Abstract
Purpose
Our institution employs a multimodal approach to manage postoperative pain after spine surgery. It involves continuous intravenous (IV) lidocaine until the morning of postoperative day two. This study aimed to determine the rate and reasons for early discontinuation of IV lidocaine in our spine patients.
Methods
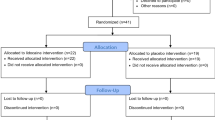
We conducted a retrospective chart review and included pediatric patients who underwent ≥ 3-level spine surgery and received postoperative IV lidocaine from November 2019 to September 2022. For each case, we recorded the side effects of IV lidocaine, adverse events, time to discontinuation, and discontinuation rate. Subsequently, we used the same methodology to generate an adult cohort for comparison.
Results
We included 52 pediatric (18M:34F) and 50 (21M:29F) adult patients. The pediatric cohort’s mean age was 14 years (8–18), and BMI 23.9 kg/m2 (13.0–42.8). The adult cohort’s mean age was 61 years (29–82), and BMI 28.8 kg/m2 (17.2–44.1). IV lidocaine was discontinued prematurely in 21/52 (40.4%) of the pediatric cases and 26/50 (52.0%) of the adult cases (RR = 0.78, p = 0.2428). The side effects noted in the pediatric cases vary, including numbness, visual disturbance, and obtundation, but no seizures. The most common adverse events were fever and motor dysfunction.
Conclusion
The early discontinuation rate of IV lidocaine use after spine surgery for children in our institution does not differ significantly from that of adults. The nature of the side effects and the reasons for discontinuation between the groups were similar. Thus, the safety profile of IV lidocaine for pediatric spine patients is comparable to adults.


Similar content being viewed by others
References
Licina A, Silvers A (2022) Perioperative intravenous lidocaine infusion for postoperative analgesia in patients undergoing surgery of the spine: systematic review and meta-analysis. Pain Med 23(1):45–56. https://doi.org/10.1093/pm/pnab210
Yoo JS, Ahn J, Buvanendran A, Singh K (2019) Multimodal analgesia in pain management after spine surgery. J Spine Surg 5(Suppl 2):S154–S159. https://doi.org/10.21037/jss.2019.05.04
Chou R, Gordon DB, de Leon-Casasola OA et al (2016) Management of postoperative pain: a clinical practice guideline from the American Pain Society, the American Society of Regional Anesthesia and Pain Medicine, and the American Society of Anesthesiologists’ Committee on Regional Anesthesia, Executive Committee, and Administrative Council [published correction appears in J Pain. 2016 Apr;17(4):508–10. Dosage error in article text]. J Pain 17(2):131–157. https://doi.org/10.1016/j.jpain.2015.12.008
Understanding the opioid overdose epidemic. Centers for Disease Control and Prevention. Updated June 1, 2022. https://www.cdc.gov/opioids/basics/epidemic.html. Accessed 17 Feb 2023
Klemme WR, Burkhalter W, Polly DW Jr, Dahl LF, Davis DA (1999) Reversible ischemic myelopathy during scoliosis surgery: a possible role for intravenous lidocaine. J Pediatr Orthop 19(6):763–765
Prabhakar NK, Chadwick AL, Nwaneshiudu C et al (2022) Management of postoperative pain in patients following spine surgery: a narrative review. Int J Gen Med 15:4535–4549. https://doi.org/10.2147/IJGM.S292698
Cassuto J, Wallin G, Högström S, Faxén A, Rimbäck G (1985) Inhibition of postoperative pain by continuous low-dose intravenous infusion of lidocaine. Anesth Analg 64(10):971–974
Baral BK, Bhattarai BK, Rahman TR, Singh SN, Regmi R (2010) Perioperative intravenous lidocaine infusion on postoperative pain relief in patients undergoing upper abdominal surgery. Nepal Med Coll J 12(4):215–220
De Oliveira Jr GS, Fitzgerald P, Streicher LF, Marcus RJ, McCarthy RJ (2012) Systemic lidocaine to improve postoperative quality of recovery after ambulatory laparoscopic surgery. Anesth Analg 115(2):262–267. https://doi.org/10.1213/ANE.0b013e318257a380
Vigneault L, Turgeon AF, Côté D et al (2011) Perioperative intravenous lidocaine infusion for postoperative pain control: a meta-analysis of randomized controlled trials. Can J Anaesth 58(1):22–37. https://doi.org/10.1007/s12630-010-9407-0
Chu R, Umukoro N, Greer T et al (2020) Intravenous lidocaine infusion for the management of early postoperative pain: a comprehensive review of controlled trials. Psychopharmacol Bull 50(4 Suppl 1):216–259
Haratian A, Musa A, Field R, Farhan S, Bennett C, Cooke C, Patel RD, Aleem IS, Eichler MC, Rajalingam K, Lee C, Bederman S (2021) Intravenous lidocaine in spine surgery: a meta-analysis of randomized controlled trials. N Am Spine Soc J. 7:100079. https://doi.org/10.1016/j.xnsj.2021.100079
Sriganesh K, Bharadwaj S, Shanthanna H, Rao GSU, Kramer BW, Sathyaprabha TN (2023) Opioid versus non-opioid analgesia for spine surgery: a systematic review and meta-analysis of randomized controlled trials. Eur Spine J 32(1):289–300. https://doi.org/10.1007/s00586-022-07469-4
Weibel S, Jelting Y, Pace NL et al (2018) Continuous intravenous perioperative lidocaine infusion for postoperative pain and recovery in adults. Cochrane Database Syst Rev 6(6):CD09642. https://doi.org/10.1002/14651858.CD009642.pub3
Rafeeqi T, Pearson EG (2021) Enhanced recovery after surgery in children. Transl Gastroenterol Hepatol 25(6):46. https://doi.org/10.21037/tgh-20-188
Phillips MR, Adamson WT, McLean SE, Hance L, Lupa MC, Pittenger SL, Dave P, McNaull PP (2020) Implementation of a pediatric enhanced recovery pathway decreases opioid utilization and shortens time to full feeding. J Pediatr Surg 55(1):101–105. https://doi.org/10.1016/j.jpedsurg.2019.09.065
Ljungqvist O, Scott M, Fearon KC (2017) Enhanced recovery after surgery: a review. JAMA Surg 152(3):292–298. https://doi.org/10.1001/jamasurg.2016.4952
Yeung SE, Hilkewich L, Gillis C, Heine JA, Fenton TR (2017) Protein intakes are associated with reduced length of stay: a comparison between enhanced recovery after surgery (ERAS) and conventional care after elective colorectal surgery. Am J Clin Nutr 106(1):44–51. https://doi.org/10.3945/ajcn.116.148619
West MA, Horwood JF, Staves S, Jones C, Goulden MR, Minford J, Lamont G, Baillie CT, Rooney PS (2013) Potential benefits of fast-track concepts in paediatric colorectal surgery. J Pediatr Surg 48(9):1924–1930. https://doi.org/10.1016/j.jpedsurg.2013.02.063
Bakan M, Umutoglu T, Topuz U et al (2015) Opioid-free total intravenous anesthesia with propofol, dexmedetomidine and lidocaine infusions for laparoscopic cholecystectomy: a prospective, randomized, double-blinded study. Braz J Anesthesiol 65(3):191–199. https://doi.org/10.1016/j.bjane.2014.05.001
Zhu B, Zhou X, Zhou Q, Wang H, Wang S, Luo K (2019) Intra-venous lidocaine to relieve neuropathic pain: a systematic review and meta-analysis. Front Neurol 10:954. https://doi.org/10.3389/fneur.2019.00954
Li X, Lv X, Jiang Z et al (2020) Application of intravenous lidocaine in obese patients undergoing painless colonoscopy: a prospective, randomized, double-blind, controlled study. Drug Des Dev Ther 14:3509–3518. https://doi.org/10.2147/DDDT.S266062
Batko I, Kościelniak-Merak B, Tomasik PJ, Kobylarz K, Wordliczek J (2020) Lidocaine as an element of multimodal analgesic therapy in major spine surgical procedures in children: a prospective, randomized, double-blind study. Pharmacol Rep 72(3):744–755. https://doi.org/10.1007/s43440-020-00100-7
Lemming K, Fang G, Buck ML (2019) Safety and tolerability of lidocaine infusions as a component of multimodal postoperative analgesia in children. J Pediatr Pharmacol Ther 24(1):34–38. https://doi.org/10.5863/1551-6776-24.1.34
Anghelescu DL, Morgan KJ, Frett MJ et al (2021) Lidocaine infusions and reduced opioid consumption-Retrospective experience in pediatric hematology and oncology patients with refractory pain. Pediatr Blood Cancer 68(11):e29215. https://doi.org/10.1002/pbc.29215
Schuler BR, Lupi KE, Szumita PM, Kovacevic MP (2021) Evaluating the safety of continuous infusion lidocaine for postoperative pain. Clin J Pain 37(9):657–663. https://doi.org/10.1097/AJP.0000000000000960
Hall EA, Sauer HE, Davis MS, Anghelescu DL (2021) Lidocaine infusions for pain management in pediatrics. Paediatr Drugs 23(4):349–359. https://doi.org/10.1007/s40272-021-00454-2
Chen M, Wu D, Chen F, Li J, Wu J, Shangguan W (2023) Intravenous lidocaine simultaneously infused with sufentanil to accelerate gastrointestinal function recovery in patients after thoracolumbar surgery: a prospective, randomized, double-blind controlled study. Eur Spine J 32(1):313–320. https://doi.org/10.1007/s00586-022-07456-9
Maheshwari K, Avitsian R, Sessler DI et al (2020) Multimodal analgesic regimen for spine surgery: a randomized placebo-controlled trial. Anesthesiology 132(5):992–1002. https://doi.org/10.1097/ALN.0000000000003143
Buren MA, Theologis A, Zuraek A, Behrends M, Clark AJ, Leung JM (2022) Lidocaine infusion for the management of postoperative pain and delirium (LIMPP): protocol for a randomised control trial. BMJ Open 12(6):e059416. https://doi.org/10.1136/bmjopen-2021-059416
Dewinter G, Moens P, Fieuws S, Vanaudenaerde B, Van de Velde M, Rex S (2017) Systemic lidocaine fails to improve postoperative morphine consumption, postoperative recovery and quality of life in patients undergoing posterior spinal arthrodesis. A double-blind, randomized, placebo-controlled trial. Br J Anaesth 118(4):576–585. https://doi.org/10.1093/bja/aex038
Farag E, Ghobrial M, Sessler DI, Dalton JE, Liu J, Lee JH, Zaky S, Benzel E, Bingaman W, Kurz A (2013) Effect of perioperative intravenous lidocaine administration on pain, opioid consumption, and quality of life after complex spine surgery. Anesthesiology 119(4):932–940. https://doi.org/10.1097/ALN.0b013e318297d4a5
Kim KT, Cho DC, Sung JK, Kim YB, Kang H, Song KS, Choi GJ (2014) Intraoperative systemic infusion of lidocaine reduces postoperative pain after lumbar surgery: a double-blinded, randomized, placebo-controlled clinical trial. Spine J 14(8):1559–1566. https://doi.org/10.1016/j.spinee.2013.09.031
Ibrahim A, Aly M, Farrag W (2018) Effect of intravenous lidocaine infusion on long-term postoperative pain after spinal fusion surgery. Medicine (Baltimore) 97(13):e0229. https://doi.org/10.1097/MD.0000000000010229
Acknowledgements
We thank Michael D. Evans, MS, for his work on the statistical analysis for this project.
Funding
The authors did not receive support from any organization for the submitted work.
Author information
Authors and Affiliations
Contributions
PBOS, JJH, JCR, GAF, DBS, KJH, DWP: Made substantial contributions to the conception and design of the work, and the acquisition, analysis, and interpretation of data. Revised the work critically for important intellectual content. Approved the version to be published and agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Corresponding authors
Ethics declarations
Conflict of interest
DP declares consulting fees from Globus Medical and Alexion; institutional grant/research support from Medtronic and Mizuho OSI; consulting fees, royalties, and honoraria from SI Bone; and royalties/other financial or material support from Springer. PS, JH, JR, GF, DS, and KH declare no financial conflicts. The authors did not receive support from any organization for the submitted work.
Ethical approval/review
This study was approved by the University of Minnesota Institutional Review Board.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Soriano, P.B.O., Haselhuhn, J.J., Resch, J.C. et al. Postoperative use and early discontinuation of intravenous lidocaine in spine patients. Spine Deform 12, 141–148 (2024). https://doi.org/10.1007/s43390-023-00753-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s43390-023-00753-3