Abstract
Background and aim
Emergency Department (ED) renal point-of-care ultrasound (PoCUS) in renal colic by accredited specialists has good prognostic value. This may not be generalizable to under-resourced EDs. We investigated PoCUS in renal colic in our ED with lesser training.
Methods
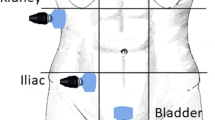
We performed a single-centre health records review of adult ED patients with renal colic and PoCUS. Patients were managed by a non-ED specialist/resident doctor with no POCUS accreditation in consultation with an attending. These doctors attended a 3.5-h training session conducted by accredited attendings to examine hydronephrosis. They needed to verify their PoCUS findings with an attending during the first two weeks of their six-month posting before performing it independently. The primary outcome was 30-day urological procedures in hydronephrotic vs. non-hydronephrotic groups. Secondary outcomes were the distribution of primary outcome with grades of hydronephrosis, 30-day ED nephrolithiasis-related reattendances in hydronephrotic vs. non-hydronephrotic groups and its distribution with grades of hydronephrosis. We compared outcomes using Fisher’s exact test. We also reported crude odds ratio (COR) and 95% CI of primary outcome between hydronephrotic vs. non-hydronephrotic groups. p values ≤ 0.05 were significant.
Results
We recruited 651 patients; 160 (24.6%) without and 491 (75.4%) with hydronephrosis. Rates of grades of hydronephrosis were: mild (76.6%), moderate (13.8%), severe (1.2%) and undifferentiated (8.4%). There was a difference in 30-day urological procedures (rates [95% CI]) in hydronephrotic vs. non-hydronephrotic groups, 11.2 [8.7–14.0]% vs. 2.5 [1.0–6.3]%; p < 0.001; COR (95% CI) 4.9 (1.8–13.8); p = 0.002. Increasing 30-day urological procedural rates were associated with increasing grade of hydronephrosis [no: 2.5%, mild: 7.7%, moderate: 23.5%, severe: 67.0% and undifferentiated: 14.6%; p < 0.001]. No differences occurred in other secondary outcomes.
Conclusions
Renal PoCUS could be performed by non-ED specialist/resident doctors to identify patients without hydronephrosis who rarely required urological intervention. Hydronephrotic patients could benefit from further risk stratification.
Abstrait
Contexte et objectif
L’échographie rénale au point de soin (PoCUS) dans les coliques rénales par des spécialistes agréés a une bonne valeur pronostique. Cela peut ne pas être généralisable aux SU sous-financés. Nous avons étudié PoCUS dans les coliques rénales dans notre DE avec une formation moindre.
Méthodes
Nous avons effectué un examen des dossiers médicaux d’un seul centre des patients adultes atteints de coliques rénales et de PoCUS. Les patients étaient pris en charge par un médecin résident/spécialiste non-membre de la DG sans accréditation POCUS en consultation avec un médecin traitant. Ces médecins ont assisté à une séance de formation de 3,5 heures menée par des titulaires accrédités pour examiner l’hydronéphrose. Ils devaient vérifier leurs résultats PoCUS auprès d’un assistant pendant les deux premières semaines de leur affectation de six mois avant de l’effectuer de manière indépendante. Le critère de jugement principal était des procédures urologiques de 30 jours dans les groupes hydronéphrotiques vs non-hydronephrotiques. Les critères de jugement secondaires étaient la distribution du critère de jugement primaire avec les grades d’hydronéphrose, les reattendances liées à la néphrose ED de 30 jours dans les groupes hydronéphrotiques vs non hydronéphrotiques et sa distribution avec les grades d’hydronéphrose. Nous avons comparé les résultats en utilisant le test exact de Fisher. Nous avons également signalé un rapport de cotes brut (RC) et un IC à 95 % du critère de jugement principal entre les groupes hydronéphrotiques et non hydronéphrotiques. Les valeurs de P 0,05 étaient significatives.
Résultats
Nous avons recruté 651 patients; 160 (24,6%) sans et 491 (75,4%) avec hydronéphrose. Les taux d’hydronéphrose étaient les suivants : légère (76,6 %), modérée (13,8 %), sévère (1,2 %) et indifférenciée (8,4 %). Il y avait une différence dans les interventions urologiques de 30 jours (taux [IC à 95 %]) dans les groupes hydronéphrotiques par rapport aux groupes non-hydronephrotiques, 11,2 [8,7-14,0] % contre 2,5 [1,0-6,3]%; p < 0,001; RCC (IC à 95 %) 4,9 (1,8-13,8); p = 0,002. L’augmentation des taux de procédures urologiques de 30 jours était associée à l’augmentation du grade d’hydronéphrose [non : 2,5%, léger : 7,7%, modéré : 23,5%, sévère : 67,0% et indifférencié : 14,6%; p < 0,001]. Aucune différence n’est survenue dans les autres critères de jugement secondaires.
Conclusions
La PoCUS rénale pourrait être réalisée par des médecins non spécialistes/résidents de la D pour identifier les patients sans hydronéphrose qui ont rarement nécessité une intervention urologique. Les patients hydronéphrotiques pourraient bénéficier d’une meilleure stratification des risques.
Similar content being viewed by others
Data availability
The data that support the findings of this study are available from the corresponding author, W.F.Lee, upon reasonable request.
References
Patti L, Leslie SW. Acute renal colic. 2022 Nov 28. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan– PMID: 28613743 (Accessed 4 July 2022).
Coursey CA, Casalino DD, Remer EM, Arellano RS, Bishoff JT, Dighe M, et al. ACR appropriateness criteria® acute onset flank pain–suspicion of stone disease. Ultrasound Q. 2012;28:227–33.
Thompson RJ, Wojcik SM, Grant WD, Ko PY. Incidental findings on CT scans in the emergency department. Emerg Med Int. 2011;2011: 624847. https://doi.org/10.1155/2011/624847.
Rekant EM, Gibert CL, Counselman FL. Emergency department time for evaluation of patients discharged with a diagnosis of renal colic: unenhanced helical computed tomography versus intravenous urography. J Emerg Med. 2001;21:371–4.
Gaspari RJ, Horst K. Emergency ultrasound and urinalysis in the evaluation of flank pain. Acad Emerg Med. 2005;12:1180–4.
Wong C, Teitge B, Ross M, Young P, Robertson HL, Lang E. The accuracy and prognostic value of point-of-care ultrasound for nephrolithiasis in the Emergency Department: a systematic review and meta-analysis. Acad Emerg Med. 2018;25:684–98.
Fields JM, Fischer JI, Anderson KL, Mangili A, Panebianco NL, Dean AJ. The ability of renal ultrasound and ureteral jet evaluation to predict 30-day outcomes in patients with suspected nephrolithiasis. Am J Emerg Med. 2015;33:1402–6.
Daniels B, Gross CP, Molinaro A, Singh D, Luty S, Jessey R, et al. Stone plus: evaluation of emergency department patients with suspected renal colic, using a clinical prediction tool combined with point-of-care limited ultrasonography. Ann Emerg Med. 2016;67:439–48.
Taylor M, Woo MY, Pageau P, McInnes MD, Watterson J, Thompson J, et al. Ultrasonography for the prediction of urological surgical intervention in patients with renal colic. Emerg Med J. 2016;33:118–23.
Mehta RL, Kellum JA, Shah SV, Molitoris BA, Ronco C, Warnock DG, et al. Acute kidney injury network: report of an initiative to improve outcomes in acute kidney injury. Crit Care. 2007. https://doi.org/10.1186/cc5713.
Acknowledgements
We received no funding for this research work. We wish to thank the staff from our Medical Informatics Department who provided much-needed assistance for us to access our patients’ electronic records. We are grateful to the research program of our Emergency Department for providing their expertise in this work. The first author has also received one year of fellowship training in Sunnybrook Health Sciences Centre and is greatly thankful for the training received which has been taught to our non-ED specialist/resident doctors.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors have no potential conflicts of interest to disclose.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Lee, W.F., Goh, S.J., Lee, B. et al. Renal point-of-care ultrasound performed by ED staff with limited training and 30-day outcomes in patients with renal colic. Can J Emerg Med 26, 198–203 (2024). https://doi.org/10.1007/s43678-023-00645-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s43678-023-00645-5