Abstract
Background
Obesity, insulin resistance, and hyperandrogenemia are commonly seen in women with polycystic ovary syndrome (PCOS), and these three conditions form a vicious cycle leading to reproductive and metabolic abnormalities. Metformin improves the symptoms of PCOS by increasing insulin sensitivity but is not therapeutically optimal. Recent studies have reported that sodium-glucose co-transporter protein receptor inhibitors improve insulin resistance and reduce the weight of patients with PCOS. We performed a meta-analysis to assess the influence of sodium-glucose co-transporter protein-2 (SGLT2) inhibitors on anthropometric, glycolipid metabolism and reproductive outcomes after therapy of overweight/obese women with PCOS.
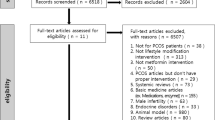
Methods
We searched the relevant literature published up to April 2023. Information on the effect of SGLT2 inhibitors on overweight/obese patients with PCOS was extracted independently by two reviewers. Review Manager 5.3 was used for meta-analysis.
Results
Five randomized controlled trials that met our criteria were retrieved. Our meta-analysis demonstrated that in overweight/obese patients with PCOS, SGLT2 inhibitors treatment was significantly superior to metformin treatment in terms of reducing body weight (P = 0.02, I2 = 36%), decreasing dehydroepiandrosterone sulfate concentrations [SMD = -0.42, 95% CI (-0.76, -0.07), I2 = 22%, P = 0.02], and reducing the incidence of nausea [RR = 0.35, 95% CI (0.21, 0.60), I2 = 71%, P = 0.0001].
Conclusions
SGLT2 inhibitors are a possible alternative therapy for treating overweight/obese women with PCOS who do not respond favorably to metformin treatment. However, further large randomized controlled trials and cost-effectiveness analyses are warranted to guide the implementation of SGLT2 inhibitors treatment in this population.








Similar content being viewed by others
Data Availability
Not applicable.
Code Availability
Not applicable.
References
Lizneva D. Criteria, prevalence, and phenotypes of polycystic ovary syndrome. Fertil Steril. 2016;106(1):6–15.
Norman RJ. Polycystic ovary syndrome. Lancet. 2007;370(9588):685–97.
Nandi A. Polycystic ovary syndrome. Endocrinol Metab Clin North Am. 2014;43(1):123–47.
Rasquin LI, Anastasopoulou C, Mayrin JV. Polycystic ovarian disease. Treasure Island: StatPearls Publishing; 2023.
Barry JA, Azizia MM, Hardiman PJ. Risk of endometrial, ovarian and breast cancer in women with polycystic ovary syndrome: a systematic review and meta-analysis. Hum Reprod Update. 2014;20(5):748–58.
Bagir GS. Body Mass Index below Obesity Threshold Implies Similar Cardiovascular Risk among Various Polycystic Ovary Syndrome Phenotypes. Med Princ Pract. 2016;25(1):61–6.
Wang FF. Pharmacologic therapy to induce weight loss in women who have obesity/overweight with polycystic ovary syndrome: a systematic review and network meta-analysis. Obes Rev. 2018;19(10):1424–45.
Stepto NK. Women with polycystic ovary syndrome have intrinsic insulin resistance on euglycaemic-hyperinsulaemic clamp. Hum Reprod. 2013;28(3):777–84.
Mahalingaiah S, Diamanti-Kandarakis E. Targets to treat metabolic syndrome in polycystic ovary syndrome. Expert Opin Ther Targets. 2015;19(11):1561–74.
Rubin KH. Development and Risk Factors of Type 2 Diabetes in a Nationwide Population of Women With Polycystic Ovary Syndrome. J Clin Endocrinol Metab. 2017;102(10):3848–57.
Li Y. Multi-system reproductive metabolic disorder: significance for the pathogenesis and therapy of polycystic ovary syndrome (PCOS). Life Sci. 2019;228:167–75.
Lashen H. Role of metformin in the management of polycystic ovary syndrome. Ther Adv Endocrinol Metab. 2010;1(3):117–28.
Teede HJ. Recommendations from the international evidence-based guideline for the assessment and management of polycystic ovary syndrome. Hum Reprod. 2018;33(9):1602–18.
Practice Committee of the American Society for Reproductive Medicine. Role of metformin for ovulation induction in infertile patients with polycystic ovary syndrome (PCOS): a guideline. Fertil Steril. 2017;108(3):426–41.
Dunaif A. Drug insight: insulin-sensitizing drugs in the treatment of polycystic ovary syndrome–a reappraisal. Nat Clin Pract Endocrinol Metab. 2008;4(5):272–83.
Chen X, He S, Wang D. Effects of metformin on body weight in polycystic ovary syndrome patients: model-based meta-analysis. Expert Rev Clin Pharmacol. 2021;14(1):121–30.
Vallon V, Verma S. Effects of SGLT2 Inhibitors on Kidney and Cardiovascular Function. Annu Rev Physiol. 2021;83:503–28.
Marinkovic-Radosevic J. Exploring new treatment options for polycystic ovary syndrome: Review of a novel antidiabetic agent SGLT2 inhibitor. World J Diabetes. 2021;12(7):932–8.
Pruett JE. 2021 Impact of SGLT-2 Inhibition on Cardiometabolic Abnormalities in a Rat Model of Polycystic Ovary Syndrome. Int J Mol Sci. 2021;22(5):2576.
Li X. Sodium Glucose Co-Transporter 2 Inhibitors Ameliorate Endothelium Barrier Dysfunction Induced by Cyclic Stretch through Inhibition of Reactive Oxygen Species. Int J Mol Sci. 2021;22(11):6044.
DeFronzo RA, Norton L, Abdul-Ghani M. Renal, metabolic and cardiovascular considerations of SGLT2 inhibition. Nat Rev Nephrol. 2017;13(1):11–26.
Rotterdam ESHRE/ASRM-Sponsored PCOS consensus workshop group. Revised 2003 consensus on diagnostic criteria and long-term health risks related to polycystic ovary syndrome (PCOS). Hum Reprod. 2004;19(1):41–7.
Legro RS. Diagnosis and treatment of polycystic ovary syndrome: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab. 2013;98(12):4565–92.
Elkind-Hirsch KE. Exenatide, Dapagliflozin, or Phentermine/Topiramate Differentially Affect Metabolic Profiles in Polycystic Ovary Syndrome. J Clin Endocrinol Metab. 2021;106(10):3019–33.
Htike ZZ. Efficacy and safety of glucagon-like peptide-1 receptor agonists in type 2 diabetes: A systematic review and mixed-treatment comparison analysis. Diabetes Obes Metab. 2017;19(4):524–36.
Han Y, Li Y, He B. GLP-1 receptor agonists versus metformin in PCOS: a systematic review and meta-analysis. Reprod Biomed Online. 2019;39(2):332–42.
Siamashvili M, Davis SN. Update on the effects of GLP-1 receptor agonists for the treatment of polycystic ovary syndrome. Expert Rev Clin Pharmacol. 2021;14(9):1081–9.
Zhang J. Canagliflozin combined with metformin versus metformin monotherapy for endocrine and metabolic profiles in overweight and obese women with polycystic ovary syndrome: A single-center, open-labeled prospective randomized controlled trial. Front Endocrinol (Lausanne). 2022;13:1003238.
Cai M. Efficacy of canagliflozin versus metformin in women with polycystic ovary syndrome: A randomized, open-label, noninferiority trial. Diabetes Obes Metab. 2022;24(2):312–20.
Javed Z. Effects of empagliflozin on metabolic parameters in polycystic ovary syndrome: A randomized controlled study. Clin Endocrinol (Oxf). 2019;90(6):805–13.
Zeng Q, Xu X, Xin L. Effect of canagliflozin combined with metformin on endocrine and metabolic levels in overweight and obese women with polycystic ovary syndrome (in Chinese). Maternal & Child Health Care of China. 2022;37(24):4649–52.
McMurray JJV. Dapagliflozin in Patients with Heart Failure and Reduced Ejection Fraction. N Engl J Med. 2019;381(21):1995–2008.
Zheng RJ. Association of SGLT2 Inhibitors With Risk of Atrial Fibrillation and Stroke in Patients With and Without Type 2 Diabetes: A Systemic Review and Meta-Analysis of Randomized Controlled Trials. J Cardiovasc Pharmacol. 2022;79(2):e145–52.
Perkovic V. Canagliflozin and Renal Outcomes in Type 2 Diabetes and Nephropathy. N Engl J Med. 2019;380(24):2295–306.
Berni TR, Morgan CL, Rees DA. Women with polycystic ovary syndrome have an increased risk of major cardiovascular events: A population study. J Clin Endocrinol Metab. 2021;106(9):e3369–80.
Wekker V. Long-term cardiometabolic disease risk in women with PCOS: a systematic review and meta-analysis. Hum Reprod Update. 2020;26(6):942–60.
Catalano PM. Obesity, insulin resistance, and pregnancy outcome. Reproduction. 2010;140(3):365–71.
Lainez NM, Coss D. obesity, neuroinflammation, and reproductive function. Endocrinology. 2019;160(11):2719–36.
Ormazabal V. Association between insulin resistance and the development of cardiovascular disease. Cardiovasc Diabetol. 2018;17(1):122.
Pruett JE. Mitochondrial function and oxidative stress in white adipose tissue in a rat model of PCOS: effect of SGLT2 inhibition. Biol Sex Differ. 2022;13(1):45.
He YL. The effects of licogliflozin, a dual SGLT1/2 inhibitor, on body weight in obese patients with or without diabetes. Diabetes Obes Metab. 2019;21(6):1311–21.
Tan S. Licogliflozin versus placebo in women with polycystic ovary syndrome: A randomized, double-blind, phase 2 trial. Diabetes Obes Metab. 2021;23(11):2595–9.
Labrie F. Is dehydroepiandrosterone a hormone? J Endocrinol. 2005;187(2):169–96.
Leowattana W. DHEAS as a new diagnostic tool. Clin Chim Acta. 2004;341(1–2):1–15.
Hoffman DI, Klove K, Lobo RA. The prevalence and significance of elevated dehydroepiandrosterone sulfate levels in anovulatory women. Fertil Steril. 1984;42(1):76–81.
Steinberger E, Smith KD, Rodriguez-Rigau LJ. Testosterone, dehydroepiandrosterone, and dehydroepiandrosterone sulfate in hyperandrogenic women. J Clin Endocrinol Metab. 1984;59(3):471–7.
Longcope C. Adrenal and gonadal androgen secretion in normal females. Clin Endocrinol Metab. 1986;15(2):213–28.
Qiao J, Feng HL. Extra- and intra-ovarian factors in polycystic ovary syndrome: impact on oocyte maturation and embryo developmental competence. Hum Reprod Update. 2011;17(1):17–33.
Naver KV. Increased risk of preterm delivery and pre-eclampsia in women with polycystic ovary syndrome and hyperandrogenaemia. BJOG. 2014;121(5):575–81.
Rachoń D, Teede H. Ovarian function and obesity–interrelationship, impact on women’s reproductive lifespan and treatment options. Mol Cell Endocrinol. 2010;316(2):172–9.
Sanchez-Garrido MA, Tena-Sempere M. Metabolic dysfunction in polycystic ovary syndrome: Pathogenic role of androgen excess and potential therapeutic strategies. Mol Metab. 2020;35:100937.
Escobar-Morreale HF, San Millán JL. Abdominal adiposity and the polycystic ovary syndrome. Trends Endocrinol Metab. 2007;18(7):266–72.
Cena H, Chiovato L, Nappi RE. Obesity, Polycystic Ovary Syndrome, and Infertility: A New Avenue for GLP-1 Receptor Agonists. J Clin Endocrinol Metab. 2020;105(8):e2695–709.
Acknowledgements
This systematic review and meta-analysis did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Ethics Approval
Not applicable.
Competing Interests
Not applicable.
Consent to Participate
Not applicable.
Consent for Publication
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Zhang, L., Wang, Z., Kong, L. et al. Effect of SGLT2 Inhibitors on Improving Glucolipid Metabolism and Reproductive Hormone Status in Overweight/Obese Women with PCOS: A Systematic Review and Meta-Analysis. Reprod. Sci. (2023). https://doi.org/10.1007/s43032-023-01415-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s43032-023-01415-5