Abstract
Purpose. Distribution to the effect site is a prerequisite for the therapeutic effect and determined by physicochemical properties and affinities to inside- and outside-directed transporters. Based on the hypothesis that lipophilic esters of the GABA-derivative baclofen have a higher affinity to brain tissue, baclofen esters (methyl, ethyl, 1-propyl, 2-propyl, butyl) were studied regarding their penetration through the blood-brain barrier and their affinities to P-glycoprotein (P-gp).
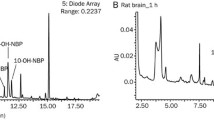
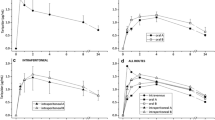
Methods. Octanol-water distribution coefficients (D) served as lipophilicity parameters. Blood and brain concentrations of baclofen and its methyl ester were determined in vivo in rats following intraperitoneal administration. Affinities to P-gp were evaluated using a radioligand binding assay based on P-gp-overexpressing cells and [3H]-talinolol as radioligand.
Results. Log D values for baclofen and ester derivatives were -0.96 (baclofen), 0.48 (methyl), 0.77 (ethyl), 1.31 (1-propyl), 1.27 (2-propyl), and 1.42 (butyl). In-vitro studies yielded negligible affinity of baclofen to P-gp, whereas IC50-values for the esters ranged between 1300 μM (methyl) and 290 μM (2-propyl). Affinity parameters correlated well with the lipophilicity parameters.
Conclusions. Despite the P-gp affinity, brain concentrations of methyl ester were significantly higher than those of baclofen, however, baclofen levels following administration of the ester were smaller than with baclofen administration indicating only partial hydrolysis.
Similar content being viewed by others
REFERENCES
H. Müller, J. Zierski, D. Dralle, D. Krauß, and E. Mutschler. Pharmacokinetics of intrathecal baclofen. In: H. Müller, J. Zierski, and R. D. Penn (eds.) Local-Spinal Therapy of Spasticity, Springer Verlag Berlin, Heidelberg, New York, 1988 pp. 223-226.
Y. Kido, I. Tamai, H. Uchino, F. Suzuki, Y. Sai, and A. Tsuji. Molecular and functional identification of large neutral amino acid transporters LAT1 and LAT2 and their pharmacological relevance at the blood-brain barrier. J. Pharm. Pharmacol. 53:497-503 (2001).
H. Matsuo, S. Tsukada, T. Nakata, A. Chairoungdua, D. K. Kim, S. H. Cha, J. Inatomi, H. Yorifuji, J. Fukuda, H. Endou, and Y. Kanai. Expression of a system L neutral amino acid transporter at the blood-brain barrier. NeuroReport 11:3507-3511 (2000).
I. Tamai and A. Tsuji. Transporter-mediated permeation of drugs across the blood-brain barrier. J. Pharm. Sci. 89:1371-1388 (2000).
I. A. Simpson, N. M. Appel, M. Hokari, J. Oki, G. D. Holman, F. Maher, E. M. Koehler-Stec, S. J. Vannucci, and Q. R. Smith. Blood-brain barrier glucose transporter: effects of hypo-and hyperglycemia revisited. J. Neurochem. 72:238-247 (1999).
P. Jolliet-Riant and J. P. Tillement. Drug transfer across the blood-brain barrier and improvement of brain delivery. Fundament. Clin. Pharmacol. 13:16-26 (1999).
R. J. Boado, J. Y. Li, M. Nagaya, C. Zhang, and W. M. Pardridge. Selective expression of the large neutral amino acid transporter at the blood-brain barrier. Proc. Natl. Acad. Sci. USA 96:12079-12084 (1999).
E. M. Cornford, S. Hyman, and B. E. Swartz. The human brain GLUT1 transporter: ultrastructural localization of the blood-brain barrier endothelia. J. Cereb. Blood Flow Metab. 14:106-112 (1994).
M. F. Fromm. P-glycoprotein: a defense mechanism limiting oral bioavailability and CNS accumulation of drugs. Int. J. Clin. Pharmacol. Ther. 38:69-74 (2000).
J. Bart, H. J. Groen, N. H. Hendrikse, W. T. van der Graaf, W. Vaalburg, and E. G. de Vries. The blood-brain barrier and oncology: new insights into function and modulation. Cancer Treat. Rev. 26:449-462 (2000).
P. L. Golden and W. M. Pardridge. Brain microvascular P-glycoprotein and a revised model of multidrug resistance in brain. Cell. Mol. Neurobiol. 20:165-181 (2000).
M. Sugawara, W. Huang, Y. J. Fei, F. H. Leibach, V. Ganapathy, and M. E. Ganapathy. Transport of valganciclovir, a ganciclovir prodrug, via peptide transporters PEPT1 and PEPT2. J. Pharm. Sci. 89:781-789 (2000).
R. Niemi, P. Turhanen, J. Vepsalainen, H. Taipale, and T. Jarvinen. Bisphosphonate prodrugs: synthesis and in vitro evaluation of alkyl and acylmethoxy esters of etidronic acid as bioreversible prodrugs of etidronate. Eur. J. Pharm. Sci. 11:173-180 (2000).
L. Mizen and G. Burton. The use of esters as prodrugs for oral delivery of beta-lactam antibiotics. Pharm. Biotech. 11:11345-11365 (1998).
Y. Deguchi, H. Hayashi, S. Fujii, T. Naito, Y. Yokoyama, S. Yamada, and R. Kimura. Improved brain delivery of a nonsteroidal anti-inflammatory drug with a synthetic glyceride ester: a preliminary attempt at a CNS drug delivery system for the therapy of Alzheimer's disease. J. Drug Target. 8:371-381 (2000).
B. Herber. Brain distribution of drugs-Correlation with lipophilicity and dependence on the administration route. PhD thesis, Martin-Luther-University Halle-Wittenberg, Halle/S., Department of Pharmacy (2002)
S. Döppenschmitt, H. Spahn-Langguth, C. G. Regardh, and P. Langguth. The role of P-glycoprotein mediated secretion in absorptive drug fluxes. J. Pharm. Sci. 88:1067-1072 (1999).
R. C. Baselt, D. Yoshikawa, and J. Chang. and J. Li. Improved long-term stability of blood cocaine in evacuated collection tubes. J. Forensic Sci. 38:935-937 (1993).
L. Sachs. Applied Statistics. Springer-Verlag, Berlin, Heidelberg, New York, 1978.
M. J. Moll-Navarro, M. Merino, V. G. Casabo, A. Nacher, and A. Polache. Interaction of taurine on baclofen intestinal absorption: a nonlinear mathematical treatment using differential equations to describe kinetic inhibition models. J. Pharm. Sci. 85:1248-1254 (1996).
J. B. M. M. van Bree, C. D. Heijligers-Feijen, A. G. de Boer, M. Danhof, and D. D. Breimer. Stereoselective transport of baclofen across the blood-brain barrier in rats as determined by the unit impulse response methodology. Pharm. Res. 8:259-262 (1991).
Y. Deguchi, K. Inabe, K. Tomiyasu, K. Nozawa, S. Yamada, and R. Kimura. Study on brain interstitial fluid distribution and blood-brain barrier transport of baclofen in rats by microdialysis. Pharm. Res. 12:1838-1844 (1995).
A. Koggel. Influence of secretory transporters on the intestinal permeability of cationic drugs. PhD. thesis, Johannes Gutenberg-University Mainz, Department of Pharmacy (2002).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Leisen, C., Langguth, P., Herbert, B. et al. Lipophilicities of Baclofen Ester Prodrugs Correlate with Affinities to the ATP-Dependent Efflux Pump P-Glycoprotein: Relevance for Their Permeation Across the Blood-Brain Barrier?. Pharm Res 20, 772–778 (2003). https://doi.org/10.1023/A:1023437603555
Issue Date:
DOI: https://doi.org/10.1023/A:1023437603555