Abstract
Purpose
Intrathecal baclofen (ITB) is a well-known treatment option for cerebral palsy (CP) spasticity. The combination of soft-tissue release and ITB for spasticity is common. This study compared patients who had soft-tissue release before ITB (PRE-ITB), soft-tissue release at the same time as ITB (ST-ITB), and no ITB (NON-ITB) but had soft-tissue release at a similar age as PRE-ITB.
Methods
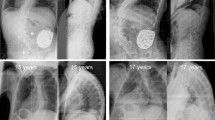
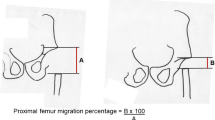
Inclusion criteria were a spastic or mixed nonambulatory CP diagnosis, prior hip adductor surgery, no prior reconstructive surgery, and at least a five-year post-operative follow-up. Thirty hips were identified as PRE-ITB, 20 hips as ST-ITB, and 43 hips as NON-ITB. The primary outcome variables were the subsequent hip surgery during the study period and/or a migration percentage ≥ 50% at the final follow-up defined as “unsuccessful hip.”
Results
The mean follow-up duration was 9.0 years (SD 2.4) for PRE-ITB, 9.4 (SD 3.6) for ST-ITB, and 9.3 (SD 3) for NON-ITB. The odds of unsuccessful outcomes were not different between NON-ITB and PRE-ITB but were lower for the ST-ITB group. The need for subsequent osteotomies or revision adductor surgery was significantly higher in ST-ITB compared with PRE-ITB (p = 0.02) or NON-ITB (p = 0.015). The incidence of surgical site infection over the whole follow-up period was higher in ST-ITB (40%) compared with PRE-ITB (13.3%, p = 0.035) and NON-ITB (0, p < 0.001).
Conclusion
The addition of tone management with ITB did not reduce the need for later hip surgery but did increase the risk for surgical site infection.



Similar content being viewed by others
References
Soo, B., Howard, J. J., Boyd, R. N., Reid, S. M., Lanigan, A., Wolfe, R., Reddihough, D., & Graham, H. K. (2006). Hip displacement in cerebral palsy. Journal of Bone Joint Surgery American, 2006(88), 121–129.
Hägglund, G., Lauge-Pedersen, H., & Wagner, P. (2007). Characteristics of children with hip displacement in cerebral palsy. BMC Musculoskeletal Disorders, 8, 101.
Terjesen, T. (2012). The natural history of hip development in cerebral palsy. Developmental Medicine & Child Neurology, 2012(54), 951–957.
Hosseinzadeh, P., Baldwin, K., Minaie, A., & Miller, F. (2020). Management of hip disorders in patients with cerebral palsy. JBJS Reviews, 8, e0148.
Lins, L. A. B., Watkins, C. J., & Shore, B. J. (2019). Natural history of spastic hip disease. Journal of Pediatric Orthopedics, 2019(39), S33–S37.
Shore, B. J., Yu, X., Desai, S., Selber, P., Wolfe, R., & Graham, H. K. (2012). Adductor surgery to prevent hip displacement in children with cerebral palsy: The predictive role of the gross motor function classification system. Journal of Bone Joint Surgery American, 94, 326–334.
Munger, M. E., Aldahondo, N., Krach, L. E., Novacheck, T. F., & Schwartz, M. H. (2017). Long-term outcomes after selective dorsal rhizotomy: A retrospective matched cohort study. Developmental Medicine and Child Neurology, 2017(59), 1196–1203.
Tedroff, K., Löwing, K., Jacobson, D. N., & Astrom, E. (2017). Does loss of spasticity matter? A 10-year follow-up after selective dorsal rhizotomy in cerebral palsy. Developmental Medicine and Child Neurology, 2011(53), 724–729.
Moreau, M., Cook, P. C., & Ashton, B. (1995). Adductor and psoas release for subluxation of the hip in children with spastic cerebral palsy. Journal of Pediatric Orthopedics, 15, 672–676.
Onimus, M., Allamel, G., Manzone, P., & Laurain, J. M. (1991). Prevention of hip dislocation in cerebral palsy by early psoas and adductors tenotomies. Journal of Pediatric Orthopedics, 11, 432–435.
Miller, F., Cardoso Dias, R., Dabney, K. W., Lipton, G. E., & Triana, M. (1997). Soft-tissue release for spastic hip subluxation in cerebral palsy. Journal of Pediatric Orthopedics, 17, 571–584.
Kalen, V., & Bleck, E. E. (1985). Prevention of spastic paralytic dislocation of the hip. Developmental Medicine and Child Neurology, 1985(27), 17–24.
Terjesen, T., Lie, G. D., Hyldmo, A. A., & Knaus, A. (2005). Adductor tenotomy in spastic cerebral palsy: A long-term follow-up study of 78 patients. Acta Orthopaedica, 76, 128–137.
Turker, R. J., & Lee, R. (2000). Adductor tenotomies in children with quadriplegic cerebral palsy: longer term follow-up. Journal of Pediatric Orthopedics, 20, 370–374.
Terjesen, T. (2017). To what extent can soft-tissue releases improve hip displacement in cerebral palsy? Acta Orthopaedica, 2017(88), 695–700.
Terjesen, T. (2006). Development of the hip joints in unoperated children with cerebral palsy: A radiographic study of 76 patients. Acta Orthopaedica, 2006(77), 125–131.
Clearfield, J. S., Nelson, M. E., McGuire, J., Rein, L. E., & Tarima, S. (2016). Intrathecal baclofen dosing regimens: A retrospective chart review. Neuromodulation, 2016(19), 642–649.
Cumlivski, R., Redl, G., Strobl, W., Krebs, A., & Machowetz, P. (2009). Neuromodulation of spasticity in children by intrathecal baclofen. Schmerz, 2009(23), 592–599.
Miller, F. (2011). The effects of continuous intrathecal baclofen infusion in non-ambulant children with cerebral palsy. Developmental Medicine and Child Neurology, 2011(53), 679–680.
Boster, A. L., Adair, R. L., Gooch, J. L., Nelson, M. E. S., Toomer, A., Urquidez, J., & Saulino, M. (2016). Best practices for intrathecal baclofen therapy: Dosing and long-term management. Neuromodulation, 2016(19), 623–631.
Buizer, A. I., Martens, B. H. M., van Grandbois, R. C., Schoonmade, L. J., Becher, J. G., & Vermeulen, R. J. (2019). Effect of continuous intrathecal baclofen therapy in children: a systematic review. Developmental Medicine & Child Neurology, 61, 128–134.
Reimers, J. (1980). The stability of the hip in children: A radiological study of the results of muscle surgery in cerebral palsy. Acta Orthopaedica Scandinavica Suppl, 184, 1–100.
Borowski, A., Shah, S. A., Littleton, A. G., Dabney, K. W., & Miller, F. (2008). Baclofen pump implantation and spinal fusion in children: techniques and complications. Spine (Phila Pa 1976), 33, 1995–2000.
Bouwhuis, C. B., van der Heijden-Maessen, H. C., Boldingh, E. J., Bos, C. F. A., & Lankhorst, G. J. (2015). Effectiveness of preventive and corrective surgical intervention on hip disorders in severe cerebral palsy: A systematic review. Disability & Rehabilitation, 37, 97–105.
Miller, S. D., Juricic, M., Hesketh, K., Mclean, L., Magnuson, S., Gasior, S., Schaeffer, E., O’donnell, M., & Mulpuri, K. (2017). Prevention of hip displacement in children with cerebral palsy: A systematic review. Developmental Medicine & Child Neurology, 59, 1130–1138.
Novak, I., Morgan, C., Fahey, M., Finch-Edmondson, M., Galea, C., Hines, A., Langdon, K., Mc Namara, M., Paton, M. C., Popat, H., Shore, B., Khamis, A., Stanton, E., Finemore, O. P., Tricks, A., Tevelde, A., Dark, L., Morton, N., & Badawi, N. (2020). State of the evidence traffic lights 2019: systematic review of interventions for preventing and treating children with cerebral palsy. Current Neurology & Neuroscience Reports, 20, 3.
Gerszten, P. C., Albright, A. L., & Johnstone, G. F. (1998). Intrathecal baclofen infusion and subsequent orthopedic surgery in patients with spastic cerebral palsy. Journal of Neurosurgery, 1998(88), 1009–1013.
Gooch, J. L., McFadden, M., & Oberg, W. (2013). Orthopedic surgery in children with intrathecal baclofen pumps. Journal of Pediatric Rehabilitation Medicine, 6, 233–238.
Imerci, A., Rogers, K. J., Pargas, C., Sees, J. P., & Miller, F. (2019). Identification of complications in paediatric cerebral palsy treated with intrathecal baclofen pump: a descriptive analysis of 15 years at one institution. Journal of Children’s Orthopaedics, 13, 529–535.
Hägglund, G., Alriksson-Schmidt, A., Lauge-Pedersen, H., Rodby-Bousquet, E., Wagner, P., & Westbom, L. (2014). Prevention of dislocation of the hip in children with cerebral palsy: 20-year results of a population-based prevention programme. Bone Joint Journal, 96-B, 1546–1552.
Presedo, A., Oh, C. W., Dabney, K. W., & Miller, F. (2005). Soft-tissue releases to treat spastic hip subluxation in children with cerebral palsy. Journal of Bone and Joint Surgery. American Volume, 2005(87), 832–841.
Vidal, J., Deguillaume, P., & Vidal, M. (1985). The anatomy of the dysplastic hip in cerebral palsy related to prognosis and treatment. International Orthopaedics, 9, 105–110.
Funding
The authors declare that no funds, grants, or other support were received during the preparation of this manuscript.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study’s conception and design. Material preparation, data collection and analysis were performed by AA, ACU, JJ H, KJR, FM, and MWS. The first draft of the manuscript was written by AA, ACU, JJH, and KJR. Critical revision for important intellectual content was made by AA, ACU, JJH, KJR, FM, and MWS. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
Ali Asma, Armagan Can Ulusaloglu, Jason J. Howard, Kenneth J. Rogers, Freeman Miller, and Michael Wade Shrader declare that they have no conflict of interest.
Ethical approval
This study was performed in line with the principles of the Declaration of Helsinki. Approval was granted by the Nemours Office of Human Subjects Protection Institutional Review Board.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Asma, A., Ulusaloglu, A.C., Howard, J.J. et al. Does the Addition of Intrathecal Baclofen Along with or After Soft-Tissue Hip Adductor Surgery Decrease the Need for Hip Reconstruction Compared with Soft-Tissue Surgery Alone for Children with Nonambulatory Cerebral Palsy?. JOIO 56, 2176–2181 (2022). https://doi.org/10.1007/s43465-022-00762-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s43465-022-00762-w