Abstract
N-methyl D-aspartate (NMDA)-antagonists decrease neurotoxicity by inhibiting Ca2+ influx which is of interest for the treatment of acute cerebrovascular insults and chronic neurodegenerative disorders. Currently, there is no surrogate marker for quantification of NMDA-receptor–mediated drug effects, which hampers dose-finding clinical studies. As prolactin and cortisol liberation is in part influenced through NMDA-receptors we investigated whether the elevation of prolactin or cortisol plasma levels is a class effect of NMDA-antagonists and might be an appropriate marker for studying NMDA-antagonistic potency. Fifteen healthy male volunteers participated in this placebo-controlled, randomized, three-way crossover trial. Ketamine (0.5mg/kg), memantine (0.16 mg/kg; i.e., a well tollerated standard dose) or placebo were infused over 60 min. Ketamine increased serum prolactin and cortisol levels (p < 0.001), whereas memantine and placebo did not affect hormone levels. Further studies are needed to define whether higher doses of memantine or other NMDA antagonists can induce hormone release.
Similar content being viewed by others
Main
Overstimulation of the N-methyl-D-aspartate (NMDA) receptor, a subtype of glutamate receptors, leads to excessive entry of calcium ions into neurons causing subsequent cell damage. This mechanism of neurotoxicity is associated with acute and chronic neurodegenerative disorders (Danysz and Parsons 1998) and schizophrenia (Abi-Saab et al. 1998), so that NMDA receptors are potential pharmacological targets.
There are currently no biologic markers available to quantify the potency of NMDA antagonists. Yet, NMDA receptors are involved in the physiologic pulsatile regulation of hormone release from the hypothalamo-pituitary-axis (Arslan et al. 1992; Bhat et al. 1995, Jezova et al. 1991). Measurement of prolactin and cortisol levels may thus reveal a drug's possible NMDA receptor antagonistic potency. Additionally, hormone levels would be readily accessible parameters for dose finding studies and for establishing minimally effective concentrations of certain NMDA antagonists.
In this study we investigated whether the rise in prolactin and/or cortisol serum levels could be a class effect of NMDA-antagonists. We thus compared the effects of two well known NMDA-antagonists, ketamine and memantine, on prolactin and cortisol release, though they show different interactions with the glycin-binding sites (Danysz and Parsons 1998), different degrees of trapping in the ion channel and differences in their binding affinities and receptor blocking actions (Mealing et al. 1999).
METHODS
Subjects
The sample size of 15 subjects was based on a previous study investigating the endocrine effects of ketamine (Krystal et al. 1994). The study protocol and informed consent form were approved by the local Ethics Committee, and all subjects undersigned the nine pages of the informed consent in the presence of a physician and a witness. All subjects underwent a battery of laboratory and physical screening tests as described previously (Jilma et al. 1996). Inclusion criteria were healthy, as defined by the absence of disease, male sex, age 19-35 years, drug free. Subjects had a body mass index of 22.8 ± 0.5 kg/m2 (mean ± SD). A psychiatric examination (open questions concerning familial and medical history, International Personality Disorders Examination and Structured Clinical Interview for DMS) was performed because NMDA-antagonists can dose-dependently provoke psychotomimetic effects (Krystal et al. 1994, 1999; Newcomer et al. 1999). Any evidence of prior or active psychiatric disorder or family history of such was defined as exclusion criterion.
Study Design
The study was placebo-controlled, balanced-randomized (by randomization tables), three-way crossover with a wash-out period of at least six days between study-days.
Experimental Procedures and Medications
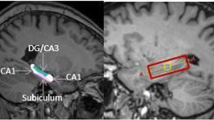
Volunteers reported at 07:45, a.m. on each trial day to the study ward. An indwelling catheter (21 gauge) was inserted and after a 1 hr resting-period ketamine (Ketalar® 0.5 mg/kg, Parke Davis), memantine (Akatinol Memantine Injektionslösung® 0.16 mg/kg, Merz & Co) or placebo (physiologic saline solution) were infused over 60 min. Blood was sampled twice at 10 min. intervals before infusion of any drug and for 2h after the start of infusion (Figure 1). Blood pressure was measured at 5 min intervals, a real time ECG was monitored continuously and pulse rate was recorded from a finger pulse-oxymeter on a HP-CMS monitor system (Hewlett Packard, Palo Alto, CA).
Methods
Cortisol and prolactin serum levels were measured by enzyme immunoassay (Enzymun-Test™Cortisol and Prolactin, Boehringer Mannheim Immundiagnostica, limit of sensitivity: 27.6nmol/L and 1ng/mL, respectively). Intra-assay coefficients of variation (CV) were <2% and inter-assay CV were <7%.
Data Analysis
Treatment effects on hormone levels and cardiovascular parameters are described as means±SEM. We used a two-way ANCOVA for analysis of treatment effects (treatment = indepedent factor, subject = covariate, outcome variable = dependent factor in a repeated measures design). A p-value of 0.05 was considered significant. F-values are provided for main effects.
RESULTS
Basal serum cortisol and prolactin levels were not significantly different between periods.
Prolactin
Prolactin levels steadily declined during placebo and memantine infusion with nadir levels seen at 120min. In contrast, ketamine increased prolactin serum levels after 40 min of infusion, which differed significantly from the decrease observed after memantine and placebo infusion (F = 3.66, [df = 12], p < .001; Figure 1)
Cortisol
Cortisol levels steadily declined during placebo and memantine infusion with nadir levels at 80 min. In contrast ketamine increased cortisol serum levels at 60 min after infusion, which differed significantly from the decrease observed after memantine or placebo infusion (F = 7.68, [df = 12]; p < .001; Figure 1).
Effects on Blood Pressure and Pulse Rate
Ketamine, but not placebo or memantine, infusion increased systolic (F = 5.56) and diastolic blood pressure (F = 2.16) and heart rate (F = 3.00) on average by 10–15% ([df = 16] and p < .001 in all cases; Figure 2).
Drug-tolerability
The ketamine infusion was discontinued in two subjects after minor adverse events. Sweating, dizziness, and paresthesia in the finger tips and around the mouth were reported; all data were included in an intention to treat analysis and the last observation was carried forward. No adverse events were reported during memantine infusion.
DISCUSSION
Ketamine increased prolactin and cortisol levels, which is in good agreement with data obtained by Krystal et al. (1994). In contrast, no significant differences were observed between the memantine and placebo period (p < .827). The fall in plasma prolactin and cortisol levels in the memantine and placebo groups represents well-known circadian changes (Miyatake et al. 1980).
This study demonstrates that tolerable doses of two non-competitive open ion channel blocking NMDA-antagonists can provoke different hormonal release reactions in healthy volunteers (Figure 1).
First, it is a clear limitation of our study that we examined only one well-tolerated dose of memantine (0.16mg/kg), which is a standard dose according to the Austrian Summary of Products Characteristics, but may be much too low to affect prolactin or cortisol concentrations, because there is evidence that high-dose memantine (20mg/kg) increases at least cortisol levels in rats (Zhou et al. 1998). Second, it is possible that the release of both hormones is triggered by a sympathomimetic effect of ketamine, because only ketamine affected cardiovascular parameters (Figure 2), and epinephrine and exercise are both well known stimuli for hormone release (Willems et al. 2000; Deuster et al. 2000). Third, memantine and ketamine have different effects on dopamine (Smith et al. 1998; Bregonzio et al. 1998; Puri et al. 1981) release, which controls prolactin release. Finally, ketamine infusion could also release prolactin by a direct effect on prolactin secreting cells (Wickings and Nieschlag 1980).
In conclusion, ketamine, in contrast to low dose memantine (0.16mg/kg), elevates serum prolactin and cortisol levels in healthy men.
References
Abi-Saab WM, D'Souza DC, Moghaddam B, Krystal JH . (1998): The NMDA antagonist model for schizophrenia: promise and pitfalls. Pharmacopsychiatry 31(Suppl 2)104–109
Arslan M, Pohl CR, Smith MS, Plant TM . (1992): Studies of the role of the N-methyl-D-aspartate (NMDA) receptor in the hypothalamic control of prolactin secretion. Life Sci 50: 295–300
Bhat GK, Mahesh VB, Chu ZW, Chorich LP, Zamorano PL, Brann DW . (1995): Localization of the N-methyl-D-aspartate R1 receptor subunit in specific anterior pituitary hormone cell types of the female rat. Neuroendocrinology 62: 178–186
Bregonzio C, Navarro CE, Donoso AO . (1998): NMDA receptor antagonists block stress-induced prolactin release in female rats at estrus. Eur J Pharmacol 350: 259–265
Danysz W, Parsons CG . (1998): Glycine and N-methyl-D-aspartate receptors: Physiological significance and possible therapeutic applications. Pharmacologic Rev 50: 597–664
Deuster PA, Petrides JS, Singh A, Chrousos GP, Poth M . (2000): Endocrine response to high-intensity exercise: dose-dependent effects of dexamethasone. J Clin Endocrinol Metab 85: 1066–1073
Jezova D, Oliver C, Jurcovicova J . (1991): Stimulation of adrenocorticotropin but not prolactin and catecholamine release by N-methyl-aspartic acid. Neuroendocrinology 54: 488–492
Jilma B, Eichler HG, Vondrovec B, Breiteneder H, Kyrle PA, Kitzweger E, Kapiotis S, Speiser W . (1996): Effects of desmopressin on circulating P-selectin. Br J Haematol 93: 432–436
Krystal JH, Karper LP, Seibyl J, Freeman GK, Delaney R, Bremner JD, et al. (1994): Subanesthetic effects of the noncompetitive NMDA antagonist, ketamine, in humans. Psychotomimetic, perceptual, cognitive, and neuroendocrine responses. Arch Gen Psychiatry 51: 199–214
Krystal JH, D'Souza DC, Karper LP, Bennett A, Abi-Dargham A, Abi-Saab D, Cassello K, Bowers MB Jr, Vegso S, Heninger GR, Charney DS . (1999): Interactive effects of subanesthetic ketamine and haloperidol in healthy humans. Psychopharmacology (Berl) 145: 193–204
Mealing GA, Lanthorn TH, Murray CL, Small DL, Morley P . (1999): Differences in degree of trapping of low-affinity uncompetitive N-methyl-D-aspartic acid receptor antagonists with similar kinetics of block. J Pharmacol Exp Ther 288: (1): 204–210
Miyatake A, Morimoto Y, Oishi T, Hanasaki N, Sugita Y, Iijima S, et al. (1980): Circadian rhythm of serum testosterone and its relation to sleep: comparison with the variation in serum luteinizing hormone, prolactin and cortisol in normal men. J Clin Endocrinol Metab 51: 1365–1371
Newcomer JW, Farber NB, Jevtovic-Todorovic V, Selke G, Melson AK, Hershey T, Craft S, Olney JW . (1999): Ketamine-induced NMDA receptor hypofunction as a model of memory impairment and psychosis. Neuropsychopharmacology 20: 106–118
Puri CP, Puri V, Anand Kumar TC . (1981): Serum levels of testosterone, cortisol, prolactin and bioactive luteinizing hormone in adult male rhesus monkeys following cage-restraint or anaesthetizing with ketamine hydrochloride. Acta Endocrinol Copenh 97: 118–124
Smith GS, Schloesser R, Brodie JD, Dewey SL, Vitkun SA, Simkowitz P, Hurley A, Coper T, Volkow ND, Cancro R . (1998): Glutamate modulation of dopamine measured in vivo with positron emission tomography (PET) and 11C-raclopride in normal human subjects. Neuropsychopharmacology 18: 18–25
Wickings EJ, Nieschlag E . (1980): Pituitary response to LRH and TRH stimulation and peripheral steroid hormones in conscious and anesthetized adult male rhesus monkeys (Macaca mulatta). Acta Endocrinol Copenh 93: 287–293
Willems E, Knigge U, Jorgensen H, Kjaer A, Warberg J . (2000): Effect of blockade of postsynaptic H1 or H2 receptors or activation of presynaptic H3 receptors on catecholamine-induced stimulation of ACTH and prolactin secretion. Eur J Endocrinol 142: 637–641
Zhou Y, Yuferov VP, Spangler R, Maggos CE, Ho A, Kreek MJ . (1998): Effects of memantine alone and with acute ‘binge’ cocaine on hypothalamic-pituitary-adrenal activity in the rat. Eur J Pharmacol 352: 65–71
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Hergovich, N., Singer, E., Agneter, E. et al. Comparison of the Effects of Ketamine and Memantine on Prolactin and Cortisol Release in Men: A Randomized, Double-blind, Placebo-controlled Trial. Neuropsychopharmacol 24, 590–593 (2001). https://doi.org/10.1016/S0893-133X(00)00194-9
Received:
Revised:
Accepted:
Issue Date:
DOI: https://doi.org/10.1016/S0893-133X(00)00194-9
Keywords
This article is cited by
-
Effects of adding low-dose ketamine to etomidate on serum cortisol levels in critically ill cardiac patients: a randomized clinical trial
BMC Anesthesiology (2022)
-
Steroid hormone secretion after stimulation of mineralocorticoid and NMDA receptors and cardiovascular risk in patients with depression
Translational Psychiatry (2020)
-
Levels of plasma and fecal glucocorticoid metabolites following an ACTH challenge in male and female coyotes (Canis latrans)
Journal of Comparative Physiology B (2018)
-
Social setting, social rank and HPA axis response in cynomolgus monkeys
Psychopharmacology (2017)
-
Memantine Effects On Sensorimotor Gating and Mismatch Negativity in Patients with Chronic Psychosis
Neuropsychopharmacology (2016)