Abstract
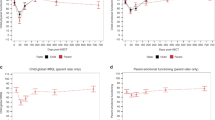
The purpose of this study was to examine longitudinally health-related quality of life (HRQOL) and related factors in mothers and fathers of children who undergo SCT, before, and 1 and 2 years after SCT. A total of 84 parents (49 mothers/35 fathers) of patients diagnosed mainly with leukemia completed a HRQOL measure before SCT, 46 at 1 year (26 mothers/20 fathers) and 50 parents (31 mothers/19 fathers) at 2 years post SCT. Physical and psychosocial HRQOL summary scores are reported. Parents’ age and gender, child's diagnosis, radiation history, age, behavior and physical health were examined. Linear mixed models for repeated measures with a covariate structure were used for analysis. Physical HRQOL did not differ between mothers and fathers or over time. Maternal and paternal psychosocial HRQOL scores improved by 2 years post SCT. Child's behavior problems and poor health, and maternal age (younger) predicted poor maternal psychosocial HRQOL 2 years post SCT. Child's behavior problems, diagnosis and treatment severity predicted poor paternal psychosocial HRQOL. These findings identify similar (child's poor behavior) and differential risk factors (parental young age, disease and treatment severity, and child's poor health status) for poor HRQOL for mothers and fathers. These findings can guide comprehensive family-care interventions before, during and after pediatric SCT.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
Guinan E, Krance R, Lehmann L. Stem cell transplantation in pediatric oncology. In: Pizzo P, Poplack D (eds). Principles and Practice of Pediatric Oncology, 4th edn. Lippincott Williams & Wilkins: Philadelphia, PA, 2002, pp 429–451.
Barrera M, Atenafu E, Hancock K . Longitudinal health-related quality of life outcomes and related factors after pediatric SCT. Bone Marrow Transplant 2009; 44: 249–256.
Barrera M, Atenafu E, Pinto J . Behavioral, social and educational outcomes after pediatric stem cell transplantation and related factors. Cancer 2009; 115: 880–889.
Clarke N, McCarthy M, Downie P, Ashley D, Anderson V . Gender differences in the psychosocial experience of parents of children with cancer: a review of the literature. Psychooncology 2009; 18: 907–915.
Vrijmoet-Wiersma CM, Kolk AM, Grootenhuis MA, Spek EM, van Klink JM, Egeler RM et al. Child and parental adaptation to pediatric stem cell transplantation. Support Care Cancer 2009; 17: 707–714.
Hatzmann J, Heymans HS, Ferrer-i-Carbonell A, van Praag BM, Grootenhuis MA . Hidden consequences of success in pediatrics: parental health-related quality of life—results from the Care Project. Pediatrics 2008; 122: 1030–1038.
Klassen A, Klassen R, Dix D, Pritchard S, Yanofsky R, O’Donnell M et al. Impact of caring for a child with cancer on parents’ health-related quality of life. J Clin Psychol 2008; 26: 5884–5889.
Eiser C, Eiser JR, Stride CB . Quality of life in children newly diagnosed with cancer and their mothers. Health Qual Life Outcomes 2005. http://www.hqlo.com/content/3/1/29.
Kazak AE, Barakat LP . Brief report: Parenting stress and quality of life during treatment for childhood leukemia predicts child and parent adjustment after treatment ends. J Pediatr Psychol 1997; 22: 749–758.
Vrijmoet-Wiersma CM, Egeler RM, Koopman HM, Lindahl Norberg A, Grootenhuis MA . Parental stress before, during and after pediatric stem cell transplantation: a review article. Support Care Cancer 2009; 17: 1435–1443.
Phipps S, Dunavant M, Lensing S, Rai SN . Psychosocial predictors of distress in parents of children undergoing stem cell or bone marrow transplantation. J Pediatr Psychol 2005; 30: 139–153.
Forinder U . Bone marrow transplantation from a parental perspective. J Child Health Care 2004; 8: 134–148.
Manne S, DuHamel K, Ostroff J, Parsons S, Martini R, Williams SE et al. Anxiety, depressive and posttraumatic stress disorder among mothers of pediatric survivors of hematopoietic stem cell transplantation. Pediatrics 2004; 113: 1700–1708.
Rini C, Manne S, DuHamel K, Austin J, Ostroff J, Boulad F et al. Mothers’ perceptions of benefit following pediatric stem cell transplantation: a longitudinal investigation of the roles of optimism, medical risk and socio-demographic resources. Ann Behav Med 2004a; 28: 132–141.
Rini C, Manne S, DuHamel K, Austin J, Ostroff J, Boulad F et al. Changes in mothers’ beliefs following a child's bone marrow transplantation: the role of prior trauma and negative life events. J Trauma Stress 2004b; 17: 325–333.
Rodrigue JR, MacNaughton K, Hoffmann RG, Graham-Pole J, Andres JM, Novak DA et al. Transplantation in children: a longitudinal assessment of mothers’ stress, coping and perceptions of family functioning. Psychosomatics 1997; 38: 478–486.
Barrera M, Pringle L, Sumbler K, Saunders F . Quality of life and behavioral adjustment after pediatric bone marrow transplantation. Bone Marrow Transplant 2000; 26: 427–435.
Sormanti M, Dungan S, Rieker P . Pediatric bone marrow transplantation: psychosocial issues for parents after a child's hospitalization. J Psychosoc Oncol 1994; 12: 23–42.
Barrera M, D’Agostino N, Gibson J, Gilbert T, Weksberg R, Malkin D . Predictors and mediators of psychological adjustment in mothers of children newly diagnosed with cancer. Psychooncology 2004; 13: 630–641.
Lindahl Norberg A, Lindblad F, Boman KK . Coping strategies in parents of children with cancer. Soc Sci Med 2005; 60: 965–975.
Barrera M, Atenafu E, Doyle J, Berlin-Romalis D, Hancock K . Differences in mothers’ and fathers’ psychological distress after pediatric stem cell transplant: a longitudinal study. Bone Marrow Transplant 2011 (in press).
Ware J, Sherbourne C . The MOS 36-item short-form health survey (SF-36): conceptual framework and item selection. Med Care 1992; 30: 473–483.
Achenbach T. . Manual for the Child Behavior Checklist/4–18 and 1991 Profile. University of Vermont Department of Psychiatry: Burlington, VT, 1991.
Achenbach T, Edelbrock C . The child behavior profile: II. Boys aged 6–12 and girls aged 6–11 and 12–16. J Consult Clin Psychol 1983; 47: 223–233.
Landgraf J, Abetz L, Ware J . Child Health Questionnaire (CHQ): A Users’ Manual. The Health Institute: Boston, MA, 1996.
Norman G, Sloan J, Wyrwich K . Interpretation of changes in health-related quality of life: the remarkable universality of a half a standard deviation. Med Care 2003; 41: 582–592.
Bonnano AG, Mancini AD . The human capacity to thrive in the face of potential trauma. Pediatrics 2008; 121: 369–375.
Park CL, Helgeson VS . Growth following highly stressful events: current status and future directions. J Consult Clin Psychol 2006; 74: 791–796.
Rubenstein C, Varni J, Katy E . Cognitive functioning in long-term survivors of childhood leukemia: a prospective analysis. J Dev Behav Pediatr 1990; 11: 301–305.
Palmer S, Goloubeva O, Reddick W, Glass J, Gajjar A, Kun L et al. Patterns of intellectual development among survivors of pediatric medulloblastoma: a longitudinal analysis. J Clin Oncol 2001; 19: 2302–2308.
Acknowledgements
We thank Karen Sumbler, Tara Smith and Gail Andrews for their help in collecting data for this study, and Jennifer Pinto for her assistance in the preparation of the manuscript. This research was supported by grants from the Hospital for Sick Children Foundation, New Initiatives; Elizabeth Lue Bone Marrow Foundation; and the National Cancer Institute of Canada.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Barrera, M., Atenafu, E., Doyle, J. et al. Differences in mothers’ and fathers’ health-related quality of life after pediatric SCT: a longitudinal study. Bone Marrow Transplant 47, 855–859 (2012). https://doi.org/10.1038/bmt.2011.190
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/bmt.2011.190
Keywords
This article is cited by
-
The impact of pediatric blood and marrow transplant on parents: introduction of the parent impact scale
Health and Quality of Life Outcomes (2015)