Abstract
Purpose
To report a series of patients who presented with an atypical retinal traction band, which was developed after an intravitreal injection of bevacizumab for stage 3 retinopathy of prematurity (ROP).
Methods
We retrospectively reviewed the medical record of three patients (five eyes) who had been referred to a tertiary care centre for the management of fibrous retinal traction band, which occurred after a bevacizumab injection for stage 3 ROP with plus disease. Clinical features and courses of these eyes were described based on the medical record and RetCam fundus photography.
Results
All three patients had taken an intravitreal injection of bevacizumab with or without concomitant laser photocoagulation as an initial treatment option for the active stage 3 ROP. With close follow-ups, regression of extraretinal fibrovascular proliferation and plus disease was noted invariably. After the regression of ROP, atypical fibrous traction membrane had arisen along the major vascular arcades with 2.5 to 4 months of latency, which progressed into tractional retinal detachment (TRD) in three out of five eyes.
Conclusion
In active stage 3 ROP, fibrous tractional membrane and subsequent TRD along the major vascular arcades were developed unpredictably after the regression of neovascular activity following bevacizumab injection as an initial treatment. Therefore, ROP patients who received bevacizumab treatment without previous retinal photocoagulation should be closely followed for more than 4 months after the treatments even if the disease seems to have regressed.
Similar content being viewed by others
Introduction
At present the ablation of avascular retina is a standard treatment method for acute phase retinopathy of prematurity (ROP). However, despite of timely administered ablation of avascular retina, unfavourable structural outcome is still unavoidable in some patients. Furthermore, there could be obstacles to conventional laser ablation of avascular retina, such as a poor systemic condition and opaque media. For these reasons, physicians keenly feel the necessity of other safe, effective, and convenient treatment options.
Vascular endothelial growth factor (VEGF) is known as a key molecule in the pathogenesis of various ischaemic retinopathies. Since bevacizumab, a humanized monoclonal anti-VEGF antibody was introduced to ophthalmic diseases, anti-VEGF agents had been spotlighted as a new treatment method in ischaemic retinopathy. Oxygen-induced vascular closure and consequent hypoxic stress of avascular retina is known as the classic pathogenic mechanism of ROP. VEGF is obviously one of the most important molecules in the development of oxygen-induced retinopathy mouse model1, 2 and elevated intraocular concentration of VEGF is consistently documented in ROP patients.3, 4 For these reasons, bevacizumab has been applicated in limited ROP cases and several clinical articles that report the efficacy and complications of the bevacizumab treatment for ROP were issued recently. Bevacizumab not only had been used as a salvage treatment in progressive cases after conventional laser photocoagulation,5, 6, 7, 8 but also had been applied simultaneously with retinal photocoagulation.9, 10 Moreover, Mintz-Hittner and associates11, 12 even tried bevacizumab monotherapy for treating moderate and severe stage 3 ROP patients in zone I or posterior zone II. Despite of the concerns about retinal neuro-developmental delay, disturbance of normal vasculogenesis and systemic side effects, the short-term results of previous clinical trials were promising. Especially, nearly all publication invariably showed the decrement of neovascular activity. However, acute deterioration of tractional retinal detachment (TRD) following intravitreal injection of bevacizumab has been reported in some patients.5, 7, 8, 13, 14 Most of the patients suffered from acute onset contraction of fibrovascular membrane, which leads to the progression of retinal detachment, were stage 4 or 5 ROP at the time point of bevacizumab treatment.
Here we present our experience of three patients with delayed onset atypical fibrous traction band and TRD, which occurred during the regression of neovascular activity after intravitreal injection of bevacizumab. Documentation of the clinical characteristics of those patients could be an alarming message to ophthalmologists and provide a better comprehension about the pathogenesis of ROP.
Methods
We retrospectively reviewed the medical records of patients who were referred to Seoul National University Children’s Hospital (SNUCH) in Seoul, Korea, for the management of atypical retinal traction membrane developed after the intravitreal injection of bevacizumab for stage 3 ROP with plus disease. The data were collected during the period from January 2008 to December 2010. Medical records from prior facility and SNUCH were analysed together with serial fundus photographs taken by RetCam (Clarity Medical Systems Inc., Pleasanton, CA, USA).
Results
Five eyes out of three patients were included. All of the eyes did not undergo retinal ablation prior to the bevacizumab injection. Initially four eyes received simultaneous injection of bevacizumab with laser photocoagulation and the other one eye was treated with bevacizumab alone. Follow-up period after bevacizumab treatment ranged from 19 to 31 months (mean: 23.7 months). Clinical characteristics of the eyes that developed an atypical fibrous retinal traction band after intravitreal bevacizumab injection for stage 3 ROP are summarized in Table 1. The following is a detailed description of each case.
Case 1
A male infant born at 32 weeks of gestation with a weight of 1690 g was referred to SNUCH for the management of TRD following retinal photocoagulation and intravitreal injection of bevacizumab. The patient had received concomitant retinal photocoagulation and intravitreal injection of bevacizumab at gestational age 37 weeks for the management of stage 3 ROP, zone I with plus disease in both eyes. Laser ablation was applied to the whole avascular retina in a confluent manner (intensity: 300 mW, OD: 2297 applications, OS: 2369 applications). The injection of bevacizumab (0.75 mg, 0.03 ml) was performed immediately after laser ablation. All procedures were performed by an experienced vitreoretinal surgeon who had practiced for 12 years. The baby was followed-up with a 2- to 5-day interval until the plus disease and extraretinal fibrovascular proliferation (EFP) had disappeared. Plus signs and EFP were regressed within 3 weeks after the injection of bevacizumab. After complete regression, the patient was examined every 2 weeks till the second post-treatment month and the retina of both eyes remained stable. When he returned to the former facility 3 months past the use of bevacizumab, the left eye developed a tractional detachment of retina. When he was transferred to SNUCH at postnatal age 5 months, the left eye had already developed total retinal detachment with centripetal contraction and the right eye showed a regression of ROP and sufficient laser scars. However, a thin vitreoretinal traction band without vascular component was observed along the major vascular arcades of his right eye. The retina of right eye remained stable during the first 2 weeks and abruptly progressed to subtotal retinal detachment within the next 2 weeks (4 months after the bevacizumab injection).
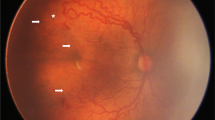
Morphologically, TRD developed in his right eye was different from the typical characteristics of TRD in ROP. Previous thin vitreoretinal traction band along the major vascular arcades, which is not associated with neovascularization, progressed into a thick fibrous traction band resulting in a subtotal retinal detachment. Despite of phakic vitrectomy and delamination of membrane, the retina of his right eye had failed to accomplish a reattachment. During follow-ups, the detached retina of his left eye was dragged anteriorly and reached to the posterior lens surface (Figure 1).
Fundus photography of case 1: Thin vitreoretinal traction band without vascular component (arrow heads) arose along the major vascular arcade of the right eye 4 months after combination therapy of bevacizumab and laser ablation (a), and progressed insidiously during next 2 weeks (b). Sudden thickening of fibrous membrane and increased tension (arrow heads), which lead to tractional retinal detachment of inferior retina (arrows), were noted after another 2 weeks (c). Retina of the left eye showed to total retinal detachment with centripetal traction of neuro-sensory retina along the major vascular arcade (arrow heads) 4 months after combination therapy (d). Retinal detachment progressed during next 2 weeks (e), and the detached retina rolled-up anteriorly to just behind the lens after another 2 weeks (f).
Case 2
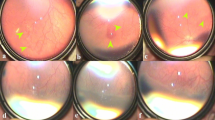
A male infant born at 30 weeks of gestation with a weight of 1370 g was referred to SNUCH for the management of stage 5 ROP. At gestational age 35 weeks, he received concomitant retinal photocoagulation and intravitreal injection of bevacizumab in both eyes due to zone I, stage 3 ROP with plus disease. Laser ablation covered the whole avascular retina in a confluent manner (intensity: 150–200 mW, OD: 1925 applications, OS: 1825 applications) by a paediatric ophthalmology specialist. A simultaneous injection of bevacizumab (0.75 mg, 0.03 ml) was performed. Four weeks past the combination therapy, EFP and plus disease of both eyes were completely regressed and the patient was recommended to have a follow-up exam 3 months later. When he returned to the former facility 4 months after treatment, total retinal detachment had developed in the right eye and thin fibrous traction band without vascular component was found along the major vascular arcades of the left eye. Traction band of the left eye was accompanied by retinal vascular avulsion and minor retinal folds, but not associated with retinal detachment. One month later, the traction band started to lose its tractional force from the temporal retina, and the retinal folds were flattened. On serial follow-up examinations, remnant traction band that caused retinal vascular avulsion was peeled spontaneously. He had one bout of vitreous haemorrhage during the process, but it was cleared within a month. Consequently, the traction membrane was peeled completely into the vitreous cavity within 12 months (Figure 2).
Fundus photography of case 2: Before treatment, both eyes showed stage 3 retinopathy of prematurity with severe plus disease in zone I (a and d). Extraretinal fibrovascular proliferation and plus disease were completely regressed 4 weeks after combined treatment (b). Four months past the treatment, total retinal detachment was found in the right eye (c) and a fibrous traction membrane with retinal vascular avulsion (arrow head) and minor retinal folds (arrow) was observed along the superotemporal retinal vascular arcade of the left eye (e). Twelve months after the treatment, the fibrous traction membrane was peeled spontaneously into the vitreous cavity (f).
Case 3
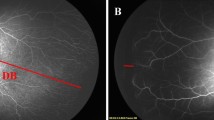
A male infant born at 28 weeks of gestation with a weight of 950 g was referred to SNUCH for the evaluation and management of fibrous tractional band following repeated bevacizumab injection. He received bevacizumab treatment (0.75 mg, 0.03 ml) for zone II posterior, stage 2 with plus disease, vitreous haemorrhage of both eyes at gestational age 35 weeks. Nine weeks later the first treatment, ROP of both eyes progressed to stage 3 with severe plus disease after a period of regression and he underwent second injection of bevacizumab (0.75 mg, 0.03 ml). Eleven weeks after the initial treatment, EFP and plus disease were regressed but a fibrous traction band was found along the superotemoral retinal vascular arcade of the right eye. ROP of his left eye was totally regressed without traction band formation. During 21 months of follow-up period, fibrous traction band of the right eye remained stable (Figure 3) and retarded peripheral vasculogenesis was noted in both eyes.
Discussion
Still there is no consensus on the safety, efficacy, and appropriate indication of bevacizumab use in patients with ROP. Although a retardation of normal vasculogenesis was noted,11 bevacizumab has been considered as a relatively safe and effective treatment modality for stage 3 ROP including zone I cases, regardless of the concomitant retinal photocoagulation.8, 11, 12, 13 However, the development or aggravation of TRD after bevacizumab injection had been reported in few cases of ROP. Most of these patients were intractable cases despite of previous retinal photocoagulation,5, 7, 8, 13 except for two cases of stage 3 ROP who had not received any retinal ablation before bevacizumab injection.14, 15 In the majority of cases, the deterioration of TRD occurred within a week after bevacizumab injection.5, 7, 8, 13 To our best knowledge, only two cases have been reported who showed delayed onset retinal detachment, which occurred 4 months after anti-VEGF treatment.15, 16 Among those patients the TRD started from the EFP, which was located at the margin of vascularized and non-vascularized retina without exception.
We experienced the development of atypical fibrous traction band, some of which lead to TRD in active stage 3 ROP patients who were treated with intravitreal injection of bevacizumab. Unlikely to the acute deterioration of previously noted cases, more than 2.5 months of latency between the bevacizumab injection and fibrous traction membrane formation was observed in our patients. Typically in ROP, new vessels bud from the retinal vessels just posterior to peripheral vascular shunt and vitreoretinal traction in those sites lead to the TRD. However in our cases, whitish fibrous traction membrane had arose along the major vascular arcades.
We should notice that the development and deterioration of atypical vitreoretinal traction band of these patients were quite unpredictable. In case 2, both eyes received a concomitant treatment with retinal photocoagulation and bevacizumab injection for zone I stage 3 ROP with plus disease and achieved symmetric regression within 4 weeks. However, the onset of traction band formation and the final anatomical result were quite different from each other. In case 3, although bevacizumab was applied on the same schedule for both eyes, focal fibrous traction band was developed only in the right eye. The onset of fibrous tractional band formation varies from 2.5 to 4 months after the initial bevacizumab injection. Preceding sign of regression and delayed onset of vitreoretinal traction could be the factors that have made clinicians inattentive to the possibility of disease progression.
In conclusion, late-onset fibrous traction band formation and subsequent TRD can occur after bevacizumab injection applied as an initial treatment in patient with active stage 3 ROP, which was considered as a relatively safe indication of bevacizumab. Moreover, these patients could have a relatively atypical feature such as vitreoretinal traction band along the major vascular arcade. Close follow-up is strongly recommended for at least 4 months after bevacizumab injection for stage 3 ROP even if the disease seems to have regressed.

References
Budd SJ, Thompson H, Hartnett ME . Association of retinal vascular endothelial growth factor with avascular retina in a rat model of retinopathy of prematurity. Arch Ophthalmol 2010; 128: 1014–1021.
Weidemann A, Krohne TU, Aguilar E, Kurihara T, Takeda N, Dorrell MI et al. Astrocyte hypoxic response is essential for pathological but not developmental angiogenesis of the retina. Glia 2010; 58: 1177–1185.
Lashkari K, Hirose T, Yazdany J, McMeel JW, Kazlauskas A, Rahimi N . Vascular endothelial growth factor and hepatocyte growth factor levels are differentially elevated in patients with advanced retinopathy of prematurity. Am J Pathol 2000; 156: 1337–1344.
Sato T, Kusaka S, Shimojo H, Fujikado T . Simultaneous analyses of vitreous levels of 27 cytokines in eyes with retinopathy of prematurity. Ophthalmology 2009; 116: 2165–2169.
Lalwani GA, Berrocal AM, Murray TG, Buch M, Cardone S, Hess D et al. Off-label use of intravitreal bevacizumab (Avastin) for salvage treatment in progressive threshold retinopathy of prematurity. Retina 2008; 28 (3 Suppl): 13–18.
Quiroz-Mercado H, Martinez-Castellanos MA, Hernandez-Rojas ML, Salazar-Teran N, Chan RV . Antiangiogenic therapy with intravitreal bevacizumab for retinopathy of prematurity. Retina 2008; 28 (3 Suppl): 19–25.
Honda S, Hirabayashi H, Tsukahara Y, Negi A . Acute contraction of the proliferative membrane after an intravitreal injection of bevacizumab for advanced retinopathy of prematurity. Graefes Arch Clin Exp Ophthalmol 2008; 246: 1061–1063.
Kusaka S, Shima C, Wada K, Arahori H, Shimojyo H, Sato T et al. Efficacy of intravitreal injection of bevacizumab for severe retinopathy of prematurity: a pilot study. Br J Ophthalmol 2008; 92: 1450–1455.
Lee JY, Chae JB, Yang SJ, Yoon YH, Kim JG . Effects of intravitreal bevacizumab and laser in retinopathy of prematurity therapy on the development of peripheral retinal vessels. Graefes Arch Clin Exp Ophthalmol 248: 1257–1262.
Chung EJ, Kim JH, Ahn HS, Koh HJ . Combination of laser photocoagulation and intravitreal bevacizumab (Avastin) for aggressive zone I retinopathy of prematurity. Graefes Arch Clin Exp Ophthalmol 2007; 245: 1727–1730.
Mintz-Hittner HA, Kuffel RR . Intravitreal injection of bevacizumab (avastin) for treatment of stage 3 retinopathy of prematurity in zone I or posterior zone II. Retina 2008; 28: 831–838.
Mintz-Hittner HA, Kennedy KA, Chuang AZ . Efficacy of intravitreal bevacizumab for stage 3+ retinopathy of prematurity. N Engl J Med 2011; 364: 603–615.
Wu WC, Yeh PT, Chen SN, Yang CM, Lai CC, Kuo HK . Effects and complications of bevacizumab use in patients with retinopathy of prematurity: a Multicenter Study in Taiwan. Ophthalmology 2011; 118: 176–183.
Zepeda-Romero LC, Liera-Garcia JA, Gutierrez-Padilla JA, Valtierra-Santiago CI, Cardenas-Lamas LJ . Paradoxical vascular-fibrotic reaction after intravitreal bevacizumab for retinopathy of prematurity. Eye (Lond) 2010; 24: 931–933.
Jang SY, Choi KS, Lee SJ . Delayed-onset retinal detachment after an intravitreal injection of ranibizumab for zone 1 plus retinopathy of prematurity. J AAPOS 2010; 14: 457–459.
Suk KK, Berrocal AM, Murray TG, Rich R, Major JC, Hess D et al. Retinal detachment despite aggressive management of aggressive posterior retinopathy of prematurity. J Pediatr Ophthalmol Strabismus 2010; 47, Online 1–4.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Lee, B., Kim, J., Heo, H. et al. Delayed onset atypical vitreoretinal traction band formation after an intravitreal injection of bevacizumab in stage 3 retinopathy of prematurity. Eye 26, 903–910 (2012). https://doi.org/10.1038/eye.2012.111
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/eye.2012.111
Keywords
This article is cited by
-
Ocular complications following intravitreal bevacizumab injection for retinopathy of prematurity and assessment of risk factors
International Journal of Retina and Vitreous (2021)
-
Risk factors associated with avascular fibrous membrane in patients with retinopathy of prematurity
International Ophthalmology (2020)
-
Vitreous changes after intravitreal bevacizumab monotherapy for retinopathy of prematurity: a case series
International Journal of Retina and Vitreous (2018)
-
Allosteric regulation of pathologic angiogenesis: potential application for angiogenesis-related blindness
Archives of Pharmacal Research (2014)
-
Intravitreal injection of bevacizumab for retinopathy of prematurity
Japanese Journal of Ophthalmology (2014)