Abstract
The repair of an abdominal aortic aneurysm (AAA) is a high-risk surgical procedure related to hormonal and metabolic stress-related response with an ensuing activation of the inflammatory cascade. In contrast to open repair (OR), endovascular aortic aneurysm repair (EVAR) seems to decrease the postoperative stress by offering less extensive incisions, dissection, and tissue manipulation. However, these beneficial effects may be offset by the release of cytokines and arachidonic acid metabolites during intra-luminal manipulation of the thrombus using catheters in endovascular repair, resulting in systemic inflammatory response (SIR), which is clinically called post-implantation syndrome. In this systematic review we compared OR with EVAR in terms of the post-interventional inflammatory response resulting from alterations in the circulating cytokine levels. We sought to summarize all the latest evidence regarding post-implantation syndrome after EVAR. We searched Medline (PubMed), ClinicalTrials.gov and the Cochrane library for clinical studies reporting on the release of cytokines as part of the inflammatory response after both open/conventional and endovascular repair of the AAA. We identified 17 studies examining the cytokine levels after OR versus EVAR. OR seemed to be associated with a greater SIR than EVAR, as evidenced by the increased cytokine levels, particularly IL-6 and IL-8, whereas IL-1β, IL-10 and TNF-α showed conflicting results or no difference between the two groups. Polyester endografts appear to be positively correlated with the incidence of post-implantation syndrome after EVAR. Future large prospective studies are warranted to delineate the underlying mechanisms of the cytokine interaction in the post-surgical inflammatory response setting.
Similar content being viewed by others
Introduction
The repair of an abdominal aortic aneurysm (AAA) is a high-risk surgical procedure related to hormonal and metabolic stress-related responses, with an ensuing activation of the inflammatory cascade1. A systemic inflammatory response (SIR) is caused by both the surgical trauma and ischemia-reperfusion injury2 related to aortic clamping3,4,5,6 and by local cellular interactions arising at the blood/biomaterial interface7,8.
In contrast to open repair (OR), endovascular aortic aneurysm repair (EVAR) seems to decrease the postoperative stress by offering less extensive incisions, dissections, and tissue manipulation. However, these beneficial effects may be offset by the release of cytokines and arachidonic acid metabolites due to the intra-luminal manipulation of the thrombus by catheters during the endovascular repair, resulting in SIRS and its manifestation after endograft placement and interaction with the aortic endothelium, which is clinically called post-implantation syndrome9. The inflammatory response is important for tissue repair and has a profound effect on homeostasis due to release of catabolic stress hormones and the interference with immune function, which delays wound healing and increases the risk of sepsis10,11. Recently, postoperative IL-6 and CRP levels were reported to correlate with the magnitude of operative injury and the invasiveness of the operative procedure11.
Contributors to the surgical stress after open repair include laparotomy and ischemia-reperfusion injury after aortic cross-clamping12. During OR, the aorta may be approached either transabdominally or through the retroperitoneal space. Depending on the anatomy, the aorta can be reconstructed with a tube graft, an aortic iliac bifurcation graft, or an aortofemoral bypass. For proximal infrarenal control, the first step is to identify the left renal vein. If significant intraluminal debris, juxtarenal thrombus, or prior peripheral embolization is present, the distal arteries are clamped first, followed by aortic clamping9.
With respect to pelvic outflow, the inferior mesenteric artery is sacrificed in most instances12. Therefore, to prevent colon ischemia, every attempt must be made to restore the perfusion from at least one hypogastric (internal iliac) artery. If the hypogastric arteries are sacrificed (eg, because of associated aneurysms), the inferior mesenteric artery should be reimplanted. The aorta is reconstructed from within by using a polytetrafluoroethylene (PTFE) or Dacron graft. The aneurysm sac is closed, and the graft is placed into the duodenum to prevent erosion. Before the restoration of the lower-extremity blood flow, both forward flow (aortic) and backflow (iliac) are allowed to remove debris. The graft is also irrigated to flush out the debris12.
Endovascular repair of an AAA involves gaining access to the lumen of the abdominal aorta, usually via small incisions over the femoral vessels13. An endograft, typically a polyester or Gore-Tex graft with a stent exoskeleton, is placed within the lumen of the AAA, extending distally into the iliac arteries. The graft serves to contain aortic flow and decrease the pressure on the aortic wall, leading to a reduction in the AAA size over time and a decrease in the risk of aortic rupture14.
The aim of this systematic review was to compare OR and EVAR in terms of the post-interventional inflammatory response as yielded by the alterations in the circulating cytokine levels. Ultimately, we sought to summarize all the latest evidence regarding post-implantation syndrome after EVAR.
Material and methods
Search strategy, data sources and eligibility criteria
This systematic review followed the guidelines proposed by the Preferred Reporting Items for Systematic reviews and Meta-Analysis (PRISMA) guidelines (Supplementary Table S1)15. A predetermined study protocol was agreed upon and was strictly followed by all the authors. The identification of the eligible studies was performed using three distinct databases through November 2nd, 2017; Medline (PubMed), ClinicalTrials.gov and the Cochrane library. The following algorithm was applied: “((surgical stress) OR cytokines OR interleukin OR (systemic inflammatory response)) AND (abdominal aortic aneurysm) AND ((open OR endovascular OR conventional) AND (repair OR surgery))”. Two independent reviewers (Diamantis I TSILIMIGRAS, Demetrios MORIS) screened all the articles yielded by the aforementioned algorithm. The reference lists of the eligible studies were manually assessed in order to detect any potential relevant article (“snowball” procedure).
Inclusion and exclusion criteria
Only clinical studies reporting on the cytokines released as part of the inflammatory response after both open/conventional and endovascular repair of the AAA were considered eligible. No study sample size restriction was applied. The exclusion criteria were as follows: 1) studies reporting on the repair of aneurysms other than abdominal, 2) studies reporting on either open or endovascular alone AAA repair without comparing the two approaches, 3) non-English studies, 4) animal studies, 5) reviews, 6) editorials and letters to the editors and 7) overlapping studies.
Data extraction and tabulation
Two independent authors (Diamantis I TSILIMIGRAS, Demetrios MORIS) reviewed the full-texts of the eligible studies, extracted the data and cross-checked all the results. In particular, the variables extracted included the general study characteristics (eg, author, year of publication, study design, number of patients pertaining to the OR and EVAR groups), the patient demographics (eg, age and gender), and cytokine alterations. In the case of data discrepancies, the authors reached a consensus by discussion.
Results and discussion
Search results and study characteristics
The initial search algorithm yielded 412 records. Following the screening of the titles and abstracts, 78 clinical studies were retrieved for the full-text evaluation. Fifteen studies were deemed eligible, while two were identified from the “snowball” procedure, resulting in a total of 17 studies examining the cytokine levels after OR versus EVAR16,17,18,19,20,21,22,23,24,25,26,27,28,29,30,31,32 (Figure 1). All the studies were prospective, incorporating a total of 530 patients with 245 (46.2%) patients undergoing OR and 285 (53.8%) undergoing EVAR. Various cytokines were examined as biomarkers of the post-interventional inflammatory response, including IL-1β, IL-2, IL-6, IL-8 and TNF-α. However, the vast majority of the available studies (14 out of 17) focused on the role of IL-616,17,18,19,20,21,22,23,24,25,27,29,31,32 followed by TNF-α (7 out of 17)10,19,21,22,25,29,31,32. The demographics of the eligible studies along with the cytokines under investigation are listed in Table 1.
Operation causes the activation of inflammatory cascade
It has long been recognized that injury to the body, either from trauma or from operative procedures causes a stereotypical cascade of neuroendocrine, cytokine, acute phase and metabolic responses33. Within minutes after uncomplicated elective operative injury, activation of the sympathetic nervous system occurs, resulting in increased secretion of catecholamines (epinephrine and norepinephrine) into the circulation, which leads to tachycardia, hypertension, fever and tachypnea1. At the same time, there is also an increased secretion of the pituitary hormones, such as corticotrophin (ACTH), growth hormone (GH) and arginine vasopressin (AVP). ACTH acts on the adrenal cortex to stimulate cortisol secretion, peaking at approximately 4–6 h after the operative injury, whereas AVP affects the kidney and fluid balance1.
Subsequently, there is an increase in the production of pro-inflammatory cytokines, such as tumor necrosis factor alpha (TNF-α), interleukin (IL)-1 beta, IL-8, IL-12, IL-18, and in particular, IL-634. It has been suggested that IL-6 peaks at approximately 18–24 h after operative injury. These cytokines are produced in response to injury by many cells throughout the body and form a complex signaling system for the subsequent production of acute phase proteins from the liver and increase the stimulation of myeloid tissue35,36,37. Changes in circulating myeloid cells occur, particularly by increasing white blood cells (WBC), which are dominated by neutrophils as well as the increased numbers of myeloid-derived suppressor cells and platelets. In addition, there seem to be changes in the plasma concentrations of a number of acute phase proteins, particularly C-reactive protein (CRP)38, which peaks at approximately 48–72 h39.
Basic principles about open and endovascular repair of AAA
For many years, OR was the mainstay of treatment for the management of AAA. Due to the significant related risk of morbidity and death40, EVAR was introduced in 199141 as a less invasive procedure of transfemoral AAA management. Apart from the advantages over OR in terms of the reduced mortality and morbidity rates42, EVAR is also associated with restricted perioperative hemodynamic parameter fluctuations43,44.
Differences in the postoperative stress response between EVAR and OR have been demonstrated in many studies with different underlying mechanisms pertaining to each approach27,45. In general, it is thought that EVAR is associated with a less intense and extensive inflammatory response and cytokine release32,46, less tissue damage, ischemia-reperfusion insult and subsequent inflammatory events. On the other hand, it has also been mentioned that endoluminal procedures may elicit an unexpected systemic inflammatory response29,47, which is also called post-implantation syndrome (PIS).
The length of the operation has long been recognized as predictive of the increased activation of the stress response, irrespective of the anesthetic method. Operations lasting more than 5 h are characterized by significantly higher CRP, IL-1β, IL-6, and TNF-α levels (P<0.05) at 12 and 24 h postoperatively than those lasting less than 4 h48, which is normally the case in AAA repair. Thus, post-surgical stress may be ameliorated with minimally invasive procedures, such as EVAR. Clarifying the pathophysiology behind the aortic aneurysm repair-related surgical stress facilitates the establishment and the application of Stress Scales that could predict the postoperative course after an AAA repair in terms of the morbidity, mortality and length of hospital stay12. Table 2 summarizes the differential release of cytokines in the AAA repair-induced surgical stress based on the treatment approach (OR versus EVAR).
Interleukin-8 (IL-8)
IL-8 is a pro-inflammatory cytokine that plays a definite role in the regulation of neutrophil recruitment and migration49. IL-8 has a lower peak than IL-6 at 2–4 h after clamp removal during thoracoabdominal AAA repair50,51. Parodi et al26 found that IL-8 levels increased immediately after OR and fell by 72 h, although not to preoperative levels. IL-8 levels were higher in the OR group than the EVAR group even on the 7th postoperative day (P=0.02)28. Rowland et al found that IL-8 levels peaked earlier than those of IL-6 (at 4 h after clamp removal), showing a faster decline in the EVAR group (at 72 h after clamp removal: OR=35 pg/mL and EVAR: 16 pg/mL, P=0.001)27. Interestingly, however, older studies showed no difference between the two groups in terms of the IL-8 levels22,24,29.
Interleukin-10 (IL-10)
IL-10 acts as an anti-inflammatory as well as a coagulation inhibitory cytokine, which counterbalances or regulates the pro-inflammatory response52. IL-10 exhibits pluripotent anti-inflammatory properties by both inhibiting TNF-α and IL-1 synthesis and antagonizing their actions through the up-regulation of cytokine antagonists53. In cases of major traumatic injury, an increased IL-10 production, in combination with decreased IFN-γ and IL-12, correlates with cellular immunity suppression54. Thus, the systemic release of IL-10, triggered by sympathetic nervous system activation, might be a key mechanism of the immunosuppression observed after injury, which predisposes patients to the development of infections55.
Given that AAA repair provokes a major tissue trauma, these interactions may explain the mechanism of wound infection. It has been shown that IL-10 levels peak during the ischemic phase in aneurysm surgical repair, while returning to baseline during visceral perfusion56 and, therefore, presents with a biphasic pattern57. Among the studies examining the differences in the cytokine release between OR and EVAR, none found significant differences between the two approaches16,27,30. IL-10 levels were comparable at 0 h, 4 h, 24 h, 72 h and 144 h after clamp removal27. Interestingly, after elective AAA repair, high levels of IL-10 were associated with both prolonged critical care (P<0.001) and hospital stay (P=0.001)58.
Interleukin-6 (IL-6)
Among all the cytokines, IL-6 has been at the forefront of the studies examining the postoperative inflammatory response after OR or EVAR16,17,18,19,20,21,22,23,24,25,27,29,31,32 (Table 2). IL-6 release follows the same pattern as other acute phase cytokines (TNF-α, IL-1 and IL-10) and peaks between 4 and 48 h after clamp removal31. However, it demonstrates the most pronounced increase and thus is supposed to reflect the intensity of the surgical trauma following AAA repair2,58. Several clinical studies have suggested that the major source of IL-6 following AAA repair may be the splanchnic system rather than the lower limb59. It has been hypothesized that IL-6 uptake through the liver may be preserved in cases of sufficient visceral organ protection56,60. Thus, a persistent rise in IL-6 levels in the postoperative period may be a valuable predictor of serious complications3,61.
Most reports (8 out of 14 eligible studies) have advocated the higher IL-6 release following OR when compared to the EVAR approach16,18,19,21,25,27,29,31. It has been suggested that the production of IL-6 in OR should be attributed to tissue damage (caused by ischemia-reperfusion injury and surgical insult) or blood transfusion, whereas IL-6 release in EVAR may be caused by manipulations into the aneurysmal thrombus22. IL-6 levels peak between 4 and 48 h postoperatively with OR, inducing a higher IL-6 response16,18,19,21,25,29,31, and IL-6 is present even on the 6th postoperative day (POD)27.
In contrast, Galle et al revealed similar IL-6 release patterns between the OR and EVAR, demonstrating the involvement of IL-6 in the inflammation process in both procedures22. The same results were obtained by two other studies at 5 min, 60 min, 24 h and 48 h postoperatively17,32, whereas Dawson et al and Morikage et al revealed lower concentrations of circulating IL-6 with OR compared to EVAR (P=0.03) and unrepaired AAA (P=0.025)20,24.
Recently, Makar et al23 investigated the SIRS following EVAR and OR in the ruptured AAA setting. They found that IL-6 decreased in both groups after surgery, reaching parity on the POD523. The peak IL-6 was significantly higher in the OR group (25.1 (17.2–50.9 pg/mL)) than in the EVAR group (14.2 (7.1–29.8 pg/mL; P=0.04))23. However, the IL-6 levels were similar at the individual time points (6 h, POD1, POD3, POD5) in both groups. Interestingly, previous studies have associated the high IL-6 levels with the development of multi-organ failure in cases of AAA rupture (P=0.01)58,62. In a recent systematic review by Watt et al, OR presented a peak value of IL-6 at the level of 332 pg/mL compared to the 116 pg/mL seen in EVAR11.
Interleukin-1β and TNF-α
Calogero et al63 demonstrated that IL-l concentrations increase mainly during periods of major surgical manipulation with a second surge at the emergence from general anesthesia and during the postoperative recovery period. Only 4 studies examined the differential release of IL-1β in the OR versus EVAR group16,19,29,32. It has been largely suggested that IL-1β levels exhibit no differences between the two groups16,19,29, with the highest intraoperative IL-1β levels recorded 60 min after clamp removal29. Only Thompson et al found a lower increase in IL-1β and TNF-α levels from baseline with EVAR compared to OR32.
TNF-α enhances vascular permeability through both neutrophil-dependent and neutrophil-independent mechanisms64, and high TNF-α levels have been correlated with poor outcomes after OR3,61,65. Some studies revealed a more pronounced TNF-α release in OR versus EVAR19,21,31,32. In contrast, two other studies22,25 reported no significant changes in TNF-α after EVAR or OR. Of note, Swartbol et al described TNF-α release only in the EVAR group29. Other observations about EVAR19,29,47 described a TNF-α response associated with a clinically relevant drop in blood pressure or as a consequence of leukocyte activation triggered by IL-6 release from the aneurysmal thrombus during manipulations66. These findings indicate that surgical stress alone does not normally produce TNF-α. Hemorrhage or shock, such as in case of a ruptured AAA, are related to significant increases in TNF-α, whereas only modest elevations if none are detected following uncomplicated elective AAA repair2,51,67. High TNF-α levels are also correlated with renal or other organ dysfunction3,58,68 and a higher mortality (P=0.01)57,69.
The role of the material in the postimplantation syndrome
Patients undergoing EVAR for AAA often develop an inflammatory response, called postimplantation syndrome (PIS), that is associated with fever and leukocytosis70. The reported incidence of PIS in the literature varies widely from 14% to 60%13,71. PIS constitutes a SIRS state, as it actually fulfills at least two of the SIRS criteria (fever and leukocytosis)72. However, hs-CRP values have also been strongly related to the presence of PIS and emerged as an important predictor of the 30-day outcome9.
The endograft type appears to influence the incidence of SIR after EVAR. PIS is mainly apparent during the first 24 h and decreases afterward. Anaconda and Zenith endografts are thought to induce a more intense inflammatory response. A "milder" inflammatory activation was observed in patients with an Excluder endograft14. PIS is not associated with perioperative adverse clinical events, showing a benign course. Moulakakis et al14 compared the variability of PIS throughout different the endograft types and concluded that the mean elevated temperature was more pronounced postoperatively in the Anaconda group, whereas all the grafts caused a significant increase in the serum levels of IL-6 and IL-10 postoperatively compared with the preoperative levels. The Excluder group showed the smallest increase in the levels of serum IL-6 and IL-10 at 24 h and 48 h, postoperatively14. The mean differences in the cytokine levels after aneurysm exclusion were greater for the Anaconda versus the Excluder group (P<0.01) than for the Anaconda versus Zenith group (P<0.05). No differences in the mortality and morbidity rates were observed among the four groups14. Another study also reached the conclusion that PIS is a benign complication after EVAR using the Anaconda endograft, mainly affecting the length of the in-hospital stay and the daily physical activities of the patients with PIS73.
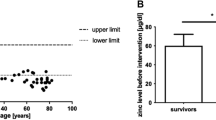
Differences between the type of the stent graft deployed and the development of PIS might indicate that different materials, and maybe configurations of the grafts, interfere with the inflammatory response. Stent grafts are a collapsible hybrid product composed of either woven Dacron or ePTFE with stents providing radial support. In 2005, Gerasimidis et al74, in a relatively underpowered study, found, for the first time, that fever was more common in a group of patients who received polyester endovascular grafts than in those who received the PTFE graft. IL-8 was higher in the first group, suggesting a stronger host reaction to the specific material74. VoÛte et al75, in a later study, showed that the implantation of the stent grafts based on polyester was independently associated with a stronger inflammatory response. Arnaoutoglou et al9 found that the use of a polyester endograft independently predicted PIS and was correlated with a greater than 10 times higher risk for an inflammatory response. Based on the results of the 3 studies mentioned above, the type of endograft material seems to play a principle role in PIS development and may have a predictive role for a significant portion of EVAR patients. Arnaoutoglou et al9 evaluated the characteristics of PIS in patients after EVAR, showing that preoperative WBC count values (P<0.001), polyester endograft material (P<0.001) and heart failure (P=0.03) were independent predictors of PIS. Postoperative hs-CRP (P=0.001) and the duration of fever (P=0.02) independently predicted the occurrence of a major cardiovascular event (MACE). A threshold of postoperative hs-CRP value of 125 mg/L was highly associated with the occurrence of a MACE, with a sensitivity of 82% and a specificity of 75%9.
Furthermore, there are other differences between stent grafts, unrelated to graft material, which theoretically might also influence PIS occurrence. The vast majority of the stent grafts have an exoskeleton made of nitinol. Since the presentation of nitinol for medical application, it has been extensively used in coronary and peripheral arterial stents. No inflammatory response is reported in these applications, despite the frequent treatment of multiple and lengthy lesions, requiring large quantities of the material. It is, therefore, doubtful that variances in the application of nitinol between stent grafts have any effect on PIS13.
Finally, the Nellix EndoVascular Aneurysm Sealing (EVAS) System (Endologix, Inc, Irvine, CA, USA) is a novel approach to AAA treatment, whereby a polymer is used to fill the AAA sac. A recent study demonstrated that the incidence of postimplantation syndrome (P=0.07), the mean body temperature (P=0.05), the mean leukocyte count (P=0.003), and the mean hs-CRP (P<0.001) were proportionally lower with EVAS than with EVAR. Serious adverse events (0% vs 12.8%, P=0.05) and endoleaks (0% vs 10.3%, P=0.13) over 30 days were less frequent with EVAS, but the differences between the groups were not significant76. The choice of endovascular graft material influenced the postoperative and 30-day clinical outcomes, with a greater overall risk observed with the polyester stent-grafts76.
Opinion
Major surgical procedures-such as AAA repair-often lead to severe immunosuppression, which in turn may contribute to infectious complications and sepsis. Strong stimulation of the sympathetic/adrenomedullary system (SNS) and the hypothalamic–pituitary–adrenal (HPA) axis correlates with the severity of the surgical injury and poor prognosis77. Corticotropin acts on the adrenal cortex to stimulate cortisol secretion, peaking at approximately 4–6 h after operative injury77. The simultaneous activation of these two systems allows the organism to adapt and maintain or regain homeostasis during the stress of the perioperative period. The perioperative imbalance between Th1 and Th2 cytokines has been suggested as a mechanism of the immune suppression after surgery78. Briefly, Th1 cytokines, such as TNF-α, IL-2 and IL-12, are highly effective at enhancing immune surveillance. By contrast, Th2 cytokines (IL-4, IL-5, IL-10, and IL-13) have a predominant immune suppressive effect79.
IL-6 demonstrates the most pronounced increase and reflects the intensity of surgical trauma following a major operation80. The increase in IL-6 levels is indicative of the activation of macrophages as antigen-presenting cells in a cell-mediated inflammatory response as well as the activation of endothelial cells, which is probably due to the endograft-aortic wall interaction. It is known that the major source of IL-6 following EVAR is the aneurysmal thrombus8. It appears to be involved in the pathogenesis of multiple-organ failure and is a potent inducer of fibrinogen production by hepatocytes77. It peaks at approximately 18–24 h after operative injury, and the more extensive the operation is, the greater is the magnitude of its circulating levels80. TNF-α is an essential component of the host immune response to trauma and is responsible for the release of other pro- and anti-inflammatory mediators77. In the study by Rettig et al, SIRS (systematic inflammatory response syndrome) and TNF-α, as a marker of this syndrome, does not seem to be associated with an increased risk of postoperative complications81. This might imply that the majority of the postoperative complications are the outcome of locally induced inflammatory responses rather than systemic ones. Moreover, the authors showed no correlation between TNF-α and IL-6 in patients with postoperative complications. This is different from findings of a recent study demonstrating that TNF-α levels were positively correlated with those of IL-6 levels in patients with postoperative sepsis82. Finally, despite the increased IL-6 levels after major surgery and the associated increased susceptibility to postoperative infections, the serum obtained postoperatively from patients after a major operation induces an immunosuppressive response reflected by the reduced MHC class II antigens reversible by IFN-γ through IL-6-independent pathways82. IL-10 acts as an anti-inflammatory cytokine that counterbalances the pro-inflammatory response. In cases of traumatic major injury, an increased production of IL-10 and a decreased production of IFN-γ and IL-12 correlate with cellular immunity suppression77. Thus, a high production of IL-10 could counterbalance the pro-inflammatory response induced by TNF-α and IL-6 and explain the decline in SIRS and IL-6 levels during the first 5 postoperative days after a major operation. Similarly, the evaluation of INF-γ, IL-2 and IL-8 levels suggests the involvement of the Th1 pathway of cell-mediated immunity (JAK-STAT and TLR pathway).
The possibility of a systematic response to endograft has been evaluated by TNF expression83, since it crosstalks with macrophages and causes a systematic inflammatory response, including fever, neutrophil and endothelial cell activation (TRADD-TRAF pathway). Similarly, the evaluation of INF-γ, IL-2 and CD40L levels indicate the involvement of the Th-1 pathway of cell-mediated immunity (JAK-STAT and TLR pathway) and T-dependent antibody production (CD40L). In the same frame, the expression of TGF-β acts as anti-inflammatory cytokine and indicates the counterbalance of the pro-inflammatory response of IL-6 and explains the deterioration of SIRS/PIS during the first 5 days after EVAR84.
A high expression of markers such as CCR7 and CD62L is indicative of immune memory and would be a striking finding, since it would imply that patients with PIS have already been exposed to antigens similar to endografts (mimicry) and thus demonstrate a more robust inflammatory response.
Figure 2 illustrates the proposed pathophysiology of the inflammatory response after AAA repair. A diagrammatic presentation of the main study findings is provided in Figure 3.
Study limitations
The present review has limitations mainly due to high heterogeneity of the included studies. The PIS definition varied throughout the literature. Moreover, the study populations were not similar, and the study design was not consistent in all the studies. There are not enough comparable studies evaluating cytokines in both OR and EVAR patients. Furthermore, the current trend in US centers for patients after EVAR includes discharge at POD1, which means that it is difficult to document PIS symptoms, which present after POD2 per the definition. The value of treating SIRS/PIS is underestimated in the literature since it is considered a benign homeostatic response to surgical stress. After the publication of a prospective study demonstrating that patients with PIS after EVAR had an increased risk of a MACE during the first year, the benign character of the syndrome as well as its management should be revisited. The current literature also lacks an understanding of the pathophysiology of the PIS. This is the reason why current studies fail to answer fundamental questions regarding the cytokines involved in the pathogenesis of PIS. The expression of these cytokines does not define the syndrome. They can only describe the syndrome, elucidate the immune mechanisms involved and facilitate therapeutic management.
Conclusions
In conclusion, OR is associated with a greater SIR compared to EVAR, as reflected by the increased cytokine levels, particularly IL-6 and IL-8. Circulating IL-6 might be an excellent marker of an inflammatory reaction and act as a useful predictive biomarker of postoperative morbidity. We suggest that a further, more detailed analysis of the postoperative immune response will contribute to the development of more accurate and sensitive predictive biomarkers for the postoperative morbidity of ΑΑΑ.
Polyester endografts are positively correlated with the incidence of post-implantation syndrome after EVAR. Future large prospective studies are warranted to delineate the underlying mechanisms of the cytokine interaction in the post-surgical inflammatory response setting.
References
Desborough JP. The stress response to trauma and surgery. Br J Anaesth 2000; 85: 109–17.
Swartbol P, Truedsson L, Norgren L. The inflammatory response and its consequence for the clinical outcome following aortic aneurysm repair. Eur J Vasc Endovasc Surg 2001; 21: 393–400.
Froon AH, Greve JW, Van der Linden CJ, Buurman WA. Increased concentrations of cytokines and adhesion molecules in patients after repair of abdominal aortic aneurysm. Eur J Surg 1996; 162: 287–96.
Groeneveld AB, Raijmakers PG, Rauwerda JA, Hack CE. The inflammatory response to vascular surgery-associated ischaemia and reperfusion in man: effect on postoperative pulmonary function. Eur J Vasc Endovasc Surg 1997; 14: 351–9.
Barry MC, Kelly C, Burke P, Sheehan S, Redmond HP, Bouchier-Hayes D. Immunological and physiological responses to aortic surgery: effect of reperfusion on neutrophil and monocyte activation and pulmonary function. Br J Surg 1997; 84: 513–9.
Welbourn CR, Goldman G, Paterson IS, Valeri CR, Shepro D, Hechtman HB. Pathophysiology of ischaemia reperfusion injury: central role of the neutrophil. Br J Surg 1991; 78: 651–5.
Tang L, Ugarova TP, Plow EF, Eaton JW. Molecular determinants of acute inflammatory responses to biomaterials. J Clin Invest 1996; 97: 1329–34.
Kakisis JD, Moulakakis KG, Antonopoulos CN, Mylonas SN, Giannakopoulos TG, Sfyroeras GS, et al. Volume of new-onset thrombus is associated with the development of postimplantation syndrome after endovascular aneurysm repair. J Vasc Surg 2014; 60: 1140–5.
Arnaoutoglou E, Kouvelos G, Papa N, Kallinteri A, Milionis H, Koulouras V, et al. Prospective evaluation of post-implantation inflammatory response after EVAR for AAA: influence on patients' 30 day outcome. Eur J Vasc Endovasc Surg 2015; 49: 175–83.
Arndt P, Abraham E. Immunological therapy of sepsis: experimental therapies. Intensive Care Med 2001; 27: S104–15.
Watt DG, Horgan PG, McMillan DC. Routine clinical markers of the magnitude of the systemic inflammatory response after elective operation: a systematic review. Surgery 2015; 157: 362–80.
Tang TY, Walsh SR, Fanshawe TR, Seppi V, Sadat U, Hayes PD, et al. Comparison of risk-scoring methods in predicting the immediate outcome after elective open abdominal aortic aneurysm surgery. Eur J Vasc Endovasc Surg 2007; 34: 505–13.
Arnaoutoglou E, Kouvelos G, Koutsoumpelis A, Patelis N, Lazaris A, Matsagkas M. An update on the inflammatory response after endovascular repair for abdominal aortic aneurysm. Mediators Inflamm 2015; 2015: 945035.
Moulakakis KG, Alepaki M, Sfyroeras GS, Antonopoulos CN, Giannakopoulos TG, Kakisis J, et al. The impact of endograft type on inflammatory response after endovascular treatment of abdominal aortic aneurysm. J Vasc Surg 2013; 57: 668–77.
Moher D, Liberati A, Tetzlaff J, Altman DG, Group P. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. J Clin Epidemiol 2009; 62: 1006–12.
Aho PS, Niemi T, Piilonen A, Lassila R, Renkonen R, Lepantalo M. Interplay between coagulation and inflammation in open and endovascular abdominal aortic aneurysm repair--impact of intra-aneurysmal thrombus. Scand J Surg 2007; 96: 229–35.
Barry MC, Hendriks JM, van Dijk LC, Pattynama P, Poldermans D, Bouchier Hayes D, et al. A comparative study of myocardial injury during conventional and endovascular aortic aneurysm repair: measurement of cardiac troponin T and plasma cytokine release. Ir J Med Sci 2010; 179: 35–42.
Bolke E, Jehle PM, Storck M, Braun C, Schams S, Steinbach G, et al. Endovascular stent-graft placement versus conventional open surgery in infrarenal aortic aneurysm: a prospective study on acute phase response and clinical outcome. Clin Chim Acta 2001; 314: 203–7.
Boyle JR, Goodall S, Thompson JP, Bell PR, Thompson MM. Endovascular AAA repair attenuates the inflammatory and renal responses associated with conventional surgery. J Endovasc Ther 2000; 7: 359–71.
Dawson JA, Choke E, Cockerill GW, Loftus IM, Thompson MM. The long-term effects of open and endovascular aneurysm repair on circulating interleukin-6. Eur J Vasc Endovasc Surg 2009; 37: 43–5.
Elmarasy NM, Soong CV, Walker SR, Macierewicz JA, Yusuf SW, Wenham PW, et al. Sigmoid ischemia and the inflammatory response following endovascular abdominal aortic aneurysm repair. J Endovasc Ther 2000; 7: 21–30.
Galle C, De Maertelaer V, Motte S, Zhou L, Stordeur P, Delville JP, et al. Early inflammatory response after elective abdominal aortic aneurysm repair: a comparison between endovascular procedure and conventional surgery. J Vasc Surg 2000; 32: 234–46.
Makar RR, Badger SA, O'Donnell ME, Soong CV, Lau LL, Young IS, et al. The inflammatory response to ruptured abdominal aortic aneurysm is altered by endovascular repair. Int J Vasc Med 2013; 2013: 482728.
Morikage N, Esato K, Zenpo N, Fujioka K, Takenaka H. Is endovascular treatment of abdominal aortic aneurysms less invasive regarding the biological responses? Surg Today 2000; 30: 142–6.
Odegard A, Lundbom J, Myhre HO, Hatlinghus S, Bergh K, Waage A, et al. The inflammatory response following treatment of abdominal aortic aneurysms: a comparison between open surgery and endovascular repair. Eur J Vasc Endovasc Surg 2000; 19: 536–44.
Parodi JC, Ferreira LM, Fornari MC, Berardi VE, Diez RA. Neutrophil respiratory burst activity and pro- and anti-inflammatory cytokines in AAA surgery: conventional versus endoluminal treatment. J Endovasc Ther 2001; 8: 114–24.
Rowlands TE, Homer-Vanniasinkam S. Pro- and anti-inflammatory cytokine release in open versus endovascular repair of abdominal aortic aneurysm. Br J Surg 2001; 88: 1335–40.
Shindo S, Kubota K, Kojima A, Matsumoto M. A comparison of the inflammatory response and the recovery of bowel function between trans- and extraperitoneal approaches of abdominal aortic aneurysmectomy. Int Angiol 2005; 24: 355–8.
Swartbol P, Norgren L, Albrechtsson U, Cwikiel W, Jahr J, Jonung T, et al. Biological responses differ considerably between endovascular and conventional aortic aneurysm surgery. Eur J Vasc Endovasc Surg 1996; 12: 18–25.
Sweeney KJ, Evoy D, Sultan S, Coates C, Moore DJ, Shanik DG, et al. Endovascular approach to abdominal aortic aneurysms limits the postoperative systemic immune response. Eur J Vasc Endovasc Surg 2002; 23: 303–8.
Syk I, Brunkwall J, Ivancev K, Lindblad B, Montgomery A, Wellander E, et al. Postoperative fever, bowel ischaemia and cytokine response to abdominal aortic aneurysm repair--a comparison between endovascular and open surgery. Eur J Vasc Endovasc Surg 1998; 15: 398–405.
Thompson MM, Nasim A, Sayers RD, Thompson J, Smith G, Lunec J, et al. Oxygen free radical and cytokine generation during endovascular and conventional aneurysm repair. Eur J Vasc Endovasc Surg 1996; 12: 70–5.
Cuthbertson DP. Second annual Jonathan E. Rhoads Lecture. The metabolic response to injury and its nutritional implications: retrospect and prospect. JPEN J Parenter Enteral Nutr 1979; 3: 108–29.
Marik PE, Flemmer M. The immune response to surgery and trauma: Implications for treatment. J Trauma Acute Care Surg 2012; 73: 801–8.
Bauer J, Herrmann F. Interleukin-6 in clinical medicine. Ann Hematol 1991; 62: 203–10.
Baigrie RJ, Lamont PM, Kwiatkowski D, Dallman MJ, Morris PJ. Systemic cytokine response after major surgery. Br J Surg 1992; 79: 757–60.
Gabay C, Kushner I. Acute-phase proteins and other systemic responses to inflammation. N Engl J Med 1999; 340: 448–54.
Cole DS, Watts A, Scott-Coombes D, Avades T. Clinical utility of peri-operative C-reactive protein testing in general surgery. Ann R Coll Surg Engl 2008; 90: 317–21.
Colley CM, Fleck A, Goode AW, Muller BR, Myers MA. Early time course of the acute phase protein response in man. J Clin Pathol 1983; 36: 203–7.
Berridge DC, Chamberlain J, Guy AJ, Lambert D. Prospective audit of abdominal aortic aneurysm surgery in the northern region from 1988 to 1992. Northern Vascular Surgeons Group. Br J Surg 1995; 82: 906–10.
Parodi JC, Palmaz JC, Barone HD. Transfemoral intraluminal graft implantation for abdominal aortic aneurysms. Ann Vasc Surg 1991; 5: 491–9.
May J, White GH, Yu W, Ly CN, Waugh R, Stephen MS, et al. Concurrent comparison of endoluminal versus open repair in the treatment of abdominal aortic aneurysms: analysis of 303 patients by life table method. J Vasc Surg 1998; 27: 213–20.
Baxendale BR, Baker DM, Hutchinson A, Chuter TA, Wenham PW, Hopkinson BR. Haemodynamic and metabolic response to endovascular repair of infra-renal aortic aneurysms. Br J Anaesth 1996; 77: 581–5.
Thompson JP, Boyle JR, Thompson MM, Strupish J, Bell PR, Smith G. Cardiovascular and catecholamine responses during endovascular and conventional abdominal aortic aneurysm repair. Eur J Vasc Endovasc Surg 1999; 17: 326–33.
Salartash K, Sternbergh WC, 3rd, York JW, Money SR. Comparison of open transabdominal AAA repair with endovascular AAA repair in reduction of postoperative stress response. Ann Vasc Surg 2001; 15: 53–9.
Aivatidi C, Vourliotakis G, Georgopoulos S, Sigala F, Bastounis E, Papalambros E. Oxidative stress during abdominal aortic aneurysm repair--biomarkers and antioxidant's protective effect: a review. Eur Rev Med Pharmacol Sci 15: 245–52.
Norgren L, Swartbol P. Biological responses to endovascular treatment of abdominal aortic aneurysms. J Endovasc Surg 1997; 4: 169-–3.
Norman JG, Fink GW. The effects of epidural anesthesia on the neuroendocrine response to major surgical stress: a randomized prospective trial. Am Surg 1997; 63: 75–80.
Peveri P, Walz A, Dewald B, Baggiolini M. A novel neutrophil-activating factor produced by human mononuclear phagocytes. J Exp Med 1988; 167: 1547–59.
Welborn MB, Oldenburg HS, Hess PJ, Huber TS, Martin TD, Rauwerda JA, et al. The relationship between visceral ischemia, proinflammatory cytokines, and organ injury in patients undergoing thoracoabdominal aortic aneurysm repair. Crit Care Med 2000; 28: 3191–7.
Hanssen SJ, Derikx JP, Vermeulen Windsant IC, Heijmans JH, Koeppel TA, Schurink GW, et al. Visceral injury and systemic inflammation in patients undergoing extracorporeal circulation during aortic surgery. Ann Surg 2008; 248: 117–25.
Boyle EM Jr, Pohlman TH, Cornejo CJ, Verrier ED. Endothelial cell injury in cardiovascular surgery: ischemia-reperfusion. Ann Thorac Surg 1996; 62: 1868–75.
Huber TS, Gaines GC. Welborn MB 3rd, Rosenberg JJ, Seeger JM, Moldawer LL. Anticytokine therapies for acute inflammation and the systemic inflammatory response syndrome: IL-10 and ischemia/reperfusion injury as a new paradigm. Shock 2000; 13: 425–34.
O'Sullivan ST, Lederer JA, Horgan AF, Chin DH, Mannick JA, Rodrick ML. Major injury leads to predominance of the T helper-2 lymphocyte phenotype and diminished interleukin-12 production associated with decreased resistance to infection. Ann Surg 1995; 222: 482–90.
Woiciechowsky C, Asadullah K, Nestler D, Eberhardt B, Platzer C, Schoning B, et al. Sympathetic activation triggers systemic interleukin-10 release in immunodepression induced by brain injury. Nat Med 1998; 4: 808–13.
Kunihara T, Kubota S, Shiiya N, Iizuka K, Sasaki S, Wakasa S, et al. Cytokine balance in hepatosplanchnic system during thoracoabdominal aortic aneurysm repair. J Artif Organs 14: 192–200.
Ziegenfuss T, Wanner GA, Grass C, Bauer I, Schuder G, Kleinschmidt S, et al. Mixed agonistic-antagonistic cytokine response in whole blood from patients undergoing abdominal aortic aneurysm repair. Intensive Care Med 1999; 25: 279–87.
Bown MJ, Nicholson ML, Bell PR, Sayers RD. Cytokines and inflammatory pathways in the pathogenesis of multiple organ failure following abdominal aortic aneurysm repair. Eur J Vasc Endovasc Surg 2001; 22: 485–95.
Norwood MG, Bown MJ, Sutton AJ, Nicholson ML, Sayers RD. Interleukin 6 production during abdominal aortic aneurysm repair arises from the gastrointestinal tract and not the legs. Br J Surg 2004; 91: 1153–6.
Febbraio MA, Ott P, Nielsen HB, Steensberg A, Keller C, Krustrup P, et al. Hepatosplanchnic clearance of interleukin-6 in humans during exercise. Am J Physiol Endocrinol Metab 2003; 285: E397–402.
Roumen RM, Hendriks T, van der Ven-Jongekrijg J, Nieuwenhuijzen GA, Sauerwein RW, van der Meer JW, et al. Cytokine patterns in patients after major vascular surgery, hemorrhagic shock, and severe blunt trauma. Relation with subsequent adult respiratory distress syndrome and multiple organ failure. Ann Surg 1993; 218: 769–76.
Komori K, Ishida M, Matsumoto T, Kume M, Ohta S, Takeuchi K, et al. Cytokine patterns and the effects of a preoperative steroid treatment in the patients with abdominal aortic aneurysms. Int Angiol 1999; 18: 193–7.
Calogero AE, Norton JA, Sheppard BC, Listwak SJ, Cromack DT, Wall R, et al. Pulsatile activation of the hypothalamic-pituitary-adrenal axis during major surgery. Metabolism 1992; 41: 839–45.
Seekamp A, Warren JS, Remick DG, Till GO, Ward PA. Requirements for tumor necrosis factor-alpha and interleukin-1 in limb ischemia/reperfusion injury and associated lung injury. Am J Pathol 1993; 143: 453–63.
Cabie A, Farkas JC, Fitting C, Laurian C, Cormier JM, Carlet J, et al. High levels of portal TNF-alpha during abdominal aortic surgery in man. Cytokine 1993; 5: 448–53.
Swartbol P, Truedsson L, Norgren L. Adverse reactions during endovascular treatment of aortic aneurysms may be triggered by interleukin 6 release from the thrombotic content. J Vasc Surg 1998; 28: 664–8.
Fiane AE, Videm V, Lingaas PS, Heggelund L, Nielsen EW, Geiran OR, et al. Mechanism of complement activation and its role in the inflammatory response after thoracoabdominal aortic aneurysm repair. Circulation 2003; 108: 849–56.
Holzheimer RG, Gross J, Schein M. Pro- and anti-inflammatory cytokine-response in abdominal aortic aneurysm repair: a clinical model of ischemia-reperfusion. Shock 1999; 11: 305–10.
Bown MJ, Horsburgh T, Nicholson ML, Bell PR, Sayers RD. Cytokines, their genetic polymorphisms, and outcome after abdominal aortic aneurysm repair. Eur J Vasc Endovasc Surg 2004; 28: 274–80.
Velazquez OC, Carpenter JP, Baum RA, Barker CF, Golden M, Criado F, et al. Perigraft air, fever, and leukocytosis after endovascular repair of abdominal aortic aneurysms. Am J Surg 1999; 178: 185–9.
Gabriel EA, Locali RF, Romano CC, Duarte AJ, Palma JH, Buffolo E. Analysis of the inflammatory response in endovascular treatment of aortic aneurysms. Eur J Cardiothorac Surg 2007; 31: 406–12.
Muckart DJ, Bhagwanjee S. American College of Chest Physicians/Society of Critical Care Medicine Consensus Conference definitions of the systemic inflammatory response syndrome and allied disorders in relation to critically injured patients. Crit Care Med 1997; 25: 1789–95.
Nano G, Occhiuto MT, Stegher S, Malacrida G, Cova M, Righini P, et al. Postimplantation syndrome after endovascular aortic repair using the Anaconda endograft. Ann Vasc Surg 2014; 28: 1409–15.
Gerasimidis T, Sfyroeras G, Trellopoulos G, Skoura L, Papazoglou K, Konstantinidis K, et al. Impact of endograft material on the inflammatory response after elective endovascular abdominal aortic aneurysm repair. Angiology 2005; 56: 743–53.
Voute MT, Bastos Goncalves FM, van de Luijtgaarden KM, Klein Nulent CG, Hoeks SE, Stolker RJ, et al. Stent graft composition plays a material role in the postimplantation syndrome. J Vasc Surg 2012; 56: 1503–9.
Berg P, Stroetges RA, Miller LE, Schoefferle J. A propensity score-matched analysis of inflammatory response with endovascular aneurysm sealing vs endovascular aneurysm repair. J Endovasc Ther 2017; 24: 670–4.
Moris DN, Kontos MI, Mantonakis EI, Athanasiou AK, Spartalis ED, Bakoyiannis CN, et al. Concept of the aortic aneurysm repair-related surgical stress: a review of the literature. Int J Clin Exp Med 2014; 7: 2402–12.
Moris D, Felekouras E, Chrousos GP. No cytokine is an island: IL-6 alone is not sufficient to predict morbidity after a major abdominal surgery. Ann Surg 2018; 267: e30–2.
Moris D, Lu L, Qian S. Mechanisms of liver-induced tolerance. Curr Opin Organ Transplant 2017; 22: 71–8.
Moris D, Karavokyros I, Spartalis E, Athanasiou A, Schizas D, Felekouras E. Early prediction of systematic inflammatory response syndrome (SIRS) after major thoracic operation should not be sneezed at, but it is not a panacea. Surgery 2017; 161: 1462–3.
Rettig TC, Verwijmeren L, Dijkstra IM, Boerma D, van de Garde EM, Noordzij PG. Postoperative interleukin-6 level and early detection of complications after elective major abdominal surgery. Ann Surg 2016; 263: 1207–12.
Longbottom ER, Torrance HD, Owen HC, Fragkou PC, Hinds CJ, Pearse RM, et al. Features of postoperative immune suppression are reversible with interferon gamma and independent of interleukin-6 pathways. Ann Surg 2016; 264: 370–7.
Moulakakis KG, Sfyroeras GS, Papapetrou A, Antonopoulos CN, Mantas G, Kakisis J, et al. Inflammatory response and renal function following endovascular repair of the descending thoracic aorta. J Endovasc Ther 2015; 22: 201–6.
Moris D, Schizas D, Liakakos T. Regarding “Prospective evaluation of postimplantation syndrome evolution on patient outcomes after endovascular aneurysm repair for abdominal aortic aneurysm”. J Vasc Surg 2016; 64: 1193–4.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Supplementary Information
Supplementary Table S1
Rights and permissions
About this article
Cite this article
Tsilimigras, D.I., Sigala, F., Karaolanis, G. et al. Cytokines as biomarkers of inflammatory response after open versus endovascular repair of abdominal aortic aneurysms: a systematic review. Acta Pharmacol Sin 39, 1164–1175 (2018). https://doi.org/10.1038/aps.2017.212
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/aps.2017.212
Keywords
This article is cited by
-
The evaluation of cytotoxicity and cytokine IL-6 production of root canal sealers with and without the incorporation of simvastatin: an invitro study
BMC Oral Health (2022)
-
LncRNA KCNQ1OT1 ameliorates the liver injury induced by acetaminophen through the regulation of miR-122-5p/CES2 axis
Molecular and Cellular Biochemistry (2020)
-
Inflammatory and oxidative stress biomarkers at protein and molecular levels in workers occupationally exposed to crystalline silica
Environmental Science and Pollution Research (2019)
-
Circulating biomarkers for cardiovascular diseases: the beats never stop
Acta Pharmacologica Sinica (2018)