Abstract
Background: The upper limit of vulnerability (ULV) is the stimulus strength above which ventricular fibrillation cannot be induced, even when the stimulus occurs during the vulnerable period of the cardiac cycle. Determination of ULV using T-wave shocks during ventricular pacing has been shown to closely correlate with the defibrillation threshold (DFT) at ICD implantation. However, there are no data correlating ULV determined in sinus rhythm at ICD implantation, with DFT determined at implantation or during long-term follow-up. This is of clinical importance since ULV may be used to estimate DFT during ICD implantation, both during ventricular pacing or sinus rhythm.
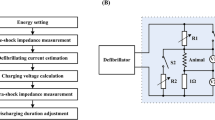
Methods and Results: Twenty-one patients receiving a transvenous ICD system were studied prospectively. There were 16 males and 5 females, mean age 68 ± 15 years, with mean ejection fraction 37.4 ± 17.4%. All had structural heart disease. The ULV was defined as the lowest energy that did not induce ventricular fibrillation with shocks at 0, 20 and 40ms before the peak of the T-wave, using a step-down protocol. The initial energy tested was 15J and the lowest energy 2J. DFT was determined following a similar step-down protocol. The DFT was defined as the lowest energy that successfully defibrillated the ventricles. The linear correlation coefficient between ULV and DFT was r = 0.73 (p < 0.001). At implant, mean ULV was 9.2 ± 5J, not statistically different from mean DFT 9.4 ± 4J. ULV plus 5J successfully defibrillated 19 of 21 patients. During long-term follow-up of 10.1 ± 1.8 months in eight patients, DFT was 8.8 ± 5.8J, not significantly different than the DFT of 7.5 ± 4.1J or ULV of 8.0 ± 5.3 at implant.
Conclusion: 1) When determined during normal sinus rhythm the ULV significantly correlates with DFT. 2) ULV testing might be used in lieu of standard DFT testing to confirm adequate lead placement thus minimizing or eliminating VF inductions, particularly in hemodynamically unstable patients. 3) Since ULV + 5J has a high probability of successful defibrillation in most patients, programming ICD first shock energy for VF at ULV + 5J may result in lower first shock energies compared to the standard methods of programming first shock energy at twice DFT.
Condensed Abstract. The purpose of this study was to determine if the upper limit of vulnerability (ULV) determined during normal sinus rhythm correlates with the defibrillation threshold (DFT), as has been previously shown when determined during ventricular pacing. The linear correlation coefficient between the ULV and DFT was r = 0.73 (p < 0.001). Mean ULV at implant was 9.2 ± 5J, not statistically different from mean DFT of 0.4 ± 4J. During long-term follow-up of 10.1 ± 1.8 months in 8 patients, DFT was 8.75 ± 8J, not significantly different than the DFT of 7.5 ± 4.1J or ULV of 8.0 ± 5.3 at implant. Shocks energies of ULV + 5J successfully defibrillated 19 of 21 patients at implant and 8 of 8 at follow-up. This study indicates that the ULV determined in normal sinus rhythm closely correlates with the DFT, and that ULV + 5J defibrillated most patients. ULV testing could be used to predict DFT and reduce or eliminate the need for DFT testing and VF induction. Programming ICD first shock energy for VF to ULV + 5J will result in lower energy than that used with standard DFT testing.
Similar content being viewed by others
References
Block M, Hammel D, Isbruch F, et al. Results and realistic expectations with transvenous lead systems. PACE Pacing Clin Electrophysiol 1992;15:665–670.
Bardy GH, Hofer B, Johnson G, et al. Implantable transvenous cardioverter-defibrillators. Circulation 1993;87: 1152–1168.
Frame R, Brodman R, Furman S, et al. Clinical evaluation of the safety of repetitive intraoperative defibrillation threshold testing. PACE Pacing Clin Electrophysiol 1992; 15:870–877.
Chen P-S, Shibata N, Dixon EG, et al. Comparison of the defibrillation threshold and the upper limit of ventricular vulnerability. Circulation 1986;73:1022–1028.
Chen P-S, Feld G, Kriett JM, et al. Relation between upper limit of vulnerability and defibrillation threshold in humans. Circulation 1993;88:186–192.
Hwang C, Swerdlow C, Kass R, et al. Upper limit of vulnerability reliably predicts the defibrillation threshold in humans. Circulation 1994;90:2308–2314.
Fabiato PA, Coumel P, Gourgon R, et al. Le seuil de response synchrone des fibres myocardiques: Application a la comparison experimentale de l' efficacite des differentes formes de chocs electriques de defibrillation. Arch Mal Coeur Vaiss 1967;60:527–544.
Lesigne C, Levy B, Saumont R, et al. An energy-time analysis of ventricular fibrillation and defibrillation thresholds with internal electrodes. Med Biol End 1976;14:617–622.
Han J, Millet D, Chizzonitti B, Moe GK. Temporal dispersion of recovery of excitability in atrium and ventricle as a function of heart rate. Am Heart J 1966;71:481–487.
Han J, Garcia de Jalon P, Moe GK. Fibrillation threshold of premature ventricular responses. Circ Res 1996;18:18–25.
Chen P-S, Feld G, Mower MM, et al. The effects of pacing rate and timing of shock on the relationship between the defibrillation threshold and the upper limit of vulnerability in open chest dogs. J Am Coll Cardiol 1991;18:1555–1563.
Hou C, Chang Sing P, Flynn E, et al. Determination of ventricular vulnerable period and ventricular fibrillation threshold by use of T-wave shocks in patients undergoing implantation of cardioverter/defibrillators. Circulation 1995;92:2558–2564.
Hsia H, Chonielewski L, Coss'u S, et al. A practical application of upper limit of vulnerability for predicting defibrillation threshold in man. PACE 1996;19:656 (abstract).
Birgersdotter-Green U, Mollerus M, Fujimura O, Feld GK. Defibrillation efficacy with ICD first shock energy programmed at ULV plus five joules using the Endo Tak Transvenous lead system: Comparison of results at implant and during long-term followup. Pacing Clin Electrophysiol 1997;20:1223 (abstract).
SPSS for Windows, Version 6.12, IL.
King BG. The Effect of Electric Shock on Heart Action with Special Reference to Varying Susceptibility in Different Parts of the Cardiac Cycle. New York: Aberdeen Press, Columbia university; 1934. Thesis.
Wiggers CJ, Wegric R. Ventricular fibrillation due to single localized induction and condenser shocks applied during the vulnerable phase of ventricular systole. Am J Physiol 1990; 128:500–505.
Shumway NE, Stish RJ. The study of ventricular fibrillation by threshold determinations. J Thorac Surg 1957;34: 643–653.
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Birgersdotter-Green, U., Undesser, K., Fujimura, O. et al. Correlation of Acute and Chronic Defibrillation Threshold with Upper Limit of Vulnerability Determined in Normal Sinus Rhythm. J Interv Card Electrophysiol 3, 155–161 (1999). https://doi.org/10.1023/A:1009825731592
Issue Date:
DOI: https://doi.org/10.1023/A:1009825731592