Abstract
Adverse drug reactions (ADRs) are estimated to be between the fourth and sixth most common cause of death worldwide, taking their place among other prevalent causes of mortality such as heart disease, cancer, and stroke. ADRs impact a broad range of populations across a wide variety of global geography and demographics, with significant mortality and morbidity burden in vulnerable groups such as older people, pediatric populations, and individuals in low-income settings. Too large a share of medicines risk management remains limited to signal detection in big ADR databases (USFDA, EMA, WHO, etc.) This resource allocation is antiquated and applied statistical signal detection methodologies have reached their limits of usefulness. In addition, existing databases are designed for short-term reactions, closely related to medication use and, thus, can only partially assess important broader consequences across geography, time, and clinical relevance. There is an urgent need change the dynamic. We need to identify (earlier and more regularly) many of the important but often overlooked or missed ADRs. Rather than assigning blame, we need to identify the root causes of the problem so they can be clearly addressed and fixed. The public health implications are profound—particularly as we recognize the importance of predicting and mitigating the next pandemic. Consequently, medicines risk management must be integrated within a broader global public health vision. To accomplish this, we need to develop the new tools and methodologies critical to assessing these public health imperatives.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction: A Global Issue
Adverse drug reactions (ADRs) are estimated to be between the fourth and sixth most common cause of death worldwide, taking their place among other prevalent causes of mortality such as heart disease, cancer, and stroke [1, 2]. ADRs impact a broad range of populations across a wide variety of global geography and demographics, with significant mortality and morbidity burden in vulnerable groups, such as older people, pediatric populations, and individuals in low-income settings [3].
As we have previously argued, in a world increasingly driven by outcomes reporting and Big Data, more patient-level information from individual consumers is not always synonymous with validated data. Despite the frustrating increase in the signals-to-noise ratio, artificial intelligence is becoming an ever-more significant source of potentially valuable electronically generated health care information [4]. Self-reporting must be encouraged throughout the pharmacovigilance spectrum as well as a concerted effort to optimize current reporting tools. However, that is not enough.
Some have argued that various abbreviated review pathways have led to more and more serious ADRs [5], but we disagree. Safety events were significantly less common among drugs with the shortest regulatory review times [6]. There are no easy answers.
The Cost of the Problem
ADR-related healthcare costs are significant—and preventable. In the United States and Europe, the financial burden is estimated at $30.1 billion US dollars and €79 billion euros, respectively [7, 8]. Despite improved access to medicines, the data on the impact of ADRs in low-and middle-income countries is scarce and very likely underestimated. A contextualized assessment of the global burden of ADRs in terms of both patients, economics, and the broader public health paradigm is a priority for the World Health Organization (WHO). The burden of ADRs has been further accentuated due to the COVID-19 pandemic, as any drug safety issue can be a contributing risk factor for vaccine hesitancy [9].
As Kjoersvik and Bate argue, effective identification of previously implausible safety signals is a core component of successful pharmacovigilance. Timely, reliable, and efficient data ingestion and related processing are critical to this. The term ‘black swan events’ was coined by Taleb to describe events with three attributes: unpredictability, severe, and widespread consequences, and retrospective bias. These rare events are not well understood at their emergence but are often rationalized in retrospect as predictable. Pharmacovigilance strives to rapidly respond to potential black swan events associated with medicine or vaccine use [10].
Although ADRs can never be entirely eliminated (due to unavoidable idiosyncratic events or those events of low predictivity, such as bone marrow suppression) they can be significantly mitigated, reducing both financial costs, and human suffering.
Current Strategies and Tactics
Following the European thalidomide tragedy [11], the WHO created the Program for International Drug Monitoring (WHO PIDM) in 1968 [12]. Currently more than 170 countries are members. The goal of the WHO PIDMs is to detect signals of any potential harm related to drug usage by gathering all available information and making it publicly available through a global drug monitoring database. The system is based on the signals detected through the assessment of spontaneous notifications of suspected ADRs. Moving forward, the WHO PIDM, the program should not only be restricted to monitor, but also consider developing a context-specific drug risk management program. In a parallel development, high-income countries created their own national (i.e., USFDA) and regional (i.e., EMA) risk management systems based on regulatory sciences and dedicated resources. The role these systems is to provide recommendations for all stakeholders, regulatory, reimbursement, industry, academia, and provider on all aspects of the drug/biologic lifecycle.
To continuously advance the global harmonization of medicines regulation, the International Council for Harmonization of Technical Requirements for Pharmaceuticals for Human Use (ICH) [13] has, since 1990, issued many guidance documents on optimizing pharmacovigilance systems. In 2001, the European Union (EU) established the first regional pharmacovigilance system implementing a set of evolving measures which included the EudraVigilance database [14] for the management, collection, and analysis of suspected ADRs (among other measures) of medicines authorized within the European Union.
EudraVigilance and other measures to advance pharmacovigilance: (“the science and activities relating to the detection, assessment, understanding and prevention of adverse effects or any other medicine-related problems” [15]) exist not only as regulatory concepts, but as legally binding, evolving, and actionable public health practices, within the broader regulatory concept of drug risk management.
Even with these transnationally coordinated and technologically sophisticated efforts, the results are not particularly impressive. Moving forwards, we must consider ways to more fully maximize the institutional knowledge and resources (both human and financial) of the biopharmaceutical industry, and regulatory agencies, as well as the experiences of both healthcare providers and patients.
Thinking Beyond the Status Quo
Pharmacovigilance policies and practices evolve through the continuous assessment of benefit-risk ratios of medicines in the post-marketing setting, through signal detection and assessment, prevention, and interventions such as prophylactic risk mitigation tools (such as the USAFDA’s REMS programs [16]) and pharmacoepidemiologic studies. Pharmacovigilance systems aim collect, analyze, and share and promote access of safe and effective medicines,—even if the facts sometime diverge from national public health interests in low- and middle-income countries [17].
As an example, the implementation of any given intervention designed for the reduction of medication harm specific to Europe or the United States, may not be as easily adapted in lower- and middle-income countries due to different political, economic, and public health priorities. This can be clearly seen in the utilization of pre-prescription genotype-screening for the prevention of drug-induced severe cutaneous adverse drug reactions (SCARS) which is neither feasible nor affordable everywhere.
Similarly, probability scales, developed to help standardize assessment of causality for all adverse drug reactions [18] are one way to assign ADR predictability scores, but such tools still require advanced (and robust) collection capabilities. As Liang, et al. point out, the quantity and quality of data directly affect the performance of AI, and there are particular challenges to implementing AI in limited-resource settings [19].
As we have argued previously, the widely variable ability of nations to build reliable regulatory systems (from precise review to robust pharmacovigilance) is a dangerous source of health care inequality [20].
Williams, et al. [21] have argued that using iterative pairwise external validation to contextualize prediction model performance, but the lack of interoperability of healthcare databases has been the biggest barrier to this occurring on a large scale.
Developing validated tools and techniques for “predictive pharmacovigilance” will assist all health systems in better understanding the risks and benefits of the medicines they regulate by understanding what should be happening once a new medicine moves from risk–benefit regulatory efficacy to real-world risk-effectiveness. This will be of particular utility for smaller regulatory agencies with fewer resources. By comparing preapproval predictive pharmacovigilance data, developing regulatory authorities will be able to better understand the potential gap between what was predicted and what was actually measured (via more traditional pharmacovigilance methodologies). Predictive pharmacovigilance recognizes the value of understanding the imperfect reporting of real-world clinical use and that the absence of reporting is an important post-marketing signal [20].
Global Challenges and Opportunities
Currently, national, regional, and global systems are confronting several daunting challenges.
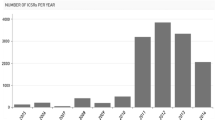
Today, generally accepted pharmacovigilance “best” practice is largely focused on promoting spontaneous notification to enhance relevant signal detection. Consequently, the number of case reports increases steadily, requiring development of the statistical tools to identify potential “signals” from the broader “noise” and, as a result, the majority of pharmacovigilance activities rely more on statistical screening rather than comprehensive clinical assessment.
Statistical detection of signals in huge national, regional, and global databases depends on the magnitude of disproportionality of an association [22], which is based on the number of case reports of interest and those used as reference. For example, a clinical event, like hepatitis, is more often observed with the drug of interest than compared with all other available drugs in a database. However, when the number of case reports increases to exhaustivity (i.e., over several hundred thousand case reports), even a small difference become statistically significant and could generate false-positive signals. In the same way, a high number of reported side effects with the same drug in a short period of time, such as the COVID-19 vaccine roll-out, can mask signals associated with other drugs or combination of drugs. In the short term, these statistical challenges can be handled through modifications of current algorithms based on disproportionality, but there is a strong need for innovative statistical approaches and the integration of both machine learning and artificial intelligence [23] New challenges require new and better solutions.
Spontaneous case reports refer mainly to easily recognized side effects occurring in a short time frame and to a limited number of patients (for example anaphylactic reactions related antibiotic use), while delayed and less easily recognized clinical side effects of significant public health impact may not be identified at all. A good example of this phenomenon is dementia related to benzodiazepine use [24]. Public health concerns related to medicines may stem not only from unsuspected associations that affect a small number of cases, but from associations related to drugs, which can increase the occurrence of common outcomes. Thus, the current systems need to be improved to identify drug-related side effects of wider public health concern.
In order to consider the wider impact of medications in various areas (including society and economics), a novel paradigm of drug risk management relating directly to public health is needed. For such purpose, the definition of Global Public Health may be useful: “Global health emphasis transnational health issues, determinants, and solutions; involves many disciplines within and beyond the health sciences and promotes interdisciplinary collaboration; and is a synthesis of population-based prevention with individual-level clinical care.” [25] Global Public Health needs to encompass medicines risk management strategies and tactics as part of a more inclusive interdisciplinary approach. Tools, such as indicators for assessing the global impact of identified and validated side effects within a more defined parameters (nation, region, etc.) identified side effects settings of and the new methodologies identifying drug associated public health issues need to be developed. It also requires policy experts and government officials to leave their comfort zones. Alas, the status quo is a harsh mistress.
Conclusion: We Must Transcend the Status Quo
Too large a share of medicines risk management remains limited to signal detection in big ADR databases (USFDA, EMA, WHO, etc.) This resource allocation is antiquated and applied statistical signal detection methodologies have reached their limits of usefulness. In addition, the existing databases are designed for short-term reactions, closely related to medication use and, thus, can only partially assess important broader consequences across geography, time, and clinical relevance.
There is an urgent need to change the dynamic. We need to identify (earlier and more regularly) many of the important but often overlooked or missed ADRs. The public health implications are profound—particularly as we recognize the importance of predicting and mitigating the next pandemic. Consequently, medicines risk management must be integrated within a broader global public health vision. To accomplish this, we need to develop the new tools and methodologies critical to assessing these public health imperatives.
References
Bates DW. Drugs and adverse drug reactions: how worried should we be? JAMA. 1998;279(15):1216–7.
Bonn D. Adverse drug reactions remain a major cause of death. Lancet. 1998;351(9110):1183.
Brahma DK, Wahlang JB, Marak MD, Sangma M. Adverse drug reactions in the elderly. J Pharmacol Pharmacother. 2013;4(2):91–4.
Pitts PJ, Le Louet H, Katz G. 21st-century oncology drug safety via new-age regulatory standards and practices. Ther Innov Regul Sci. 2019;53:701–5. https://doi.org/10.1177/2168479018809689.
https://www.sciencedaily.com/releases/2017/05/170509121927.htm.
Sultana J, Cutroneo P, Trifiro G. Clinical and economic burden of adverse drug reactions. J Pharmacol Pharmacother. 2013;4(Suppl1):S73–7.
Commission of the European Communities. Commission staff working document Annex 2 of the Report on the impact assessment of strengthening and rationalizing EU Pharmacovigilance. 2008.
https://www.commercialbiotechnology.com/index.php/jcb/article/view/1012.
Kjoersvik O, Bate A. Black swan events and intelligent automation for routine safety surveillance. Drug Saf. 2022;45:419–27. https://doi.org/10.1007/s40264-022-01169-0.
Toxicol Sci. 2011;122(1):1–6. https://doi.org/10.1093/toxsci/kfr088.
https://who-umc.org/about-the-who-programme-for-international-drug-monitoring/.
https://www.ema.europa.eu/en/human-regulatory/research-development/pharmacovigilance/eudravigilance.
https://www.who.int/teams/regulation-prequalification/regulation-and-safety/pharmacovigilance.
https://www.sciencedirect.com/science/article/pii/S1319016417301780.
Naranjo CA, Busto U, Sellers EM, Sandor P, Ruiz I, Roberts EA, Janecek E, et al. A method for estimating the probability of adverse drug reactions. Clin Pharacol Ther. 1981;30:239–45.
Liang L, Hu J, Sun G, et al. Artificial intelligence-based pharmacovigilance in the setting of limited resources. Drug Saf. 2022;45:511–9. https://doi.org/10.1007/s40264-022-01170-7.
Williams RD, Reps JM, Kors JA, et al. Using iterative pairwise external validation to contextualize prediction model performance: a use case predicting 1-year heart failure risk in patients with diabetes across five data sources. Drug Saf. 2022;45:563–70. https://doi.org/10.1007/s40264-022-01161-8.
Moreland-Head LN, Coons JC, Seybert AL, Gray MP, Kane-Gill SL. Use of disproportionality analysis to identify previously unknown drug-associated causes of cardiac arrhythmias using the food and drug administration adverse event reporting system (FAERS) database. J Cardiovasc Pharmacol Ther. 2021;26(4):341–8. https://doi.org/10.1177/1074248420984082.
de Gage SB, Begaud B, Bazin F, Verdoux H, Dartigues J-F, Peres K, et al. Benzodiazepine use and risk of dementia: prospective population-based study. BMJ. 2012;27(345): e6231.
Salm M, Ali M, Minihane M, Conrad P. Defining global health: findings from a systematic review and thematic analysis of the literature. BMJ Glob Health. 2021;6(6): e005292. https://doi.org/10.1136/bmjgh-2021-005292.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
On behalf of all authors, the corresponding author states that there is no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Le Louët, H., Pitts, P.J. Twenty-First Century Global ADR Management: A Need for Clarification, Redesign, and Coordinated Action. Ther Innov Regul Sci 57, 100–103 (2023). https://doi.org/10.1007/s43441-022-00443-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s43441-022-00443-8