Abstract
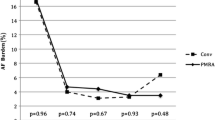
Defibrillation energy requirements of epicardial implantable cardioverter defibrillator systems are generally lower than endovascular systems currently used. The former has the disadvantage of requiring a thoracotomy and so has a greater morbidity and mortality than an endovascular procedure. The middle cardiac vein (MCV) is an epicardial structure that is accessible by a non-thoracotomy approach. This study investigated the merits of ventricular defibrillation from the middle cardiac vein. Methods and Results. Defibrillation thresholds (DFT) were measured in 10 anesthetized pigs, weighing 34.5–44.1 kg (mean 39 kg). An Angeflex electrode (1.7mm × 50mm) was introduced via the left external jugular vein to the right ventricular apex. The MCV was identified with standard angiography techniques and a 4080 (Angeion Corp.) defibrillation electrode (1.6mm × 65mm) introduced into the vein. An active can was implanted in the left subpectoral region. The defibrillation thresholds (DFT) of the following defibrillation configurations were assessed using a modified four-reversal binary search: RV → Can, RV+MCV → Can and MCV → Can. The DFT's for the three configurations were 15.5±2.8 J, 10.8±3.4 J and 13.7±2.4 J. Analysis of variance showed that the DFT with the RV+MCV combination was significantly less than the RV alone (p < 0.05) Conclusions: Defibrillation is possible through the MCV and that incorporating an electrode in the MCV with RV-Can configuration can reduce the DFT by 30%.
Similar content being viewed by others
References
Saksena S, Musif A, Prakash A, Madan N. Future directions for implantable defibrillation devices. In: Interventional Electrophysiology. 1996;617–649.
Mouchawar GA, Wolsleger WK, Doan PD, Causey JD, Kroll MW. Does an SVC electrode further reduce DFT in a hotcan ICD system? Pacing Clin Electrophysiol 1997;20:163–167.
Bardy GH, Dolack GL, Kudenchuk PJ, Poole JE, Mehra R. Johnson G. Prospective, randomized comparison in humans of a unipolar defibrillation system with that using an additional superior vena cava electrode. Circulation 1994;89:1090–1093.
Bardy GH, Allen MD, Mehra R, Johnson G. An effective and adaptable transvenous defibrillation system using the coronary sinus in humans. J Am Coll Cardiol 1990;16:887–895.
Bardy GH, Allen MD, Mehra R, Johnson G, Feldman S, Greene HL, Ivey TD. Transvenous defibrillation in humans via the coronary sinus. Circulation 1990;81:1252–1259.
Kudenchuk PJ, Bardy GH, Dolack GL, Poole JE, Mehra R, Johnson G. Efficacy of a single-lead unipolar transvenous defibrillator compared with a system employing an additional coronary sinus electrode. A prospective, randomized study. Circulation 1994;89:2641–2644.
Guse PA, Walcott GP, Rollins DL, Smith WM, Ideker RE. Defibrillation electrode configurations developed from cardiac mapping that combine biphasic shocks with sequential timing. Am Heart J 1992;124:1491–1500.
Singer I, Goldsmith J, Maldonado C. Transseptal defibrillation is superior for transvenous defibrillation. Pacing Clin Electrophysiol 1995;18:229–232.
Mower MM, Mirowski M, Spear JF, Moore EN. Patterns of ventricular activity during catheter defibrillation. Circulation 1974;49:858–861.
Kallok MJ. Pathways for Defibrillation Current. In: Kroll MW, Lehmann MH, eds. Implantable Cardioverter Defibrillator Therapy: The Engineering-Clinical Interface. The Netherlands: Kluwer Academic Publishers, 1993;105–119.
Martin DR, Newman D, Sheahan R, Yao J, Dorian P. Inadvertent defibrillator sense/pace lead placement in the middle cardiac vein: a possible complication with new implications. Pacing Clin Electrophysiol 1994;17:2349–2352.
Arruda M, Otomo K, Reynolds D, Bonner M, Pitha J, Bussey J, Nakagawa H, Imai S, Lazzara R. Ventricular defibrillation from the middle cardiac vein: A new transvenous epicardial lead configuration to lower the defibrillation threshold. (Abstract) Pacing Clin Electrophysiol 1998;21:853.
Zipes DP, Fischer J, King RM, Nicoll Ad, Jolly WW. Termination of ventricular fibrillation in dogs by depolarizing a critical amount of myocardium. Am J Cardiol 1975;36:37–44.
Chang MS, Inoue H, Kallok MJ, Zipes DP. Double and triple sequential shocks reduce ventricular defibrillation threshold in dogs with and without myocardial infarction. J Am Coll Cardiol 1986;8:1393–1405.
Gras D, Mabo P, Ritter P, Cazeau S, Mainardis M, Debroucker F, Daubert J. First experience with coronary sinus leads used for permanent left ventricular pacing. (Abstract) Pacing Clin Electrophysiol 1998;21:825.
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Roberts, P.R., Urban, J.F., Euler, D.E. et al. The Middle Cardiac Vein—A Novel Pathway to Reduce the Defibrillation Threshold. J Interv Card Electrophysiol 3, 55–60 (1999). https://doi.org/10.1023/A:1009827607495
Issue Date:
DOI: https://doi.org/10.1023/A:1009827607495