an alarmingly high ambulatory SBP hypertension prevalence of 70.7%. To the best of our knowledge, this is the first quantitative study demonstrating a direct relationship between the brain (emotional stress) and heart (myocardial ischemia and double product) in a cohort from sub-Saharan Africa.
Specifically, a matter of great concern is the poor BP control and accompanying SMI profile of Black male teachers. Only 33.7% of these teachers reported hypertension medication usage, reflecting either unawareness or a lack of compliance, thereby increasing their stroke risk.3 Concurrently, the Inter-stroke Investigators’ report obtained from 32 countries showed a population stroke risk of 47.9% attributed to hypertension, whereas 9.1% was due to cardiac causes.25 Despite the large representative study sample, for stress data, similar to alcohol intake, a 5.8% risk was observed. However, findings from this report were mostly self-reported (qualitative), and varying protocols may not truly reflect susceptibility for ischemic heart disease and stroke.
Emotional stress and HPAA dysregulation
In our cohort, quantitative measurement of emotional stress risk markers were determined and higher ACTH levels but lower cortisol, DHEAS and cortisol:DHEAS levels, were evident in the Black cohort. Higher levels of cortisol were expected as high cortisol levels have been associated with acute emotional distress.12 However, chronic exposure to emotionally demanding psychosocial stress situations may facilitate regulatory feedback, resulting in the downregulation or hyporesponsiveness26, 27, 28, 29 between the HPAA, pituitary ACTH and adrenal activity.11, 12, 13, 14, 15 Indeed, chronic depression symptoms were evident in the current urban-dwelling cohort, underscoring the notion of chronic emotional distress and potential dysregulated HPAA at baseline.3 Ongoing unremitting stress indicates that the adrenal gland is in a constant state of alert and does not have time to recover, which may result in exhaustion.13, 14 This finding might explain the higher ACTH but lower cortisol, DHEAS and cortisol:DHEAS levels in Black men, accompanied by more depressive symptoms than in White men, exacerbating dysregulation of the HPAA. A loss of downstream signaling appears to occur at the receptor level in the adrenal cortex, desensitizing the cortisol-releasing cells to ACTH, which reduces negative feedback mechanisms of cortisol and DHEAS on ACTH.26, 29 Thus, we cautiously suggest the possibility of cortisol hyporesponsivity or potential exhaustion, as chronic emotional distress facilitated HPAA hyperactivity and desensitized cortisol. This finding supports the observed higher ACTH and lower cortisol:DHEAS in Black men. However, the decline in cortisol:DHEAS ratio is the result of a larger decline in cortisol than in DHEAS. The positive association of cortisol:DHEAS with SMI is thus driven more by lower cortisol than DHEAS levels. Our data firmly support the results of De Kock et al.9 who showed attenuated cortisol responses to acute mental stress in SABPA Black men, suggesting adrenal hyporesponsiveness or fatigue. A similar trend was also shown in other African cohort studies.5, 7 However, prospective findings are needed to confirm HPAA downregulation.
On a related note, when cortisol levels are disrupted, central obesity acts as a strong supporting marker for emotional distress.30, 31, 32, 33 Björntorp33 demonstrated an association between psychosocial stress and increased corticoid receptor binding in abdominal adipose tissue, thus reflecting increased cortisol levels and central obesity. The urban Black male cohort presented higher ACTH, lower cortisol and DHEAS levels accompanied by central obesity that exceeded recently proposed ethnic-specific WC cut-points (Black men (⩾90 cm))30 and support the possible dysregulation of the HPAA and higher susceptibility for chronic emotional distress.30, 31, 32, 33 The findings of Epel et al.31 also suggested that participants with greater central obesity would be ‘non-habituators’ to stress, that is, that they would reliably secrete cortisol in response to stressful situations. Independent of emotional distress, WC showed strong associations with the cardiovascular risk marker, double product, in the total cohort. However, an increase in double product showed additive myocardial ischemia risk in Black men only when emotional distress values (cortisol:DHEAS) were considered.
Emotional stress, SMI and workload
Because more myocardial ischemic events were observed in the Black men (11.1 events in 24 h), it is plausible that vascular responsiveness10, 34 will increase the double product and may implicate cardiac wall remodeling and ischemic heart disease. Even at the microvasculature level, chronic emotional distress in relationship to vascular dysregulation and ocular perfusion deficits has been shown.3 Chronic depression symptoms accompanied by hypoperfusion predicted a wider retinal venular caliber, an index of stroke risk in the current Black sex cohort.3
We could not identify any studies in Africa showing the importance of double product as a risk marker for emotional distress or cardiovascular disease. In Mongolians, the coexistence of hypertension and high heart rate was shown to be a valuable predictor of stroke and coronary heart disease incidence.35 Double product was also shown to be an independent predictor of cardiovascular mortality in healthy subjects and in patients with ischemic heart disease.36 In the Bogolusa Heart study, African-American adults showed higher double product and increased risk of cardiovascular disease compared with Caucasian adults.37 However, these findings36, 37 oppose the results of Schultz et al.16 and Schutte et al.,38 who demonstrated that double product may not be a good marker of increased cardiovascular disease in African Blacks. In the International Database on Ambulatory blood pressure in relationship to the Cardiovascular Outcomes (IDACO) study,38 double product did not add to risk stratification beyond SBP and heart rate in 9937 subjects (median age, 53.2 years; 47.3% females). However, none of these studies16, 35, 36, 37, 38 considered associations between emotional stress markers and double product as a cardiovascular disease risk.
Presently, we argue that double product may not precede SMI;22, 39 instead, it may be compensatory to alleviate perfusion deficits and associated HPAA dysregulation39, 40, 41 in Black men. Their higher alcohol intake may further induce central nervous system depression and a dysregulated HPAA, as cortisol interacts with the brain’s reward system, contributing to the reinforcing effects of alcohol on myocardial oxygen supply.39 The prognostic value of double product as an index of myocardial oxygen consumption may also be supported by enhanced sympathetic hyperactivity in Black men18, 29, 30, 34 with initial increases in cortisol. However, during chronic emotional distress, HPAA dysregulation will increase vasoconstriction responsivity and potentiate SMI.34 Thus, potential adrenal fatigue (higher ACTH, hyporesponsive cortisol:DHEAS) accompanied by SMI may impair autoregulation and facilitate compensatory increases in double product. Thus, we cautiously suggest that when chronic emotional distress and potential dysregulation of the HPAA is apparent, maladaptive or high ACTH and below-median cortisol levels may facilitate more SMI events to comply with higher central metabolic demands. The dysregulated HPAA in the current study population does not act as a protective mechanism against SMI.11, 18, 34 Thus, our data contradict findings in metabolic syndrome rodent models, where protective effects of glucocorticoid receptor blockers showed less cardiac damage and adipose tissue inflammation.43
Increases in double product act as a compensatory mechanism or defense response to upregulate metabolic demands, resulting in an increase in myocardial oxygen supply in the maintenance of homeostasis. Higher chronic emotional demands emphasize susceptibility to myocardial ischemia, and these emotional demands may be the underlying reason for the differences observed in the biethnic sex cohort. Black females may have increased resiliency towards emotional distress as their SMI was positively associated with cortisol, which is indicative of acute stress.30, 31, 32, 33 However, no differences were observed in SMI or double product when compared with White females. More investigations are needed to clarify this matter.
Limitations of this study include the relatively small sample size, which may not represent other teacher cohorts from sub-Saharan Africa. Prospective findings are warranted to confirm dysregulation of the HPAA and accompanying risk markers for cardiac stress.
In conclusion, a combination of increased central obesity and higher ACTH-hyporesponsive cortisol:DHEAS may be the result of chronic emotional distress in a Black male cohort. Such a profile resembles a dysregulated HPAA in Black men. The absence of chronic emotional distress in Black females or in the White sex cohort may explain the lower ACTH-cortisol:DHEAS in these groups. Dysregulation of the HPAA in Black men further correlated with myocardial ischemia and volume loading due to higher metabolic demands. Double product increases, as a defense response to alleviate perfusion deficits, potentiated future ischemic heart disease risk.
References
World Health Organisation The World Health Report: Non-Communicable Diseases Country Profiles. ISBN: 789241507509. WHO: Geneva, Switzerland, 2014, pp207.
Hamer M, Von Känel R, Reimann, Malan NT, Schutte AE, Huisman HW, Malan L . Progression of cardiovascular risk factors in Black Africans: 3 year follow up of the SABPA cohort study. Atherosclerosis 2015; 238: 52–54.
Malan L, Hamer M, von Känel R, Schlaich MP, Reimann M, Frasure-Smith-N, Lambert GW, Vilser W, Harvey B, Steyn HS, Malan NT . Chronic depression symptoms and salivary NOx are associated with retinal vascular dysregulation: the SABPA study. Nitric Oxide Biol Chem 2016; 55–56: 10–17.
Malan L, Malan NT, Wissing MP, Seedat YK . Coping with urbanization: a cardiometabolic risk? The THUSA study. Biol Psychol 2008; 79: 323–328.
Malan NT, Brits JS, Eloff FC, Huisman HW, Kruger A, Laubscher PJ, Pretorius PJ . The influence of acculturation on endocrine reactivity during acute stress in urban black males. Stress Med 1996; 12: 55–63.
Seldenrijk A, Hamer M, Lahiri A, Penninx BWJH, Steptoe A . Psychological distress, cortisol stress response and subclinical coronary calcification. Psychoneuroendocrinology 2012; 37: 48–55.
Mashele N, Malan L, Van Rooyen JM, Harvey BH, Potgieter JC, Hamer M . Blunted neuroendocrine responses linking depressive symptoms and ECG-left ventricular hypertrophy in black Africans: the SABPA study. Cardiovasc Endocrinol 2014; 3: 59–65.
Batty GD, Russ TC, Stamatakis E, Kivimäki M . Psychological distress and risk of peripheral vascular disease, abdominal aortic aneurysm, and heart failure: Pooling of sixteen cohort studies. Atherosclerosis 2014; 236: 385–388.
De Kock A, Malan L, Hamer M, Cockeran M, Malan NT . Defensive coping and renovascular disease risk—adrenal fatigue in a cohort of Africans and Caucasians: the SABPA study. Phys Behav 2015; 147: 213–219.
Malan L, Hamer M, Schlaich MP, Lambert GL, Harvey BH, Reimann M, Ziemssen T, De Geus JCN, Huisman HW, Van Rooyen JM, Schutte R, Schutte AE, Fourie CMT, Malan NT . Facilitated defensive coping, silent ischaemia and ECG left-ventricular hypertrophy: the SABPA study. J Hypertens 2012; 30: 543–550.
Wirtz PH, von Känel R, Emini L, Ruedisueli K, Groessbauer S, Maercker A, Ehlert U . Evidence for altered hypothalamus-pituitary-adrenal axis functioning in systemic hypertension: blunted cortisol response to awakening and lower negative feedback sensitivity. Psychoneuroendocrinology 2007; 32: 430–436.
Hammer F, Stewart PM . Cortisol metabolism in hypertension. Best Pract Res Clin Endocrinol Metab 2006; 20: 337–353.
Dorin RI, Qualls CR, Crapo LM . Diagnosis of adrenal insufficiency. Ann Intern Med 2003; 139: 194–204.
Whitworth JA, Williamson PM, Mangos G . Cardiovascular consequences of cortisol excess. Vasc Health Risk Manag 2005; 1: 291–299.
Engert V, Efanov SI, Duchense A . Differentiating anticipatory from reactive cortisol responses to psychosocial stress. Psychoneuroendocrinology 2013; 38: 128–133.
Shultz AJ, Schutte AE, Schutte R . Double product and end-organ damage in African and Caucasian men: the SABPA study. Int J Cardiol 2013; 167: 792–797.
Gerald S, Berenson MD, Dharmendrakumar A . Pressure–heart rate product changes from childhood to adulthood in a biracial population—a crossover phenomenon: the Bogalusa Heart Study. J Am Society Hypertens 2008; 2: 80–87.
Malan L, Hamer M, Frasure-Smith N, Steyn HS, Malan NT . COHORT PROFILE: sympathetic activity and Ambulatory Blood Pressure in Africans (SABPA) Prospective Cohort Study. Int J Epidemiol 2015; 44: 1814–1822.
Kohara K, Nishida W, Maguchi M, Hiwida K . Autonomic nervous function in non-dipper essential hypertensive participants: evaluation by power spectral analysis of heart rate variability. Hypertension 1995; 26: 808.
Palatini P, Benetti E, Fania C, Malipiero G, Saladini F . Rectangular cuffs may overestimate blood pressure in individuals with large conical arms. J Hypertens 2012; 30: 530–536.
O’Brien E . Prognostic value of ambulatory blood pressure monitoring in obese patients. J Clin Hypertens 2016; 18: 119–120.
Uen S, Baulmann J, Dusing R, Glanzer K, Vetter H, Mengden T . ST-segment depression in hypertensive patients is linked to elevations in blood pressure, pulse pressure and double product by 24-h Cardiotens monitoring. J Hypertens 2003; 21: 977–983.
Kroenke K, Spitzer RL . The PHQ-9: a new depression diagnostic and severity measure. Psychiatr Ann 2002; 32: 1–7.
Monahan PO, Shacham E, Reece M, Kroenke K, Ong’or WO, Omollo O, Yebei VN, Ojwang C . Validity/reliability of PHQ-9 and PHQ-2 depression scales among adults living with HIV/AIDS in Western Kenya. J Gen Intern Med 2009; 24: 189–197.
O'Donnell MJ, Chin SL, Rangarajan S, Xavier D, Liu L, Zhang H, Rao-Melacini P, Zhang X, Pais P, Agapay S, Lopez-Jaramillo P, Damasceno A, Langhorne P, McQueen MJ, Rosengren A, Dehghan M, Hankey GJ, Dans AL, Elsayed A, Avezum A, Mondo C, Diener HC, Ryglewicz D, Czlonkowska A, Pogosova N, Weimar C, Iqbal R, Diaz R, Yusoff K, Yusufali A, Oguz A, Wang X, Penaherrera E, Lanas F, Ogah OS, Ogunniyi A, Iversen HK, Malaga G, Rumboldt Z, Oveisgharan S, Al Hussain F, Magazi D, Nilanont Y, Ferguson J, Pare G, Yusuf S, INTERSTROKE investigators. Global and regional effects of potentially modifiable risk factors associated with acute stroke in 32 countries (INTERSTROKE): a case–control study. Lancet 2016; 388: 761–775.
Saurez EC, Sundy JS, Erkanli A . Depressogenic vulnerability and sex-specific patterns of neuro-immune dysregulation: What the ratio of cortisol to C-reactive protein can tell us about loss of normal regulatory control. Brain Behav Immun 2015; 44: 137–147.
Prinsloo J, Malan L, de Ridder J, Potgieter J, Steyn H . Determining the waist circumference cut off which best predicts the metabolic syndrome components in urban Africans: the SABPA study. Exp Clin Endocrinol Diabetes 2011; 119: 599–603.
Hamer M, Malan L . Sympathetic nervous activity, depressive symptoms, and metabolic syndrome in black Africans: the Sympathetic Activity and Ambulatory Blood Pressure in Africans study. Stress 2012; 15: 562–568.
De Kock A, Malan L, Hamer M, Malan NT . Defensive coping and subclinical vascular disease risk—associations with autonomic exhaustion in Africans and Caucasians: the SABPA study. Atherosclerosis 2012; 225: 438–443.
McEwen BS . Physiology and neurobiology of stress and adaptation: central role of the brain. Phys Rev 2007; 87: 873–904.
Epel SE, McEwen B, Seeman T, Matthews K, Castellazo G, Brownell KD, Bell J, Ickovics R . Stress and body shape: stress-induced cortisol secretion is consistently greater among women with central fat. Psychosom Med 2000; 62: 623–632.
Incollingo-Rodrigueza AC, Epel ES, Whitea ML, Standena EC, Secklc JR, Tomiyamaa AJ . Hypothalamic-pituitary-adrenal axis dysregulation and cortisol activity in obesity: a systematic review. Psychoneuroendocrinology 2015; 62: 301–318.
Björntorp P . Do stress reactions cause abdominal obesity and comorbidities? Obesity Rev 2001; 2: 73–86.
Malan L, Hamer M, Schlaich MP, Lambert GW, Ziemssen T, Reimann M, Frasure-Smith N, Amirkhan JM, Schutte R, Van Rooyen JM, Mels C, Fourie CMT, Uys AS, Malan NT . Defensive coping facilitates higher blood pressure and early sub-clinical structural vascular disease via alterations in heart rate variability: the SABPA study. Atherosclerosis 2013; 227: 391–397.
Zhong C, Zhong X, Xu T, Peng H, Li H, Zhang M, Wang A, Xu T, Sun Y, Zhang Y . Combined effects of hypertension and heart rate on the risk of stroke and coronary heart disease: a population-based prospective cohort study among Inner Mongolians in China. Hypertens Res 2015; 38: 883–888.
Sadrzadeh-Rafie AH, Dewey FE, Sungar GW, Ashley EA, Hadley D, Myers J, Froelicher VF . Age and double product (systolic blood pressure × heart rate) reserve-adjusted modification of the Duke Treadmill Score nomogram in men. Am J Cardiol 2008; 02: 1407–1412.
Berenson GS, Patel DA, Wang H, Srinivasan SR, Chen W . Pressure-heart rate product changes from childhood to adulthood in a biracial population—a crossover phenomenon: the Bogalusa Heart Study. J Am Soc Hypertens 2008; 2: 80–87.
Schutte R, Thijs L, Asayama K, Boggia J, Li Y, Hansen TW, Liu Y-P, Kikuya M, Björklund-Bodegård K, Ohkubo T, Jeppesen J, Torp-Pedersen C, Dolan E, Kuznetsova T, Stolarz-Skrzypek K, Tikhonoff V, Malyutina S, Casiglia WE, Nikitin Y, Lind L, Sandoya E, Kawecka-Jaszcz K, Filipovský J, Imai Y, Wang J, Ibsen H, O’Brien E, Staessen JA, on behalf of the International Database on Ambulatory blood pressure in relation to Cardiovascular Outcomes (IDACO) Investigators. Double product reflects the predictive power of systolic pressure in the general population: evidence from 9937 participants. Am J Hypertens 2013; 26: 665–672.
Deedwania PC, Nelson JR . Pathophysiology of silent myocardial ischaemia during daily life: hemodynamic evaluation by simultaneous electrocardiographic and blood pressure monitoring. Circulation 1990; 82: 1296–1304.
Oosthuizen W, Malan L, Scheepers JD, Cockeran M, Malan NT . The defense response and alcohol intake: a coronary artery disease risk? The SABPA Study. J Clin Exp Hypertens 2016; 38: 526–532.
Van Deventer CA, Lindeque JZ, Jansen van Rensburg PJ, Malan L, Van der Westhuizen FH, Louw R . Use of metabolomics to elucidate the metabolic perturbation associated with hypertension in a black South African male cohort: The SABPA Study. J Am Soc Hypertens 2015; 9: 104–114.
King A, Munisamy G, de Wit H, Lin S . Attenuated cortisol response to alcohol in heavy social drinkers. Int J Psychophysiol 2006; 59: 203–209.
Takeshita Y, Watanabe S, Hattori T, Nagasawa K, Matsuura N, Takahashi K, Murohara T, Nagata K . Blockade of glucocorticoid receptors with RU486 attenuates cardiac damage and adipose tissue inflammation in a rat model of metabolic syndrome. Hypertens Res 2015; 38: 741–750.
Acknowledgements
We gratefully acknowledge the voluntary collaboration of the participants. The SABPA study would not have been possible without the valuable contributions of the coinvestigators and technical staff. The present study was partially funded by the National Research Foundation, Medical Research Council, North-West University, Potchefstroom Campus, North-West Province, ROCHE Diagnostics South Africa and the Metabolic Syndrome Institute, France.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Supplementary Information accompanies the paper on Hypertension Research website
Supplementary information
Rights and permissions
About this article
Cite this article
Malan, L., Schutte, C., Alkerwi, A. et al. Hypothalamic-pituitary-adrenal-axis dysregulation and double product increases potentiate ischemic heart disease risk in a Black male cohort: the SABPA study. Hypertens Res 40, 590–597 (2017). https://doi.org/10.1038/hr.2017.5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/hr.2017.5
Keywords
This article is cited by
-
Cardiovascular Disease and Hair Cortisol: a Novel Biomarker of Chronic Stress
Current Cardiology Reports (2019)
-
Clinical significance of stress-related increase in blood pressure: current evidence in office and out-of-office settings
Hypertension Research (2018)