Abstract
Background: Sulfonylurea compounds may impair ischemic preconditioning and endogenous fibrinolysis. Increased mortality has been reported in diabetics receiving these drugs prior to admission for acute myocardial infarction when treated by direct angioplasty. Although thrombolytics are currently employed far more frequently than direct angioplasty the effect of sulfonylureas on mortality in the setting of thrombolysis has not been previously addressed.
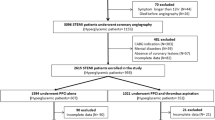
Methods: Two hundred forty five diabetics treated with either accelerated t-PA or streptokinase in a national, multi-center, randomized comparison of argatroban vs. heparin (n=1200) were grouped by anti-diabetic treatment prior to hospitalization, and their outcomes were compared by retrospective analysis.
Results: Baseline characteristics were similar in all groups (sulfonylureas: n=121, oral medications other than sulfonylureas: n=17, insulin: n=28, diet alone: n=79). Sulfonylurea use was not associated with increased mortality or adverse event rates. By logistic regression analysis with diet treatment as reference, only prior insulin use was associated with higher risk for mortality at 30 days and 1 year (odds ratios 4.5 and 5.22, respectively, p<0.05).
Conclusions: Sulfonylureas use prior to admission is not associated with adverse outcomes in diabetics treated with thrombolytics for myocardial infarction. Since direct angioplasty may increase mortality in patients taking these drugs, a randomized trial is needed to specifically compare different strategies of acute reperfusion in diabetics.
Abbreviated abstract. Increased mortality has been reported in diabetics using sulfonylureas when treated for myocardial infarction by direct angioplasty. No study has specifically addressed the effect of these drugs on outcomes in the setting of thrombolysis. In a retrospective analysis of 245 diabetics treated with thrombolysis in a randomized comparison of argatroban vs. heparin, outcomes were compared in relation to anti-diabetic therapy prior to admission. Sulfonyl-urea use did not adversely affect prognosis, which was worst among diabetics previously treated with insulin. In conclusion, sulfonylureas do not worsen outcomes of diabetics treated with current thrombolytic regimens in comparison with other anti-diabetic treatments.
Similar content being viewed by others
References
Abbud ZA, Shindler DM, Wilson AC and Kostis JB. Effect of diabetes mellitus on short–and long–term mortality rates of patients with acute myocardial infarction: A statewide study. Am Heart J 1995;130:51–58.
Mak KH, Moliterno DJ, Granger CB, et al. Influence of diabetes mellitus on clinical outcome in the thrombolytic era of acute myocardial infarction. J Am Coll Cardiol 1997;30:171–179.
Haffner SM, Lehto S, Ronnemaa T, Pyorala K, Laakso M. Mortality from coronary heart disease in subjects with type 2 diabetes and in non–diabetic subjects with and without prior myocardial infarction. N Engl J Med 1998;339:229–234.
Brady PA, Terzic A. The sulfonylurea controversy: More questions from the heart. J Am Coll Cardiol 1998;31:950–956.
Connaughton M, Webber J. Diabetes and coronary artery disease: Time to stop taking the tablets? Heart 1998;80; 108–109.
Panten U, Schwanstecher M, Schwanstecher C: Sulfonylurea receptors and mechanism of sulfonylurea action. Exp Clin Endocrinol Diabetes 1996;104:1–9.
Cleveland JC Jr, Meldrum DR, Cain BS, Banerjee A, Harken AH. Oral sulfonylurea hypoglycemic agents prevent ischemic preconditioning in human myocardium. Two paradoxes revisited. Circulation 1997;96:29–32.
Narishige T, Egashir K, Akatsuka Y, Takahashi T, Kasuya H, Takeshita A. Glibenclamide prevents coronary vasodilatation induced by beta 1–adrenoreceptor stimulation in dogs. Am J Physiol 1994; 266:H84–H92.
Mansfield MW, Stickland MH, Grant PJ. Environmental and genetic factors in relation to elevated circulating levels of plasminogen activator–1 in caucasian patients with non–insulin–dependent diabetes mellitus. Thromb Haemost 1995;74:842–847.
Ito Y, Okeda T, Sato Y, Ito M, Sakata T. Plasminogen activator inhibitor–1 in non–obese subjects with non–insulin–dependent diabetes mellitus. Proc Soc Exp Biol Med 1996;211:287–291.
Panahloo A, Mohamed–Ali V, Andres C, Denver AE, Yudkin JS. Effect of insulin versus sulfonylurea therapy on cardiovascular risk factors and fibrinolysis in type II diabetes. Metabolism 1998;47: 637–643.
Gram J, Jespersen J. Increased fibrinolytic potential induced by gliclazide in type I and type II diabetic patients. Metabolism 1992;41(Suppl 1):25–29.
Ziegler O, Drouin P. Hemobiological properties of gliclazide. J Diabetes Complications 1994;8:235–239.
Mak KH, Topol EJ. Emerging concepts in the management of acute myocardial infarction in patients with diabetes mellitus. J Am Coll Cardiol 2000;35:563–568.
Garrat KN, Brady PA, Hassinger NL, Grill DE, Terzic A, Holmes DR Jr. Sulfonylurea drugs increase early mortality in patients with diabetes mellitus after direct angioplasty for acute myocardial infarction. J Am Coll Cardiol 1999;33:119–124.
Brady PA, Al–Suwaidi J, Kopecky SL, Terzic A. Sulfonylurea and mortality in diabetic patients after myocardial infarction. Circulation 1998;97:709–710. [letter].
Davis TME, Parsons RW, Broadhurst RJ, Hobbs MST, Jamrozik K. Arrhythmias and mortality after myocardial infarction in diabetic subjects. Relation to diabetes treatment. Diabetes Care 1998;21:637–640.
Klamann A, Sarfert P, Launhardt V, Schulte G, Schmiegel WH, Nauck MA. Myocardial infarction diabetic vs. non–diabetic subjects. Survival and infarct size following therapy with sulfonylureas (glibenclamide). Eur Heart J 2000;21:220–229.
Behar S, Hod H, Kaplinsky E, for the ARGAMI–2 Study Group. Argatroban vs. heparin as adjuvant therapy to thrombolysis for acute myocardial infarction. Circulation 1998;98(Suppl I):I–453–I–454. [abstr].
Fliess JL. Statistical Methods for Rates and Proportions, 2nd ed. New York: John Wiley and Sons, 1981:260–265.
Meinert CL, Knatterund GL, Prout TE, Klimt CR. A study of the effects of hypoglycemic agents on vascular complications of patients with adult–onset diabetes. Diabetes 1970;19:789–830.
Genuth S. Exogenous insulin administration and cardiovascular risk in non–insulin–dependent and insulin–dependent diabetes mellitus. Ann Intern Med 1996;124:104–109.
UK Prospective Diabetes Study (UKPDS) Group. Intensive blood–glucose control with sulphonylureas or insulin compared with conventional treatment and risk of complications in patients with 2 diabetes (UKPDS 33). Lancet 1998;352:837–853.
UK Prospective Diabetes Study (UKPDS) Group. Effect of intensive blood–glucose control with metformin on complications in overweight patients with type 2 diabetes (UKPDS 34). Lancet 1998;352:854–865.
Malmberg K, Norhammar A, Wedel H, Ryden L. Glycometabolic state at admission: important risk marker of mortality in conventionally treated patients with diabetes mellitus and acute myocardial infarction. Circulation 1999;99:2626–2632.
O'Keefe JH, Blackstone EH, Sergeant P, McCallister BD. The optimal mode of coronary revascularization for diabetics. A risk–adjusted long–term study comparing coronary angioplasty and coronary bypass surgery. Eur Heart J 1998;19:1696–1703.
Tomai F, Crea F, Gaspardone A, Versaci F, De Paulis R. Ischemic preconditioning during coronary angioplasty is prevented by glibenclamide, a selective ATPsensitive K+ channel blocker. Circulation 1994;90:700–705.
Weintraub WS, Stein B, Kosinski A, et al. Outcome of coronary bypass surgery versus coronary angioplasty in diabetic patients with multivessel coronary artery disease. J Am Coll Cardiol 1998;31:10–19.
Malmberg K, for the DIGAMI investigators. Prospective randomized study of intensive insulin treatment on long–term survival after acute myocardial infarction in patients with diabetes mellitus. BMJ 1997;314:1512–1515.
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Halkin MD, A., Roth MD, A., Jonas MD, M. et al. Sulfonylureas Are Not Associated With Increased Mortality in Diabetics Treated With Thrombolysis for Acute Myocardial Infarction. J Thromb Thrombolysis 12, 177–184 (2001). https://doi.org/10.1023/A:1012979622945
Issue Date:
DOI: https://doi.org/10.1023/A:1012979622945