Abstract
Context: Unfractionated heparin remains widely utilized in the treatment of acute coronary syndromes (ACS). However, limited data exist on optimal dosing and range of activated partial thromboplastin time (aPTT) in this setting. A large trial of thrombolysis for acute myocardial infarction has reported an association between longer aPTTs and adverse outcomes.
Objectives: Estimate the optimal heparin-dosing regimen in achieving early therapeutic aPTTs (50 to 75 seconds) and determine the association of aPTT and death, reinfarction, and bleeding in population with ACS.
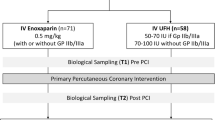
Design: Subgroup analysis within a randomized, controlled trial of 5861 patients given unfractionated heparin who had aPTTs at 6, 12, or 24 hours, with outcome analyses by weight categories.
Setting: In 373 hospitals in 13 countries from May 1994 to October 1995.
Patients: A total of 12,142 patients admitted for ACS, stratified by the presence (n = 4131) or absence (n = 8011) of ST-segment elevation, and randomized to 72 hours of unfractionated heparin.
Results: In a simulated weight-adjusted model, based on retrospective grouping by weight, a simulated dose of 60-U/kg bolus and 12-U/kg/h infusion resulted in the highest proportion of therapeutic aPTTs. After adjustment for baseline variables, longer 12-hour aPTT was associated with the composite of 30-day death or reinfarction in patients not treated with thrombolytic therapy (odds ratio, 1.10; 95% CI, 1.00 to 1.22; P = 0.047). Longer aPTT at 6 hours was associated with increased moderate or severe bleeding for the entire cohort. There was also a significant, nonlinear correlation of the 12-hour aPTT with moderate or severe bleeding in thrombolysis-treated patients.
Conclusions: For ACS patients who are treated with heparin, aPTT is highly associated with body weight. Longer aPTT within the first 12 hours is associated with adverse outcomes in ACS. Heparin dosing for ACS should be weight based.
Similar content being viewed by others
References
Ambrose JA, Winters SL, Arora RR, et al. Angiographic evaluation of coronary artery morphology in unstable angina. J Am Coll Cardiol 1986;7:474–478.
Williams AE, Freeman MR, Chisolm RJ, Patt NL, Armstrong PW. Angiographic morphology in unstable angina pectoris. Am J Cardio 1988;62:1024–1027.
Falk E, Shah PK, Fuster V. Coronary plaque disruption. Circulation 1995;92:657–671.
Fuster V, Badimon L, Badimon JJ, Chesebro JH. The pathogenesis of coronary artery disease and the acute coronary syndromes [2]. N Engl J Med 1992;36:310–318.
Libby P. Currents concepts of the pathogenesis of the acute coronary syndromes. Circulation 2001;104:365–372.
Vetrovec G, Leinback R, Gold HK, Cowley MJ. Intracoronary thrombolysis in syndromes of unstable angina: Angiographic and clinical results. Am Heart J 1982;104:946–952.
Mandelkorn J, Wolf N, Singh S, et al. Intracoronary thrombs in nontransmural myocardial infarction and in unstable angina pectoris. Am J Cardiol 1983;52:1–6.
Sherman CT, Litvack F, Gundfest T, et al. Coronary angioscopy in patients with unstable angina pectoris. N Eng J Med 1986;315:913–919.
Mizuno K, Satomora K, Miyamoto A, et al. Angioscopic evaluation of coronar artery thrombi in acute coronary syndromes. N Engl J Med 1992;326:287–291.
Ryan TJ, Antman EM, Brooks NH, et al. ACC/AHA guide-lines for the management of patients with acute my-ocardial infarction. A report of the ACC/AHA taskforce on practice guidelines. J Am Coll Cardiol 1999;34:890–911.
Braunwald E, Mark DB, Jones RH, et al. Unstable angina: Diagnosis and management. Clinical Practice Guideline No. 10. Rockville, MD: Agency for Health Care Policy and Research, 1994. (AHCPR Publication No. 94-0602).
Theroux P, Ouimet H, McCans J, et al. Aspirin, heparin or both to treat unstable angina. N Eng J Med 1988;319:1105–1111.
Theroux P, Waters D, Qui S, McCans J, deGuise P, Juneau M. Aspirin versus heparin to prevent myocardial infarction during the acute phase of unstable angina. Circulation 1993;88:2045–2048.
The RISC Group. Risk of myocardial infarction and death during treatment with low dose aspirin and intravenous heparin in men with unstable coronary artery disease. Lancet 1990;336:827–830.
Cohen M, Adams PC, Parry G, et al. Combination antithrombotic therapy in unstable rest angina and non-Q-wave infarction in non-prior aspirin users: Primary end points analysis from the ATACS trial. Circulation 1994;89:81–88.
Fragmin during Instability in Coronary Artery Disease (FRISC) Study Group. Low-molecular-weight heparin during instability in coronary artery disease. Lancet 1996;347:561–568.
Oler A, Whooley MA, Oler J, Grady D. Adding heparin to aspirin reduces the incidence of myocardial infarction and death in patients with unstable angina: A meta-analysis. JAMA 1996;276:811–815.
Menon V, Berkowitz SD, Antman EM, Fuchs RM, Hochman JS. New heparin dosing recommendations for patients with acute coronary syndromes. Am J Med 2001;110:641–650.
Giugliano RP, McCabe CH, Antman EM, et al. Lower-dose heparin with fibrinolysis is associated with lower rates of intracranial hemorrhage. Am Heart J 2001;141:742–750.
Braunwald E, Antman EM, Beasley JW, et al. ACC/AHA guidelines for the management of patients with unstable angina, and non-ST-segment activation myocardial infarction. A report of the ACC/AHA taskforce on practice guidelines (Committee of the management of patients with unstable angina). J Am Coll Cardiol 2000;36:970–1062.
Granger CB, Hirsch J, Califf RM, et al., for the GUSTO-I Trial Investigators. Activated partial thromboplastin time and outcome after thrombolytic therapy for acute myocardial infarction: The results from the GUSTO-I trial. Circulation 1996;93:870–878.
White HD, Barbash GI, Califf RM, et al. Age and outcome with contemporary thrombolytic therapy: Results from the GUSTO-I trial. Circulation 1996;94:1826–1833.
Cipolle R, Seifert R, Neilan B, Zaske DE, Haus E. Heparin kinetics: Variables related to disposition and dosage. Clin Pharmacol Ther 1981;29:387–393.
The GUSTO-IIb Investigators. A comparison of recombinant hirudin with heparin for the treatment of acute coronary syndromes. N Engl J Med 1996;335:775–782.
Gilchrist IC, Berkowitz SD, Thompson TD, Califf RM, Granger CB. Heparin dosing and outcome in acute coronary syndromes: The GUSTO-IIb experience. Am Heart J 2002;144:73–80.
The GUSTO-IIa Investigators. Randomized trial of intravenous heparin versus recombinant hirudin for acute coronary syndromes. Circulation 1994;90:1631–1637.
Arnout J, Simoons M, deBono D, Rapold HJ, Collen D, Verstraete M. Correlation between level of heparinization and patency of the infarct relate artery treatment of acute myocardial infarction with alteplase (rTPA). J Am Coll Cardiol 1992;20:513–519.
Bozovich GE, Gurfinkel EP, Antman EM, McCabe CH, Mautner B. Superiority of Enoxaparin versus unfractionated heparin for unstable angina/non-Q-wave myocardial infarction regardless of activated partial thromboplastin time. Am Heart J 2000;140:637–642.
Antman EM, McCabe CH, Gurfinkel EP, et al. Enoxaparin prevents death and cardiac ischemic events in unstable angina/non-Q wave myocardial infarction: Results of the Thrombolysis in Myocardial Infarction (TIMI) 11B trial. Circulation 1999;100:1593–1601.
Hsia J, Kleiman NS, Aguirre FV, Chaitman BR, Roberts R, Ross AM. Heparin induced prolongation of partial thromboplastin time after thrombolysis: Relation to coronary artery patency. J Am Coll Cardiol 1992;20:31–35.
De Cristofaro R, De Candia E, Landolfi R. Effect of high-and low-molecular-weight heparins on thrombin-thrombomodulin interaction and protein C activation. Circulation 1998;98:1297–1301.
Warkentin TE. Heparin-induced thrombocytopenia: IgG-mediated platelet activation, platelet microparticle generation, and altered procoagulant/anticoagulant balance in the pathogenesis of thrombosis and venous limb gangrene complicating heparin-induced thrombocytopenia. Transfus Med Rev 1996 1996;10:249–258.
Chiu HM, Hirsch J, Yung WL, Regoeczi E, Gent M. Relationship between the anticoagulant and antithrombotic effects of heparin in experimental venous thrombosis. Blood 1977;49:172–184.
Theroux P, Waters D, Lam J, Juneau M, McCans J. Reactivation of unstable angina after the discontinuation of heparin. N Engl J Med 1992;327:141–145.
Gori AM, Pepe G, Attanasio M, et al. Tissue factor reduction and tissue factor pathway inhibitor release after heparin administration. Thromb Haemost 1999;81:589–593.
Lauer MA, Houghtaling PL, Peterson JG, et al. Attenuation of rebound ischemia after discontinuation of heparin therapy by glycoprotein IIb/IIIa inhibition with eptifibatide in patients with acute coronary syndromes: Observations from the platelet IIb/IIIa in unstable angina: Receptor suppression using integrilin therapy (PURSUIT) trial. Circulation 2001;104:2772–2777.
The GUSTO-IIa Investigators. Randomized trial of intravenous heparin versus recombinant hirudin for acute coronary syndromes. Circulation 1994;90:1631–1637.
Antman EM, Hirudin in acute myocardial infarction: Safety report from the Thrombolysis and Thrombin Inhibition in Myocardial Infarction (TIMI) 9A Trial. Circulation 1994;90:1624–1630.
In TIME-II Investigators. Intravenous nPA for the treatment of infracting myocardium early: In TIME-II, a double-blind comparison of single bolus lanoteplase vs. accelerated alteplase vs. for the treatment of patients with acute myocardial infarction. Eur Heart J 2000;21:2005–2013.
Single-bolus tenecteplase compared with front-loaded alteplase in acute myocardial infarction: The ASSENT-2 double-blind randomized trial: Assess of the Safety and Efficacy of a New Thrombolytic Investigators. Lancet 1999;354:716–722.
Assessment of the Safety and Efficacy of a New Thrombolytic Regimen (ASSENT)-3 Investigators. Efficacy and safety of tenecteplase in combination with enoxaparin, abciximab, or unfractionated heparin: The ASSENT-3 randomised trial in acute myocardial infarction. Lancet 2001;358:605–613.
Hirsch J, Warkentin TE, Shaughnessy SG, et al. Heparin and low-molecular-weight heparin: Mechanisms of action, pharmacokinetics, dosing, monitoring, efficacy, and safety. Sixth ACCP consensus conference on antithrombotic therapy. Chest 2001;119:64–93S.
White RH, Zhou H, Woo L, Mungall D. Effect of weight, sex, age, clinical diagnosis and thromboplastin reagent on steady state intravenous heparin requirements. Arch Intern Med 1997;157:2468–2472.
Hochman JS, Wali AU, Gavrila D, et al. A new regimen for heparin use in acute coronary syndromes. Am Heart J 1999;138:313–318.
Hassan WM, Flaker GC, Feutz C, Petroski GF, Smith D. Improved anticoagulation with a weight adjusted heparin nomogram in patients with acute coronary syndromes: A randomized trial. J Tromb Thrombol 1995;2:245–249.
Cohen M, Demers C, Gurfinkel EP, et al., for the ESSENCE study group. A comparison of low-molecular-weight heparin with unfractionated heparin for unstable coronary artery diseases. N Engl J Med 1997;337:447–452.
Hirsh J, Van Aken G, Gallus AS, et al. Heparin kinetics in venous thrombosis and pulmonary embolism. Circulation 1976;53:691–695.
Davi G, Gennaro F, Spatola A, et al. Thrombin-antithrombin III complexes in type II diabetes mellitus. J Diabetes Complic 1992;6:7–11.
Tschoepe D, Schauseil S, Rosen P, Kaufman L, Gries FA. Increased platelet volume: Sign of impaired thrombopoiesis in diabetes mellitus. Klin Wochenscht 1989;67: 253–259.
Silva JA, Escobar A, Collins TJ, Ramee SR, White CJ. Unstable angina: A comparison of angioscopic findings between diabetic and non diabetic patients. Circulation 1995; 92:1731–1736.
Becker RC, Cannon CP, Tracy RP, et al. Relation between systemic anticoagulation as determined by activated partial thromboplastin time and heparin measurements and in-hospital clinical events in unstable angina and non-Q wave myocardial infarction. Thrombolysis in Myocardial Ischemia III B Investigators. Am Heart J 1996;131:421–433.
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Lee, M.S., Wali, A.U., Menon, V. et al. The Determinants of Activated Partial Thromboplastin Time, Relation of Activated Partial Thromboplastin Time to Clinical Outcomes, and Optimal Dosing Regimens for Heparin Treated Patients with Acute Coronary Syndromes: A Review of GUSTO-IIb. J Thromb Thrombolysis 14, 91–101 (2002). https://doi.org/10.1023/A:1023235926825
Issue Date:
DOI: https://doi.org/10.1023/A:1023235926825