Abstract
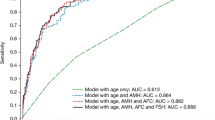
Purpose : To compare treatment-associated follicle-stimulating hormone (FSH) response in patients undergoing controlled ovarian hyperstimulation with either microdose flare (MDF) leuprolide acetate or clomiphene citrate and human menopausal gonadotropin (CC/hMG).
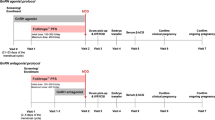
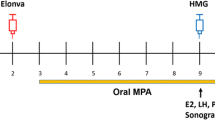
Methods : Thirteen patients who were deemed poor responders underwent stimulation with one of two poor responder stimulation protocols (MDF group: n = 8; CC/hMG group: n = 5). Serum FSH, estrone (E1), estrone sulfate (E1S), and estradiol (E2) levels were measured at baseline, day 5 of medication, and on day of hCG administration. Ovarian and uterine responses were evaluated by ultrasound.
Results : Treatment-associated FSH levels were consistently higher in the group that took CC/hMG. However, serum E1, E1S, and E2 values were similar in both groups as were the number of oocytes retrieved and the endometrial echo complex. There were no differences between the two groups with regards to the quality of the oocytes obtained, fertilization rate, or the quality of the embryos.
Conclusion : Clomiphene citrate, when administered in conjunction with exogenous hMG, is a more potent stimulator of FSH production than MDF leuprolide acetate among poor responders to ovarian stimulation. However, the number of oocytes is not increased.
Similar content being viewed by others
REFERENCES
Anserini P, Magnasco A, Remorgida V, Gaggero G, Testa D, Capitanio GL: Comparison of a blocking vs. flare-up protocol in poor responders with a normal and abnormal clomiphene citrate challenge test. Gynecol Endocrinol 1997;11:321–326
Muasher SJ: Treatment of low responders. J Assist Reprod Genet 1993;10:112–114
Jenkins JM, Davies DW, Devonport H, Anthony FW, Gadd SC, Watson RH, Masson GM: Comparison of “poor” responders with “good” responders using a standard buserelin/human menopausal gonadotrophin regime for in-vitro fertilization. Hum Reprod 1991;6:918–921
Navot D, Rosenwaks Z, Margalioth EJ: Prognostic assessment of female fecundity. Lancet 1987;2:645–647
Muasher SJ, Oehninger S, Simonetti S, Matta J, Ellis LM, Liu HC, Jones GS, Rosenwaks Z: The value of basal and/or stimulated serum gonadotropin levels in prediction of stimulation response and in vitro fertilization outcome. Fertil Steril 1988;50:298–307
Dor J, Seidman DS, Ben-Shlomo I, Levran D, Karasik A, Mashiach S: The prognostic importance of the number of oocytes retrieved and estradiol levels in poor and normal responders in in vitro fertilization (IVF) treatment. J Assist Reprod Genet 1992;9:228–232
Schoolcraft W, Schlenker T, Gee M, Stevens J, Wagley L: Improved controlled ovarian hyper-stimulation in poor responder in vitro fertilization patients with a microdose follicle-stimulating hormone flare, growth hormone protocol. Fertil Steril 1997;67:93–97
Feldberg D, Farhi J, Ashkenazi J, Dicker D, Shalev J, Ben-Rafael Z: Minidose gonadotropin-releasing hormone agonist is the treatment of choice in poor responders with high follicle-stimulating hormone levels. Fertil Steril 1994;62:343–346
Karacan M, Erkan H, Karabulut O, Sarikamis B, Camlibel T, Benhabib M: Clinical pregnancy rates in an IVF program. Use of the flare-up protocol after failure with long regimens of GnRH-a. J Reprod Med 2001;46:485–489
Land JA, Yarmolinskaya MI, Dumoulin JC, Evers JL: Highdose human menopausal gonadotropin stimulation in poor responders does not improve in vitro fertilization outcome. Fertil Steril 1996;65:961–965
Paulson RJ, Marrs RP: Ovulation stimulation and monitoring for in-vitro fertilization. Curr Probl Obstet Gynecol Infert 1986;9:497–526
Diamond MP, Hill GA, Webster BW, Herbert CM, Rogers BJ, Osteen KG, Maxson WS, Vaughn WK, Wentz AC: Comparison of human menopausal gonadotropin, clomiphene citrate, and combined human menopausal gonadotropin-clomiphene citrate stimulation protocols for in vitro fertilization. Fertil Steril 1986;46:1108–1112
Tanbo T, Dale PO, Abyholm T, Stokke KT: Follicle-stimulating hormone as a prognostic indicator in clomiphene citrate/human menopausal gonadotrophin-stimulated cycles for in-vitro fertilization. Hum Reprod 1989;4:647–650
Scott RT, Navot D: Enhancement of ovarian responsiveness with microdoses of gonadotropin-releasing hormone agonist during ovulation induction for in vitro fertilization. Fertil Steril 1994;61:880–885
Huisman GJ, Fauser BC, Eihkemans MJ, Pieters MH: Implantation rates after in vitro fertilization and transfer of maximum of two embryos that have undergone three to five days of culture. Fertil Steril 2000;73:117–122
Veeck LL: An Atlas of Human Gametes and Conceptuses. New York, Parthenon, 1998, pp 40–45
Scott RT, Jr, Hofmann GE, Oehninger S, Muasher SJ: Intercycle variability of day 3 follicle-stimulating hormone levels and its effect on stimulation quality in in vitro fertilization. Fertil Steril 1990;54:297–302
Manzi DL, Thornton KL, Scott LB, Nulsen JC: The value of increasing the dose of human menopausal gonadotropins in women who initially demonstrate a poor response. Fertil Steril 1994;62:251–256
Surrey ES, Schoolcraft WB: Evaluating strategies for improving ovarian response of the poor responder undergoing assisted reproductive techniques. Fertil Steril 2000;73:667–676
Coulam C, Stanczyk FZ, Paulson RJ: Estrone sulfate as a predictor of gonadotropin response during controlled ovarian hyperstimulation (COH). Fertil Steril 1999;71(Suppl 1):9S
Surrey ES, Bower JA, Hill DM, Ramsey J, Surrey MW: Clinical and endocrine effects of a microdose GnRH agonist flare regimen administered to poor responders who are undergoing in vitro fertilization. Fertil Steril 1998;69:419–424
Lessing JB, Peyser MR, Gilad S, Amit A, Kogosowski A, Yovel I, Barak Y, David MP: Estrone-3-glucuronide chemiluminescence immunoassay: An alternative method for monitoring induction of ovulation with human menopausal gonadotropin in an in vitro fertilization program. Fertil Steril 1987;48:450–453
Rapi S, Fuzzi B, Mannelli M, Pratesi S, Criscuoli L, Pellegrini S, Messeri G: Estrone-3-glucuronide chemiluminescence immunoassay (LIA) and 17β-estradiol radioimmunoasay (RIA) in the monitoring of superovulation for in vitro fertilization (IVF): Correlation with follicular parameters and oocyte maturity. Acta Eur Fertil 1992;23:63–68
Diamond MP, Maxson WS, Vaughn WK, Osteen KG, Wentz AC: Antiestrogenic effect of clomiphene citrate in a multiple follicular stimulation protocol. J In Vitro Fert Embryo Transf 1986;3:106–109
Maxson WS, Pittaway DE, Herbert CM, Garner CH, Wentz AC: Antiestrogenic effect of clomiphene citrate: Correlation with serum estradiol concentrations. Fertil Steril 1984;42:356–359
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Saadat, P., Slater, C.C., Jain, J.K. et al. Treatment-Associated Serum FSH Levels in Very Poor Responders to Ovarian Stimulation. J Assist Reprod Genet 20, 395–399 (2003). https://doi.org/10.1023/A:1026280508821
Issue Date:
DOI: https://doi.org/10.1023/A:1026280508821