Abstract
Purpose. The ability to optimize new formulations for pulmonary delivery has been limited by inadequate in vitro models used to mimic conditions particles encounter in the lungs. The aim is to develop a physiologically-relevant model of the pulmonary epithelial barrier that would allow for quantitative characterization of therapeutic aerosols in vitro.
Methods. Calu-3 human bronchial epithelial cells were cultured on permeable filter inserts under air-interfaced culture (AIC) and liquid-covered culture (LCC) conditions. Calu-3 cells grown under both conditions formed tight monolayers and appeared physiologically similar by SEM and immunocytochemical staining against cell junctional proteins and prosurfactant protein-C.
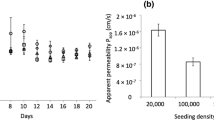
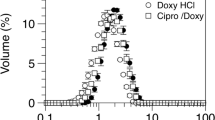
Results. Aerosolized large porous particles (LPP) deposited homogeneously and reproducibly on the cell surface and caused no apparent damage to cell monolayers by SEM and light microscopy. However, monolayers initially grown under LCC conditions showed a significant decrease in barrier properties within the first 90 min after impingement with microparticles, as determined by transepithelial electrical resistance (TEER) measurements and fluorescein-sodium transport. Conversely, AIC grown monolayers showed no significant change in barrier properties within the first 90 min following particle application. A dense mucus coating was found on AIC grown Calu-3 monolayers, but not on LCC grown monolayers, which may protect the cell surface during particle impinging.
Conclusions. This in vitro model, based on AIC grown Calu-3 cells, should allow a more relevant and quantitative characterization of therapeutic aerosol particles intended for delivery to the tracheo-bronchial region of the lung or to the nasal passages. Such characterization is likely to be particularly important with therapeutic aerosol particles designed to provide sustained drug release in the lung.
Similar content being viewed by others
REFERENCES
J. S. Patton and R. Platz. Pulmonary delivery of peptides and proteins for systemic action. Adv. Drug Deliv. Rev. 8:179-196 (1992).
S. Sanjar and S. Matthews. Treating systemic diseases via the lung. J. Aerosol Med. 14:S51-S58 (2001).
J. S. Patton. Inhalation: The other “oral” route for delivery of molecules with low gastrointestinal bioavailability. Abstr. Pap. Am. Chem. Soc. 219:175(2000).
R. W. Niven. Delivery of biotherapeutics by inhalation aerosol. Crit. Rev. Ther. Drug Carrier Syst. 12:151-231 (1995).
X. M. Zeng, G. P. Martin, and C. Marriott. The controlled delivery of drugs to the lung. Int. J. Pharm. 124:149-164 (1995).
D. A. Edwards, J. Hanes, G. Caponetti, J. Hrkach, A. Ben—Jebria, M. L. Eskew, J. Mintzes, D. Deaver, N. Lotan, and R. Langer. Large porous particles for pulmonary drug delivery. Science 276:1868-1871 (1997).
R. Vanbever, A. Ben—Jebria, J. D. Mintzes, R. Langer, and D. A. Edwards. Sustained release of insulin from insoluble inhaled particles. Drug Dev. Res. 48:178-185 (1999).
E. R. Weibel. Morphometry of the Human Lung, Academic Press, New York, 1963.
J. Bastacky, C. Y. Lee, J. Goerke, H. Koushafar, D. Yager, L. Kenaga, T. P. Speed, Y. Chen, and J. A. Clements. Alveolar lining layer is thin and continuous: low-temperature scanning electron microscopy of rat lung. J. Appl. Physiol. 79:1615-1628 (1995).
J. Fogh and G. Trempe. In J. Fogh (ed.), Human Tumor Cells In Vitro, Plenum Press, New York, 1975 pp. 115-159.
B. Q. Shen, W. E. Finkbeiner, J. J. Wine, R. J. Mrsny, and J. H. Widdicombe. Calu-3: a human airway epithelial cell line that shows cAMP-dependent Cl-secretion. Am. J. Physiol. 266:L493-L501 (1994).
K. A. Foster, M. Yazdanian, and K. L. Audus. Microparticulate uptake mechanisms of in-vitro cell culture models of the respiratory epithelium. J. Pharm. Pharmacol. 53:57-66 (2001).
J. Moebius, C. Ehrhardt, I. Erler, U. F. Schaefer, and C. M. Lehr. The epithelial cancer cell line Calu-3: Characterization as an in vitro model for drug absorption in the upper airways. Arch. Pharm. Pharm. Med. Chem. 333:13(2001).
M. E. Cavet, M. West, and N. L. Simmons. Transepithelial transport of the fluoroquinolone ciprofloxacin by human airway epithelial Calu-3 cells. Antimicrob. Agents. Ch. 41:2693-2698 (1997).
B. I. Florea, I. C. van der Sandt, S. M. Schrier, K. Kooiman, K. Deryckere, A. G. de Boer, H. E. Junginger, and G. Borchard. Evidence of P-glycoprotein mediated apical to basolateral transport of flunisolide in human broncho-tracheal epithelial cells (Calu-3). Br. J. Pharmacol. 134:1555-1563 (2001).
C. Witschi and R. J. Mrsny. In vitro evaluation of microparticles and polymer gels for use as nasal platforms for protein delivery. Pharm. Res. 16:382-390 (1999).
J. Fu, J. Fiegel, E. Krauland, and J. Hanes. New polymer carriers for controlled drug delivery following inhalation or injection. Biomaterials 23:4425-4433 (2002).
J. Hanes, D. A. Edwards, C. Evora, and R. Langer. Particles incorporating surfactants for pulmonary drug delivery. U.S. Patent No. 5,855,913 (1999).
W. C. Hinds. Aerosol Technology—Properties, Behavior, and Measurement of Airborne Particles, John Wiley & Sons, Inc., New York, 1999.
C. Ehrhardt, C. Kneuer, J. Fiegel, J. Hanes, U. F. Schaefer, K. J. Kim, and C. M. Lehr. Influence of apical fluid volume on the development of functional intercellular junctions in the human epithelial cell line 16HBE14o-: implications for the use of this cell line as an in vitro model for bronchial drug absorption studies. Cell Tissue Res. 308:391-400 (2002).
K. J. Elbert, U. F. Schaefer, H. J. Schafers, K. J. Kim, V. H. L. Lee, and C. M. Lehr. Monolayers of human alveolar epithelial cells in primary culture for pulmonary absorption and transport studies. Pharm. Res. 16:601-608 (1999).
M. Yamaya, W. E. Finkbeiner, S. Y. Chun, and J. H. Widdicombe. Differentiated structure and function of cultures from human tracheal epithelium. Am. J. Physiol. 262:L713-L724 (1992).
H. Wan, H. L. Winton, C. Soeller, G. A. Stewart, P. J. Thompson, D. C. Gruenert, M. B. Cannell, D. R. Garrod, and C. Robinson. Tight junction properties of the immortalized human bronchial epithelial cell lines Calu-3 and 16HBE14o-. Eur. Respir. J. 15:1058-1068 (2000).
B. Forbes, S. Lim, G. P. Martin, and M. B. Brown. An in vitro technique for evaluating inhaled nasal delivery systems. S.T.P. Pharma. 12:75-79 (2002).
M. Kondo, W. E. Finkbeiner, and J. H. Widdicombe. Cultures of bovine tracheal epithelium with differentiated ultrastructure and ion transport. In Vitro Cell. Dev. Biol. 29A:19-24 (1993).
P. M. de Jong, M. A. J. A. van Sterkenburg, J. A. Kempenaar, J. H. Dijkman, and M. Ponec. Serial culturing of human bronchial epithelial cells derived from biopsies. In Vitro Cell. Dev. Biol. 29A:379-387 (1993).
K. J. Kim, Z. Borok, and E. D. Crandall. A useful in vitro model for transport studies of alveolar epithelial barrier. Pharm. Res. 18:253-255 (2001).
C. Ehrhardt, J. Fiegel, S. Fuchs, R. Abu-Dahab, U. F. Schaefer, J. Hanes, and C. M. Lehr. Drug absorption by the respiratory mucosa-cell culture models and particulate drug carriers. J. Aerosol Med. 15:131-139 (2002).
L. Cruewels, L. Golde, and H. Haagsman. The pulmonary surfactant system: Biochemical and clinical aspects. Lung 175:1-39 (1997).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Fiegel, J., Ehrhardt, C., Schaefer, U.F. et al. Large Porous Particle Impingement on Lung Epithelial Cell Monolayers—Toward Improved Particle Characterization in the Lung. Pharm Res 20, 788–796 (2003). https://doi.org/10.1023/A:1023441804464
Issue Date:
DOI: https://doi.org/10.1023/A:1023441804464