Abstract
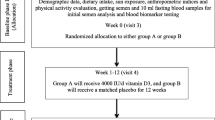
The objective is to evaluate the effects of vitamin D3 (VD3) on sperm parameters and seminal and serum oxidative stress (OS) biomarkers in asthenozoospermia infertile men. This randomized, triple-masking, placebo-controlled clinical trial conducted on 86 asthenozoospermia infertile men with serum 25 hydroxy vitamin D3 (25-OH-D3) < 30 ng/ml in the infertility clinic of Ahvaz Jahad Daneshgahi, Iran. Patients were randomly allocated to groups A and B, who received daily 4000 IU vitamin D3 (VD3) and matching placebo respectively for 3 months. Demographic data, dietary intake, physical activity, sun exposure, anthropometric indices, serum and seminal levels of MDA (Malondialdehyde), 8-hydroxy-2- Dioxy Guanosine (8-OHDG), total antioxidant capacity (TAC) and calcium, sperm DNA fragmentation index (DFI), serum 25-OH-D3, parathyroid hormone (PTH), phosphorus, and sperm parameters were assessed. VD3 supplementation had no significant effects on body weight, body mass index (BMI), waist circumference (WC), body fat (BF), 8-OHDG, DFI, semen volume, sperm count, and normal sperm morphology, but increased post-intervention mean and mean change of serum 25-OH-D3 (P < 0.001, P < 0.001), PTH (P < 0.001, P < 0.001) and phosphorus (P = 0.009, P = 0.049) and seminal calcium (P = 0.035, P = 0.038) and serum calcium (P = 0.008, P = 0.009), seminal TAC (P < 0.001, P < 0.001), and serum TAC (P = 0.007, P = 005), total sperm motility (P < 0.001, P < 0.001) and progressive sperm motility (P < 0.001, P < 0.001) and decreased seminal MDA (P = 0.017, P = 0.004) and serum MDA (P = 006, P = 0.005) significantly compared to the baseline and placebo group respectively. VD3 supplementation may modulate OS and affect sperm motility in men with asthenozoospermia and serum 25-OH-D3 < 30 ng/ml. Iran Clinical Trials Registry, ID: IRCT20151128025274N4, registered on 28 March 2018, URL of trial registry record: https://www.irct.ir/trial/29983

Similar content being viewed by others
Data Availability
Datasets are available through the corresponding author upon reasonable request.
Code Availability
Not applicable.
References
Kazemijaliseh H, Ramezani Tehrani F, Behboudi-Gandevani S, Hosseinpanah F, Khalili D, Azizi F. The prevalence and causes of primary infertility in Iran: a population-based study. Global J Health Sci. 2015;7:226–32. https://doi.org/10.5539/gjhs.v7n6p226.
Agarwal A, Mulgund A, Hamada A, Chyatte MR. A unique view on male infertility around the globe. Reprod Biol Endocrinol. 2015;13:37–45. https://doi.org/10.1186/s12958-015-0032-1.
Hasanpoor Azghdy SB, Simbar M, Vedadhir A, Hossein Rashid B. Psychological impact of infertility among infertile women. Adv Nurs Midwifery. 2014;23:1–10.
Kumar N, Singh AK. Trends of male factor infertility, an important cause of infertility: a review of literature. J Hum Reprod Sci. 2015;8:191–6. https://doi.org/10.4103/0974-1208.170370.
Pereira R, Sá R, Barros A, Sousa M. Major regulatory mechanisms involved in sperm motility. Asian J Androl. 2017;19:5–14. https://doi.org/10.4103/1008-682x.167716.
Villaverde AISB, Netherton J, Baker MA. From past to present: the link between reactive oxygen species in sperm and male infertility. Antioxidants (Basel). 2019;8:616–35. https://doi.org/10.3390/antiox8120616.
Du Plessis SS, Agarwal A, Halabi J, Tvrda E. Contemporary evidence on the physiological role of reactive oxygen species in human sperm function. J Assist Reprod Genet. 2015;32:509–20. https://doi.org/10.1007/s10815-014-0425-7.
Imamovic Kumalic S, Pinter B. Review of clinical trials on effects of oral antioxidants on basic semen and other parameters in idiopathic oligoasthenoteratozoospermia. Biomed Res Int. 2014;2014:1–11. https://doi.org/10.1155/2014/426951.
Karavolos S, Panagiotopoulou N, Alahwany H, Martins da Silva S. An update on the management of male infertility. Obstet Gynecol. 2020;22:267–74. https://doi.org/10.1111/tog.12688.
Ko EY, Sabanegh ES Jr, Agarwal A. Male infertility testing: reactive oxygen species and antioxidant capacity. Fertil Steril. 2014;102:1518–27. https://doi.org/10.1016/j.fertnstert.2014.10.020.
Torres-Arce E, Vizmanos B, Babio N, Márquez-Sandoval F, Salas-Huetos A. Dietary antioxidants in the treatment of male infertility: counteracting oxidative stress. Biology. 2021;10:241–80. https://doi.org/10.3390/biology10030241.
Amrein K, Scherkl M, Hoffmann M, Neuwersch-Sommeregger S, Köstenberger M, Tmava Berisha A, et al. Vitamin D deficiency 2.0: an update on the current status worldwide. Eur J Clin Nutr. 2020;74:1498–513. https://doi.org/10.1038/s41430-020-0558-y.
Blomberg JM. Vitamin D and male reproduction. Nat Rev Endocrinol. 2014;10:175–86. https://doi.org/10.1038/nrendo.2013.262.
Merino O, Sánchez R, Gregorio MB, Sampaio F, Risopatrón J. Effect of high-fat and vitamin D deficient diet on rat sperm quality and fertility. Theriogenology. 2019;125:6–11. https://doi.org/10.1016/j.theriogenology.2018.09.030.
Arab A, Hadi A, Moosavian SP, Askari G, Nasirian M. The association between serum vitamin D, fertility and semen quality: a systematic review and meta-analysis. Int J Surg. 2019;71:101–9. https://doi.org/10.1016/j.ijsu.2019.09.025.
Abbasihormozi S, Kouhkan A, Alizadeh AR, Shahverdi AH, Nasr-Esfahani MH, Sadighi Gilani MA, et al. Association of vitamin D status with semen quality and reproductive hormones in Iranian subfertile men. Andrology. 2017;5:113–8. https://doi.org/10.1111/andr.12280.
Dcunha R, Hussein RS, Ananda H, Kumari S, Adiga SK, Kannan N, et al. Current insights and latest updates in sperm motility and associated applications in assisted reproduction. Reprod Sci. 2020;7:1–19. https://doi.org/10.1007/s43032-020-00408-y.
Pizzorno J. Environmental toxins and infertility. Integr Med. (Encinitas). 2018;17:8–11.
Deng XL, Li YM, Yang XY, Huang JR, Guo SL. Song LM [Efficacy and safety of vitamin D in the treatment of idiopathic oligoasthenozoospermia]. Zhonghua Nan Ke Xue. 2014;20:1082–5.
Holick MF, Binkley NC, Bischoff-Ferrari HA, Gordon CM, Hanley DA, Heaney RP, et al. Evaluation, treatment, and prevention of vitamin D deficiency: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab. 2011;96:1911–30. https://doi.org/10.1210/jc.2011-0385.
Institute of Medicine Committee to Review Dietary Reference Intakes for Vitamin D, Calcium. The National Academies Collection: Reports funded by National Institutes of Health. In: Ross AC, CL Taylor, AL Yaktine, HB Del Valle, editors. Dietary reference intakes for calcium and vitamin D. Washington (DC): National Academies Press (US),Copyright © 2011, National Academy of Sciences.; 2011.
Lavelle G, Noorkoiv M, Theis N, Korff T, Kilbride C, Baltzopoulos V, et al. Validity of the International Physical Activity Questionnaire Short Form (IPAQ-SF) as a measure of physical activity (PA) in young people with cerebral palsy: a cross-sectional study. Physiotherapy. 2020;107:209–15. https://doi.org/10.1016/j.physio.2019.08.013.
Nikooyeh B, Neyestani TR, Farvid M, Alavi-Majd H, Houshiarrad A, Kalayi A, et al. Daily consumption of vitamin D- or vitamin D + calcium-fortified yogurt drink improved glycemic control in patients with type 2 diabetes: a randomized clinical trial. Am J Clin Nutr. 2011;93:764–71. https://doi.org/10.3945/ajcn.110.007336.
Cooper TG, Noonan E, von Eckardstein S, Auger J, Baker HW, Behre HM, et al. World Health Organization reference values for human semen characteristics. Hum Reprod Update. 2010;16:231–45. https://doi.org/10.1093/humupd/dmp048.
Evenson DP. Sperm chromatin structure assay (SCSA®). Methods Mol Biol. 2013;927:147–64. https://doi.org/10.1007/978-1-62703-038-0_14.
Blomberg Jensen M, Lieben L, Nielsen JE, Willems A, Jorgensen A, Juul A, et al. Characterization of the testicular, epididymal and endocrine phenotypes in the Leuven Vdr-deficient mouse model: targeting estrogen signalling. Mol Cell Endocrinol. 2013;377:93–102. https://doi.org/10.1016/j.mce.2013.06.036.
Sun W, Chen L, Zhang W, Wang R, Goltzman D, Miao D. Active vitamin D deficiency mediated by extracellular calcium and phosphorus results in male infertility in young mice. Am J Physiol Endocrinol Metab. 2015;308:51–62. https://doi.org/10.1152/ajpendo.00076.2014.
Merino O, Sánchez R, Gregorio BM, Sampaio FJ, Risopatrón J. Effects of diet-induced obesity and deficient in vitamin D on spermatozoa function and DNA integrity in Sprague-Dawley rats. BioMed Research International. 2018;2018:5479057. https://doi.org/10.1155/2018/5479057
Blomberg Jensen M, Bjerrum PJ, Jessen TE, Nielsen JE, Joensen UN, Olesen IA, et al. Vitamin D is positively associated with sperm motility and increases intracellular calcium in human spermatozoa. Hum Reprod. 2011;26:1307–17. https://doi.org/10.1093/humrep/der059.
Jueraitetibaike K, Ding Z, Wang D-D, Peng L-P, Jing J, Chen L, et al. The effect of vitamin D on sperm motility and the underlying mechanism. Asian J Androl. 2019;21:400–7. https://doi.org/10.4103/aja.aja_105_18.
Moghadam MT, Hosseini G, Absalan F, Tabar MH, Nikbakht R. Effects of vitamin D on apoptosis and quality of sperm in asthenozoospermia. JBRA Assist Reprod. 2020;24:316–23. https://doi.org/10.5935/1518-0557.20200009.
Taheri Moghadam M, Asadi Fard Y, Saki G, Nikbakht R. Effect of vitamin D on apoptotic marker, reactive oxygen species and human sperm parameters during the process of cryopreservation. Iran J Basic Med Sci . 2019;22:1036–43. https://doi.org/10.22038/ijbms.2019.36258.8634.
Alzoubi A, Mahdi H, Al Bashir S, Halalsheh O, Al Ebbini M, Alzarir M, et al. Normalization of serum vitamin D improves semen motility parameters in patients with idiopathic male infertility. Acta Endocrinol (Buchar). 2017;13:180–7. https://doi.org/10.4183/aeb.2017.180.
Blomberg Jensen M, Lawaetz JG, Petersen JH, Juul A, Jørgensen N. Effects of vitamin D supplementation on semen quality, reproductive hormones, and live birth rate: a randomized clinical trial. J Clin Endocrinol Metab. 2018;103:870–81. https://doi.org/10.1210/jc.2017-01656.
Amini L, Mohammadbeigi R, Vafa M, Haghani H, Vahedian-Azimi A, Karimi L, et al. Evaluation of the effect of vitamin D3 supplementation on quantitative and qualitative parameters of spermograms and hormones in infertile men: a randomized controlled trial. Complement Ther Med. 2020;53:1–9.
Blomberg Jensen M, Gerner Lawaetz J, Andersson AM, Petersen JH, Nordkap L, Bang AK, et al. Vitamin D deficiency and low ionized calcium are linked with semen quality and sex steroid levels in infertile men. Hum Reprod. 2016;31:1875–85. https://doi.org/10.1093/humrep/dew152.
Agarwal A, Parekh N, Panner Selvam MK, Henkel R, Shah R, Homa ST, et al. Male oxidative stress infertility (MOSI): proposed terminology and clinical practice guidelines for management of idiopathic male infertility. World J Mens Health. 2019;37:296–312. https://doi.org/10.5534/wjmh.190055.
Alahmar AT. Role of oxidative stress in male infertility: an updated review. J Hum Reprod Sci. 2019;12:4–18. https://doi.org/10.4103/jhrs.JHRS_150_18.
Nadjarzadeh A, Mehrsai A, Mostafavi E, Gohari MR, Shidfar F. The association between dietary antioxidant intake and semen quality in infertile men. Med J Islam Repub Iran. 2013;27:204–9.
Pahune PP, Choudhari AR, Muley PA. The total antioxidant power of semen and its correlation with the fertility potential of human male subjects. J Clin Diagn Res. 2013;7:991–5. https://doi.org/10.7860/jcdr/2013/4974.3040.
Agarwal A, Sekhon LH. Oxidative stress and antioxidants for idiopathic oligoasthenoteratospermia: Is it justified? Indian J Urol. 2011;27:74–85. https://doi.org/10.4103/0970-1591.78437.
Kumaresan A, Das Gupta M, Datta TK, Morrell JM. Sperm DNA integrity and male fertility in farm animals: a review. Front Vet Sci. 2020;7:1–15. https://doi.org/10.3389/fvets.2020.00321.
Tremellen K. Oxidative stress and male infertility–a clinical perspective. Hum Reprod Update. 2008;14:243–58. https://doi.org/10.1093/humupd/dmn004.
Kim GY. What should be done for men with sperm DNA fragmentation? Clin Exp Reprod Med. 2018;45:101–9. https://doi.org/10.5653/cerm.2018.45.3.101.
Panner Selvam MK, Agarwal A. A systematic review on sperm DNA fragmentation in male factor infertility: laboratory assessment. Arab J Urol. 2018;16:65–76. https://doi.org/10.1016/j.aju.2017.12.001.
Rubal L, Hernandez AM, Ingles S, Scrooc M, Bendikson K. Do serum vitamin D levels correlate with semen analysis parameters and sperm DNA fragmentation? Fertil Steril. 2012;98:47–8. https://doi.org/10.1016/j.fertnstert.2012.07.170.
Sharifi N, Amani R, Hajiani E, Cheraghian B. Does vitamin D improve liver enzymes, oxidative stress, and inflammatory biomarkers in adults with non-alcoholic fatty liver disease? A randomized clinical trial. Endocrine. 2014;47:70–80. https://doi.org/10.1007/s12020-014-0336-5.
Coussens AK, Martineau AR, Wilkinson RJ. Anti-inflammatory and antimicrobial actions of vitamin D in Combating TB/HIV. Scientifica. 2014;2014:1–13. https://doi.org/10.1155/2014/903680.
Shab-Bidar S, Neyestani TR, Djazayery A, Eshraghian MR, Houshiarrad A, Kalayi A, et al. Improvement of vitamin D status resulted in amelioration of biomarkers of systemic inflammation in the subjects with type 2 diabetes. Diabetes Metab Res Rev. 2012;28:424–30. https://doi.org/10.1002/dmrr.2290.
Cannell JJ, Grant WB. What is the role of vitamin D in autism? Dermatoendocrinol. 2013;5:199–204. https://doi.org/10.4161/derm.24356.
Jain SK, Micinski D. Vitamin D upregulates glutamate cysteine ligase and glutathione reductase, and GSH formation, and decreases ROS and MCP-1 and IL-8 secretion in high-glucose exposed U937 monocytes. Biochem Biophys Res Commun. 2013;437:7–11. https://doi.org/10.1016/j.bbrc.2013.06.004.
Asemi Z, Samimi M, Tabassi Z, Shakeri H, Esmaillzadeh A. Vitamin D supplementation affects serum high-sensitivity C-reactive protein, insulin resistance, and biomarkers of oxidative stress in pregnant women. J Nutr. 2013;143:1432–8. https://doi.org/10.3945/jn.113.177550.
Acknowledgements
The authors would like to express their sincere gratitude to Vice Chancellor of Research, Ahvaz Jundishapur University of Medical Sciences, Ahvaz Center of Therapy and Research Infertility Jahad Daneshgahi, the staff of Biochemistry Laboratory of School of Allied Medical Sciences, and trial participants.
Funding
This study was a part of the Ph.D. thesis of Leila Maghsoumi-Norouzabad that was supported by Vice Chancellor of Research, Ahvaz Jundishapur University of Medical Sciences (Ahvaz, Iran) [grant number NRC-9634].
Author information
Authors and Affiliations
Contributions
AZ, LMN, AM, MD, and AS: involved in design and data extraction. LMN: drafted the manuscript. AZ and AM: performed the critical review. The manuscript has been revised and approved by all authors.
Corresponding author
Ethics declarations
Ethics Approval
This study has been approved by Medical Ethics Committee of Ahvaz Jundishapur University of Medical Sciences and is in accordance with the Declaration of Helsinki (approval number IR.AJUMS.REC.1396.1013). This investigation has been registered in Iranian Registry of Clinical Trials (IRCT registration number IRCT20151128025274N4).
Consent to Participate
All participants signed informed consent forms.
Consent for Publication
Not applicable.
Competing Interests
The authors declare no competing interests.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Maghsoumi-Norouzabad, L., Zare Javid, A., Mansoori, A. et al. Vitamin D3 Supplementation Effects on Spermatogram and Oxidative Stress Biomarkers in Asthenozoospermia Infertile Men: a Randomized, Triple-Blind, Placebo-Controlled Clinical Trial. Reprod. Sci. 29, 823–835 (2022). https://doi.org/10.1007/s43032-021-00769-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s43032-021-00769-y