Introduction
Elevated blood pressure is an established risk factor for developing cardiovascular disease (CVD), the leading cause of morbidity and mortality in the U.S. (Benjamin et al., Reference Benjamin, Blaha, Chiuve, Cushman, Das, Deo, de Ferranti, Floyd, Fornage, Gillespie, Isasi, Jimenez, Jordan, Judd, Lackland, Lichtman, Lisabeth, Liu, Longenecker, Mackey, Matsushita, Mozaffarian, Mussolino, Nasir, Neumar, Palaniappan, Pandey, Thiagarajan, Reeves, Ritchey, Rodriguez, Roth, Rosamond, Sasson, Towfighi, Tsao, Turner, Virani, Voeks, Willey, Wilkins, Wu, Alger, Wong and Muntner2017). However, preventing high blood pressure remains a major public health challenge (Chobanian et al., Reference Chobanian, Bakris, Black, Cushman, Green, Izzo, Jones, Materson, Oparil, Wright and Roccella2003). Blood pressure tends to increase with age (Chobanian et al., Reference Chobanian, Bakris, Black, Cushman, Green, Izzo, Jones, Materson, Oparil, Wright and Roccella2003) and current trends show a rising prevalence of hypertension in younger adults (Yano et al., Reference Yano, Stamler, Garside, Daviglus, Franklin, Carnethon, Liu, Greenland and Lloyd-Jones2015). Higher blood pressure in early adulthood persists into later adulthood and inflates CVD risk beyond the effects of hypertension in middle adulthood (Gray et al., Reference Gray, Lee, Sesso and Batty2011). Thus, if age-related increases in blood pressure could be prevented or lessened, the burden of CVD might be substantially reduced (Rieder, Reference Rieder2007; Institute of Medicine, 2010). Certain populations have also been identified as having elevated risk of developing hypertension relatively early in life, including those exposed to major occupational stressors, like service members and veterans (Yu et al., Reference Yu, Ravelo, Wagner, Phibbs, Bhandari, Chen and Barnett2003; Shrestha et al., Reference Shrestha, Ho, Vie, Labarthe, Scheier, Lester and Seligman2019). Besides occupational status, other sociodemographic correlates of high blood pressure have been identified. Higher rates of hypertension occur in younger men v. women and early-onset hypertension is more common in Blacks relative to Whites, although less is known about premature risk in other racial groups (e.g. Hispanic and Asian) (Benjamin et al., Reference Benjamin, Blaha, Chiuve, Cushman, Das, Deo, de Ferranti, Floyd, Fornage, Gillespie, Isasi, Jimenez, Jordan, Judd, Lackland, Lichtman, Lisabeth, Liu, Longenecker, Mackey, Matsushita, Mozaffarian, Mussolino, Nasir, Neumar, Palaniappan, Pandey, Thiagarajan, Reeves, Ritchey, Rodriguez, Roth, Rosamond, Sasson, Towfighi, Tsao, Turner, Virani, Voeks, Willey, Wilkins, Wu, Alger, Wong and Muntner2017). To date, strategies to reduce hypertension risk have had limited success, with more attention focused on treatment than prevention (Rieder, Reference Rieder2007; Institute of Medicine, 2010). Consequently, recent work has sought to identify modifiable protective factors, particularly for younger, healthy individuals at risk of early-onset hypertension.
Preliminary research has suggested psychological health plays a role in hypertension onset, particularly in the military. For example, one study found a three-fold increase in hypertension risk among veterans with post-traumatic stress disorder (PTSD) or other psychiatric diagnoses; strikingly, these veterans were, on average, 31 years of age (Cohen et al., Reference Cohen, Marmar, Ren, Bertenthal and Seal2009). A national cohort study of 1 547 182 Swedish military male conscripts found those with low v. high resilience to stressors at age 18 had over 40% excess hypertension risk over 26 years of follow-up (Crump et al., Reference Crump, Sundquist, Winkleby and Sundquist2016). This work suggests some psychological factors may reduce risk. One such factor is dispositional optimism, the tendency to believe good events are likely and bad events are unlikely (Carver et al., Reference Carver, Scheier and Segerstrom2010). Shaped by social experiences (Boehm et al., Reference Boehm, Chen, Williams, Ryff and Kubzansky2015), optimism tends to be stable starting in young adulthood. However, it is also modifiable via active interventions (Meevissen et al., Reference Meevissen, Peters and Alberts2011) and has consistently demonstrated protective effects against incident coronary heart disease and stroke (Boehm and Kubzansky, Reference Boehm and Kubzansky2012). Most studies of optimism and hypertension have been cross-sectional and conducted with older adults (Trudel-Fitzgerald et al., Reference Trudel-Fitzgerald, Gilsanz, Mittleman and Kubzansky2015). The only published prospective study found no relationship across 12 years in a sample of mid-life professional adults, although optimism was assessed with only a single item (Trudel-Fitzgerald et al., Reference Trudel-Fitzgerald, Boehm, Kivimaki and Kubzansky2014).
Examining optimism's association with incident hypertension risk may provide insight into novel targets for the prevention of a highly prevalent condition. In this study, we hypothesised higher optimism would be associated with reduced risk of developing hypertension in a young and diverse sample of 103 486 U.S. Army active-duty soldiers, a population at high risk of early-onset hypertension (Stewart et al., Reference Stewart, Sosnov, Howard, Orman, Fang, Morrow, Zonies, Bollinger, Tuman, Freedman and Chung2015). We used a multi-item measure of dispositional optimism and evaluated associations among initially healthy participants. Following previous research, we included multiple potential confounders (e.g. family history of CVD) and variables that might lie on the pathway linking optimism to hypertension risk (e.g. cigarette smoking) (Cohen et al., Reference Cohen, Marmar, Ren, Bertenthal and Seal2009; Trudel-Fitzgerald et al., Reference Trudel-Fitzgerald, Gilsanz, Mittleman and Kubzansky2015). We further adjusted for possible confounding by depression, which has been linked with both lower optimism and increased hypertension risk (Trudel-Fitzgerald et al., Reference Trudel-Fitzgerald, Gilsanz, Mittleman and Kubzansky2015). In secondary analyses, we assessed whether the primary association would hold after accounting for baseline blood pressure and, separately, whether the association differed depending on race/ethnicity, sex or age.
Methods
Participants
Data are from a large cohort of active-duty U.S. Army soldiers followed for up to five years. Every year, soldiers complete the global assessment tool (GAT), a self-report questionnaire assessing psychosocial functioning (Peterson et al., Reference Peterson, Park and Castro2011). During the study baseline 284 620 Army active-duty soldiers, age 17–65 years, completed the GAT (May 2009–April 2010) and indicated their responses could be used for research purposes. In this population of soldiers with the majority younger than age 30, approximately 8.7% had hypertension at study baseline, which is comparable to estimates of hypertension rates in the civilian population. For example, the National Health and Nutrition Examination Survey reported the prevalence of hypertension in men and women age 20–44 years was 10.5% (AHA Centers for Health Metrics and Evaluation, 13 November 2017). After excluding soldiers with hypertension, suspected hypertension derived from related conditions or CVD at baseline (n = 24 903) or without relevant health information at baseline (n = 156 231), we retained 103 486 soldiers for analysis (Fig. 1). Comparing soldiers included v. excluded because of missing health information [i.e. a missing periodic health assessment (PHA)] at baseline, few differences were evident (see online Supplementary Table S1). Excluded soldiers had more deployments and days deployed, perhaps explaining why they were less likely to have a baseline PHA.

Fig. 1. Study population flow chart. Diagram showing how we derived the analytic sample. Soldiers missing a PHA may have completed their physical sometime leading up to or shortly after the specified 12-month baseline window. The PHA includes measures of family history of CVD, diabetes status, BMI, smoking, alcohol misuse, SBP and DBP. GAT: global assessment tool; HT: hypertension; CVD: cardiovascular disease.
The current study is part of a military–civilian collaboration between the Army and the University of Pennsylvania and was approved by the University of Pennsylvania Institutional Review Board and a DOD Human Research Protection Official.
Measures
Optimism
Optimism was measured in the GAT using a modified version of the revised life orientation test (Scheier et al., Reference Scheier, Carver and Bridges1994). Internal consistency was acceptable (α = 0.74). After reverse scoring negatively-worded items, we obtained the mean of the item responses and standardised the overall scores (higher scores indicate higher optimism). To assess discontinuous or threshold effects, we also created quintiles of optimism scores based on the distribution of unstandardised scores in the analytic sample (range = 1–5): low (score < 3), low–moderate (score = 3), moderate (3 < score < 4), moderate–high (4 ⩽ score ⩽ 4.5) and high (score > 4.5). Prior work has demonstrated that optimism tends to be stable over time (Scheier and Carver, Reference Scheier and Carver2018).
Hypertension
Relevant diagnosis and medication data were obtained from electronic health records collected in the Military Health System Data Repository (MDR). The MDR records all outpatient and inpatient medical encounters and medications dispensed to soldiers and reimbursed by TRICARE, the military health insurer (Vie et al., Reference Vie, Scheier, Lester, Ho, Labarthe and Seligman2015). Hypertensive cases through the follow-up period (through 30 April 2014) were defined according to whether a soldier received a hypertension diagnosis using the International Classification of Diseases, Ninth-Revision, Clinical Modification (ICD-9-CM; code 401) or a prescription for antihypertensive medication.
Additionally, measured blood pressure was obtained from the PHA, a health assessment soldiers complete with an Army healthcare provider annually. For some analyses, we considered measured blood pressure as an additional criterion for identifying hypertension cases. Those with blood pressure readings over clinical cut-points of both 140 mmHg [systolic blood pressure (SBP)] and 90 mmHg [diastolic blood pressure (DBP)] were also considered hypertensive. Measured blood pressure was also used to identify individuals with baseline prehypertension (⩾120 mmHg SBP or ⩾80 mmHg DBP).
Covariates
Covariates were assessed at baseline unless otherwise indicated. Demographic characteristics obtained from the GAT included sex (men and women), age (years), and rank (officer and enlisted). Other characteristics obtained from electronic administrative records housed at the Defense Manpower Data Center included self-identified race/ethnicity (White, Black, Hispanic, Asian and others), educational attainment (<high school diploma, high school diploma, some college or associate of Arts degree, ⩾college degree) and marital status (married/not married). We used the number of deployments and the total number of days deployed prior to each soldier's baseline GAT (beginning in September 2001), obtained from the Defense Manpower Data Center, to derive a measure of the average length of deployment prior to the baseline GAT. Family history of CVD and participants’ baseline diabetes status were each self-reported with a single item on the PHA. Baseline depression status was assessed according to the presence or absence of a depression diagnosis in the MDR (ICD-9-CM: 296.2, 296.3, 300.4 or 311).
Potential pathway variables included healthy behaviours and related conditions. On the PHA, current cigarette smoking status was assessed using a single self-report item (yes/no) and alcohol misuse was measured with the validated three-item alcohol use disorders identification test (AUDIT-C), which queried alcohol frequency, quantity consumed and binge drinking (Bush et al., Reference Bush, Kivlahan, McDonell, Fihn and Bradley1998). Following prior work, AUDIT-C scores were dichotomised using screening thresholds for alcohol misuse (⩾4 in men; ⩾3 in women) (Bradley et al., Reference Bradley, DeBenedetti, Volk, Williams, Frank and Kivlahan2007). Body mass index (BMI) in kg/m2 was derived from height and weight measurements taken by an Army professional close in time to the soldier's baseline PHA. Given stringent muscular strength, endurance and cardiovascular respiratory fitness requirements for active-duty Army soldiers, we did not adjust for physical activity.
Statistical analyses
We analysed data in the person-event data environment, a secure, cloud-based environment that houses Army workforce, medical and personnel data (Vie et al., Reference Vie, Scheier, Lester, Ho, Labarthe and Seligman2015). Using SAS 9.4, Cox proportional-hazard models estimated the hazard ratios (HRs) and 95% confidence intervals (CIs) for associations between optimism, assessed at the 2009–2010 baseline, and incident hypertension. Soldiers were followed until diagnosis of hypertension, separation from Army service, death or end of follow-up (fixed censoring date of 30 April 2014), whichever occurred first. Multiple imputation procedures were used to handle missing values on BMI (missing: 31.45%), as well as other variables with fewer missing values (⩽1%). Parameter estimates from ten imputed datasets were pooled (Schafer, Reference Schafer1999).
We examined three nested models: (1) an age-adjusted model; (2) a confounder model that was adjusted for age, demographic factors (sex, race/ethnicity, education and marital status) and other potential confounders (officer rank, average length of deployment, diabetes status, family history of CVD and depression status); and (3) a pathway model that included all variables from model 2 along with BMI, cigarette smoking status and alcohol misuse. Separate model sets were run using optimism either as a standardised, continuous variable or as quintiles to assess possible discontinuous effects. An examination of the correlation between the Schoenfeld residuals and functions of time in the primary model supported the assumption of proportional hazards (the highest absolute correlation was 0.05) (Schoenfeld, Reference Schoenfeld1982).
We ran three additional sets of analyses to refine the primary models described above. First, we examined the role of blood pressure in two ways: we added SBP and DBP as additional covariates in models 1–3 and, separately, we included blood pressure levels as a defining criterion for hypertension in the covariate-adjusted model (model 2). Second, to assess if effects were similar across demographic subgroups when adjusting for confounders, we included an interaction term (or terms) for optimism (continuous) with race/ethnicity (White, Black, Hispanic, Asian and others), sex (men and women) or age (continuous). We also assessed potential effect modification by running separate confounder-adjusted models stratified by race/ethnicity, sex, or age (⩽30 and >30 years). Third, to reduce concerns about reverse causality (i.e. subclinical hypertension influencing optimism levels), we ran each model excluding hypertension cases that developed within two years of baseline. Separately, we also ran the three main nested models excluding individuals with prehypertension at baseline.
Results
At the 2009–2010 baseline, a majority of soldiers (64%) were ⩽30 years of age (mean age 28.96 years, range = 17–65), men (83.24%) and White (61.76%). Mean BMI was 26.58 kg/m2 [standard deviation (s.d.) = 3.66], 24% of participants reported a family history of CVD and very few reported diabetes (0.29%). Table 1 shows the distribution of covariates across optimism quintiles. Individuals with high optimism levels were more likely to be older, have at least a college education, be an officer, not be depressed, not be a current smoker and not misuse alcohol. Over a mean follow-up period of 3.51 years (s.d. = 1.23), 15 052 soldiers developed hypertension (14.54%). Notably, soldiers with hypertension at baseline (i.e. those excluded from this study) had nearly identical optimism scores as the hypertension-free soldiers included in this study (3.59 v. 3.61).
Table 1. Distribution of covariates at baseline (2009–2010) according to the levels of optimism

Values are either mean (s.d.) or n (%). N = 103 486.
Note: non-imputed data are reported for descriptive purposes. Percentages refer to the column percent of individuals within each optimism category with that characteristic.
BMI, body mass index; BP, blood pressure; CVD, cardiovascular disease; Q, quintile; s.d., standard deviation.
Optimism and incident hypertension
In the age-adjusted model, we observed a 13% decreased risk of incident hypertension with each 1-s.d. increase in the optimism score (HR = 0.87; 95% CI = 0.85–0.88). This estimate was slightly attenuated but remained statistically significant after adjusting for demographics and health conditions, as well as for healthy behaviours that might lie on the pathway (see Table 2 and online Supplementary S2). It is noteworthy that optimism was associated with reduced risk of hypertension independent of depression diagnosis (also significantly associated with higher hypertension risk; HR = 1.66; 95% CI = 1.56–1.76).
Table 2. HRs (95% CIs) for the association between optimism and incident hypertension, 2009–2014
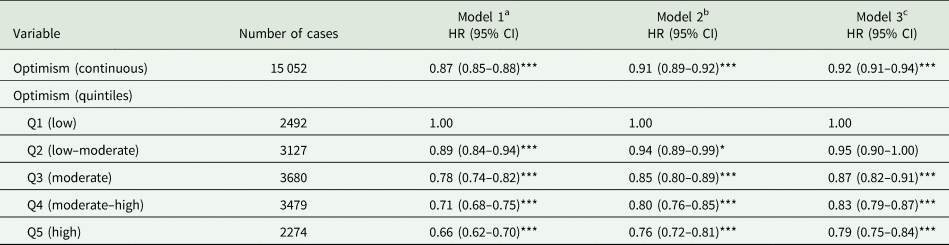
N = 103 486.
HR, hazard ratio; CI, confidence interval, Q: quintile.
a Adjusted for age.
b Adjusted for age, sex, race/ethnicity, education, marital status, rank, average deployment length prior to baseline, diabetes status, family history of CVD and depression.
c Adjusted for model 2 covariates as well as BMI, smoking status and alcohol misuse.
*p < 0.05, **p < 0.01, ***p < 0.001.
Additionally, findings with optimism quintiles demonstrated a 34% reduction in subsequent hypertension risk for the highest v. lowest optimism quintiles in the age-adjusted model (HR = 0.66; 95% CI = 0.62–0.70). Relative to the lowest optimism quintile, all other optimism quintiles were also significantly associated with a reduced risk of hypertension in the age-adjusted model. After further adjusting for potential confounders, a dose–response relationship remained evident with each increase in optimism quintile associated with a lower relative risk (p for trend <0.001). Optimism's association with hypertension risk remained statistically significant but was somewhat attenuated after additionally adjusting for healthy behaviours that might lie on the pathway (see Table 2). Figure 2 illustrates the estimated survival probability of incident hypertension for individuals within each optimism quintile.

Fig. 2. Unadjusted Kaplan–Meier survival curve for optimism and incident hypertension. Estimated survival probability of incident hypertension according to the level of optimism, with individuals with higher optimism at lower risk of developing hypertension.
Additional analyses
Adding measured levels of SBP and DBP to our primary models demonstrated higher SBP (HR = 1.02; 95% CI = 1.02–1.02) and DBP (HR = 1.03; 95% CI = 1.02–1.03) were each uniquely associated with increased hypertension risk in the confounder-adjusted model, and findings were virtually identical in fully adjusted models. However, even after including measured SBP and DBP at baseline in the confounder-adjusted model, optimism remained significantly associated with lower hypertension risk (per 1-s.d., HR = 0.91; 95% CI = 0.90–0.93; highest v. lowest optimism quintile, HR = 0.76; 95% CI = 0.72–0.81). See Table 3. Additionally, in separate confounder-adjusted models, optimism remained significantly associated with lower hypertension risk when thresholds according to measured SBP and DBP were included as part of the defining criteria for hypertension case status (per 1-s.d. optimism, HR = 0.92; 95% CI = 0.90–0.93; highest v. lowest optimism quintile, HR = 0.78; 95% CI = 0.74–0.83).
Table 3. Association between optimism and incident hypertension while adjusting for baseline SBP and DBP, 2009–2014

N = 103 486.
HR, hazard ratio; CI, confidence interval, Q: quintile.
a Adjusted for age, SBP and DBP.
b Adjusted for age, SBP, DBP, sex, race/ethnicity, education, marital status, rank, average deployment length prior to baseline, diabetes status, family history of CVD and depression.
c Adjusted for model 2 covariates as well as BMI, smoking status and alcohol misuse.
*p < 0.05, **p < 0.01, ***p < 0.001.
We observed a statistically significant interaction of optimism with age (p = 0.01) and with being Black (p < 0.001) compared to being White, but not with sex (p = 0.58) or with being Asian (p = 0.29). In age-stratified analyses, associations of optimism with the risk of developing hypertension were somewhat stronger in soldiers >30 years relative to younger soldiers (Table 4). Although associations of optimism with hypertension risk were largely similar across racial/ethnic groups relative to Whites (Table 4), the HR for optimism was slightly attenuated (but still statistically significant) for Blacks. Optimism was not significantly associated with hypertension risk among Asians; however, there were fewer cases of hypertension documented among Asians during follow-up (n = 450), relative to other racial/ethnic groups.
Table 4. Association between optimism (per 1 s.d.) and incident hypertension, modelled separately within categories of race/ethnicity, sex and age, 2009–2014
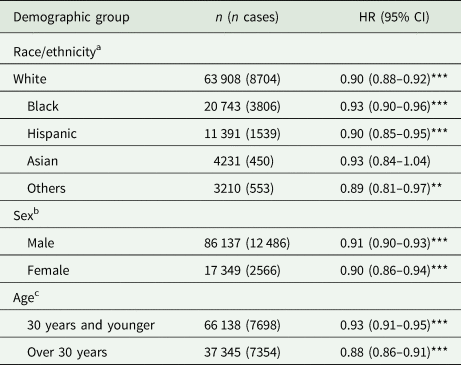
HR, hazard ratio; CI, confidence interval, s.d., standard deviation.
a Adjusted for demographics (age, sex, education and marital status), rank, average deployment length prior to baseline, diabetes status, family history of CVD and depression.
b Adjusted for demographics (age, race/ethnicity, education and marital status), rank, average deployment length prior to baseline, diabetes status, family history of CVD and depression.
c Adjusted for demographics (age, sex, race/ethnicity, education and marital status), rank, average deployment length prior to baseline, diabetes status, family history of CVD and depression.
*p < 0.05, **p < 0.01, ***p < 0.001.
After excluding hypertension cases that developed within the first two years of baseline, optimism remained associated with an increased risk of developing hypertension. Specifically, after adjusting for potential confounders (i.e. model 2), estimates were somewhat attenuated but still statistically significant (per 1-s.d., HR = 0.93; 95% CI = 0.91–0.95; highest v. lowest optimism quintile, HR = 0.81; 95% CI = 0.75–0.88). Similarly, optimism remained significantly associated with hypertension risk after excluding individuals with prehypertension at baseline (model 2, per 1-s.d. of optimism, HR = 0.88; 95% CI = 0.85–0.91; highest v. lowest optimism quintile, HR = 0.71; 95% CI = 0.63–0.80).
Discussion
This study provides consistent evidence that optimism is prospectively associated with reduced risk of hypertension over a four-year period in a large sample of initially healthy Army soldiers. Particularly noteworthy is that higher optimism levels were associated with reduced risk across a diverse set of individuals, including young men and women, as well as Blacks, Whites, and Hispanics. Effects were somewhat stronger in individuals over age 30, but still evident among younger soldiers. Moreover, associations were independent of conventional cardiovascular risk factors (including measured baseline blood pressure levels), length of deployment, Army rank and depression. Given depression was also significantly associated with increased hypertension risk; our findings may suggest optimism leads to health benefits beyond simply marking the absence of depression or other mental health disorders. Including health behaviours attenuated associations somewhat; however, estimates remained statistically significant, suggesting the possibility of other mechanisms at play. These findings are consistent with other research demonstrating independent associations of optimism with other cardiovascular outcomes including coronary heart disease (Boehm and Kubzansky, Reference Boehm and Kubzansky2012; Carver and Scheier, Reference Carver and Scheier2014).
The rate of incident hypertension in the current sample (14.5%) is higher than has been noted in civilian populations of comparable age. For example, in participants age 18–30 entering the coronary artery risk in young adults study, the ten-year incidence of hypertension ranged from 3.2% in White women to 7.8% in White men and 16.4% in Black men (Dyer et al., Reference Dyer, Liu, Walsh, Kiefe, Jacobs and Bild1999). However, other research suggests soldiers exposed to high levels of combat stressors and related distress develop hypertension at higher rates. For example, one study (n = 303 223; mean age 31 years) reported 15.6% prevalence of hypertension among U.S. veterans with a mental health diagnosis excluding PTSD and 30.8% prevalence among those with PTSD with or without another mental health diagnosis (Cohen et al., Reference Cohen, Marmar, Ren, Bertenthal and Seal2009). In a cross-sectional study also drawing on data from active-duty U.S. Army soldiers but weighted to the 2012 U.S. Army active-duty population, 5% of soldiers were estimated to have hypertension and 64.7% were estimated to be pre-hypertensive at the time of assessment in 2012 (Shrestha et al., Reference Shrestha, Ho, Vie, Labarthe, Scheier, Lester and Seligman2019). Thus, findings from this sample do support the notion that individuals in the military are at higher risk of developing hypertension relatively early in life.
One key pathway linking optimism with reduced hypertension risk may operate by increasing healthy behaviours. Numerous studies indicate optimists are more likely to have healthier diets, exercise more and obtain adequate sleep (Kelloniemi et al., Reference Kelloniemi, Ek and Laitinen2005; Steptoe et al., Reference Steptoe, Wright, Kunz-Ebrecht and Iliffe2006; Trudel-Fitzgerald et al., Reference Trudel-Fitzgerald, James, Kim, Zevon, Grodstein and Kubzansky2019), while less likely to engage in behaviours that jeopardise health, like excess alcohol consumption or smoking (Carvajal et al., Reference Carvajal, Wiatrek, Evans, Knee and Nash2000; Steptoe et al., Reference Steptoe, Wright, Kunz-Ebrecht and Iliffe2006; Trudel-Fitzgerald et al., Reference Trudel-Fitzgerald, James, Kim, Zevon, Grodstein and Kubzansky2019). A recent meta-analysis found more v. less optimistic individuals tend to engage in healthier behaviours that protect against CVD, although effect sizes were modest (Boehm et al., Reference Boehm, Chen, Koga, Mathur, Vie and Kubzansky2018). In line with these findings, we found healthy behaviours partially but not fully attenuated associations in our study. Optimism may also increase the likelihood of healthier biological function by buffering the cardiotoxic effects of stressors and psychological distress or improving endothelial function (Kubzansky et al., Reference Kubzansky, Huffman, Boehm, Hernandez, Kim, Koga, Feig, Lloyd-Jones, Seligman and Labarthe2018).
Because many of the conventional risk factors for hypertension and CVD – including diet, exercise, and obesity – are difficult to change (Fjeldsoe et al., Reference Fjeldsoe, Neuhaus, Winkler and Eakin2011), identifying an upstream determinant of behaviour-related factors may offer critical insights for interventions to reduce risk. Optimism has been described as a unique factor that directly contributes to the transformation of goals into behaviours (Scheier and Carver, Reference Scheier and Carver1987). It is partially heritable (Plomin et al., Reference Plomin, Scheier, Bergeman, Pederson, Nesselroade and McClearn1992) but can also be learned (Murphy et al., Reference Murphy, O'Donoghue, Drazich, Blackwell, Nobre and Holmes2015; Peters et al., Reference Peters, Flink, Boersma and Linton2010) and changed over extended time periods, especially in adulthood (Mroczek, Reference Mroczek2014). Moreover, optimism can be modified intentionally with relatively low-burden strategies, including expressing gratitude or meditating, as well as by more resource-intensive strategies like engaging in cognitive-behavioural or well-being prevention and therapy programmes (Peters et al., Reference Peters, Flink, Boersma and Linton2010; Ruini and Fava, Reference Ruini and Fava2012). A critical next step is to evaluate if interventions to improve optimism translate into health benefits.
The present study has some limitations including a relatively short follow-up period. Because our sample comprised a high proportion of men with high school level education and good initial physical condition, this study's internal validity is enhanced, but findings may not be generalisable. Due to the stability of optimism scores across years (Scheier and Carver, Reference Scheier and Carver2018) and the brief follow-up period, we could not assess whether a change in optimism was associated with altered risk of subsequently developing hypertension. Given that optimism remained a significant predictor of hypertension risk even after adjusting for measured blood pressure at baseline, removing hypertension cases within two years of baseline, and, separately, removing prehypertension cases at baseline, it is unlikely hypertension played a causal role in observed optimism levels. Current findings are based on observational data and cannot rule out the possibility of unmeasured confounding. However, with longer follow-up, future studies may assess whether changes in optimism affect hypertension risk, providing stronger evidence for a causal relationship. Additionally, because this study relied on measured blood pressure obtained from medical records, assessed as part of a clinical examination, this measure may not be directly comparable to one obtained solely for research purposes. However, empirical tests of the measure were reassuring, as we found the association between optimism and HT held when blood pressure was added as an indicator of HT, and blood pressure measures were associated with HT risk, as obtained from the MDR. Methodological strengths include an examination of a large, diverse sample of younger adults serving in the Army uniquely at risk for hypertension. This is one of the first studies to examine associations not only in Whites and Blacks but also in Hispanics and Asians. Moreover, the study was prospective and assessed numerous potential confounding and pathway variables.
Conclusion
Given that hypertension developed in younger adulthood may be particularly pernicious and that individuals involved in stressful jobs may be at elevated risk for early-onset hypertension (Cuevas et al., Reference Cuevas, Williams and Albert2017), identifying protective factors that reduce risk in these populations is urgent. Rates of incident hypertension in this population of U.S. soldiers were striking. Nonetheless, we found higher optimism was associated with reduced incident hypertension risk, over and above a range of potential confounders and pathway-related variables. Protective associations of optimism were evident even within these young and initially healthy individuals who were likely exposed to trauma and stressors over follow-up. While the effect size was modest, the consistency of the associations across multiple racial/ethnic, age and sex groups suggests findings are robust. Prior work indicates that every 10 mmHg SBP reduction leads to approximately 20% reduction in CVD risk, 27% reduction in stroke risk and 17% reduction in coronary heart disease risk (Ettehad et al., Reference Ettehad, Emdin, Kiran, Anderson, Callender, Emberson, Chalmers, Rodgers and Rahimi2016). We found for every s.d. of optimism, hypertension risk was reduced by 8–13% depending on the covariates included. Identifying individuals with lower optimism levels in early adulthood may serve not only as a sign that action is needed to improve their psychological health but also as the ‘canary in the coal mine,’ providing an early alarm that lifelong cardiovascular health may be at risk. These findings, together with other work demonstrating optimism is a modifiable health asset, suggest optimism may be a valuable target for public health intervention.
Supplementary material
The supplementary material for this article can be found at https://doi.org/10.1017/S2045796020000621
Availability of data and materials
Under US Army policy, the data will not be made available to other researchers for purposes of reproducing the results.
Acknowledgements
We acknowledge the support provided to this project by men and women of the Office of the Deputy Under Secretary of the Army, the Army Analytics Group and Research Facilitation Laboratory. We thank Dr Les McFarling and Captain Kristin Saboe from the Army Resiliency Directorate for assisting in acquiring GAT data and Dr Douglas Bonett for statistical guidance.
Financial support
This publication stems from a military–civilian collaboration supported in part by the Robert Wood Johnson Foundation through a grant to the University of Pennsylvania, M.E.P. Seligman, Principal Investigator. This work was also supported by the Fonds de Recherche du Québec – Santé (Quebec, Canada) under a postdoctoral fellowship awarded to Claudia Trudel-Fitzgerald.
Conflict of interest
The U.S. Department of Defense (DOD) does not exercise any editorial, security, or other control over information in this article. Authors assume responsibility for the veracity, accuracy and source documentation of material, including no use of classified material and conformity to copyright and usage permissions. Views expressed in this article are those of the authors and do not necessarily represent the official policy of the Department of the Army, DOD, or U.S. Government. Dr Seligman reported the following: (1) University of Pennsylvania has a proprietary interest in the program Master Resilience Training, the backbone of the US Army's Comprehensive Soldier Fitness program; (2) University of Pennsylvania licenses such resilience and positive psychology training programs to private companies, and Dr Seligman receives a nominal fee from the university for some of these; (3) Dr Seligman is often paid to give speeches where he mentions resilience and resilience training. No other disclosures were reported.
Ethical standards
The authors assert all procedures contributing to this work comply with the ethical standards of the relevant national and institutional committees on human experimentation and with the Helsinki Declaration of 1975, as revised in 2008.










