Abstract
Purpose
A priori cardiovascular (CV) health status may impact reductions in risk factors and CV mortality and morbidity following exercise training, although this is not fully understood. Therefore, the purpose of the study was to examine if endothelial function (assessed via flow mediated dilation; FMD%), predicts the magnitude of change in CV risk factors or fitness following exercise training.
Methods
We pooled data from 338 individuals who underwent supervised exercise training (8–26 weeks). Using recent sex- and age-specific reference values for flow-mediated dilation (FMD%), we categorised participants as having preserved endothelial function (P-EF) (> 50th percentile of reference value, 56 females, 67 males, 46 ± 17 years) or reduced endothelial function (R-EF) (< 50th percentile of reference value, 67 females, 148 males, 48 ± 17 years). The effects of exercise training on cardiovascular risk factors (BMI, cholesterol, glucose and triglycerides), cardiorespiratory fitness (VO2peak) and vascular function (FMD%) were examined using a two-way mixed design general linear model.
Results
Exercise training significantly improved physical fitness (P < 0.001), with no difference in the magnitude of improvement between P-EF and R-EF. Modest but significant reductions were present in BMI, blood pressure and total cholesterol (all P < 0.005), with no difference between P-EF and R-EF groups in the magnitude of changes in these variables with training. Exercise training did not significantly alter glucose, triglycerides, high density lipoprotein (HDL) and low-density lipoprotein (LDL) (all P > 0.05).
Conclusion
Individuals with reduced and preserved a priori endothelial function status can obtain benefits from exercise in terms of risk factor modification and fitness change. Therefore, exercise has the potential to be beneficial in all clinical groups.
Similar content being viewed by others
Introduction
Cardiovascular disease (CVD) is the leading causes of death worldwide and is one of the most serious health problems throughout the world [38, 46]. Regular exercise training and/or physical activity is a conventional and non-pharmological strategy that effectively reduces the risk for development and progression of cardiovascular disease [14]. Benefits of exercise are only partly explained through improvements in traditional cardiovascular disease risk factors, e.g., blood pressure [29], body weight [33], glucose homeostasis [34], cholesterol [13], and cardiorespiratory fitness [10]. Benefits of exercise training also relate to improvements in vascular health, including endothelial function [3, 18, 21, 58].
Endothelial function, measured as flow mediated dilation (FMD), is largely nitric oxide (NO)-mediated [16] and predicts future CV events [19]. It is therefore considered an early marker of future atherosclerotic vascular risk and a non-invasive window into vascular health status. Recently, age and sex-specific FMD reference intervals for healthy individuals have been published [27]. It has been consistently reported that age and sex-specific differences in FMD are present [28, 50, 53, 62] with sex altering the age-related decline in FMD. [27]. FMD references intervals that account for these differences allow for a clinical interpretation of FMD.
Some epidemiological evidence suggests that individuals with CVD gain less benefit from regular physical activity, in terms of relative risk reduction for all-cause mortality and morbidity, than apparently healthy individuals [32, 41, 42]. In addition, a recent study demonstrated that cardiovascular (CV) health status alters the dose–response between moderate to vigorous physical activity (MVPA) and incident morbidity and mortality among 143,493 adults [4]. Healthy individuals and those with CV risk factors presented with a curvilinear relation, whilst those with established CVD presented a more gradual, linear relation, suggesting a smaller risk reduction from regular physical activity in those with CVD [16, 36]. This could have implications for the benefits of exercise training and interventions in these individuals.
Whilst a priori cardiovascular health status may impact reductions in risk factors and CV mortality and morbidity, currently, it is not known whether a priori endothelial dysfunction impacts upon exercise-training adaptation in CV risk factors and fitness. Therefore, the aim of this study was to investigate whether a priori endothelial dysfunction is associated with distinct training-induced improvement in traditional CVD risk factors, cardiopulmonary fitness, or vascular function by performing a secondary analysis in a large cohort of 338 individuals who performed supervised exercise training. Supported by our previous work on endothelial (dys)function [16, 36], it was hypothesised that those with a priori endothelial dysfunction would show smaller improvements in CV risk factors and cardiopulmonary fitness compared to those with a priori preserved endothelial function.
Methods
Participants
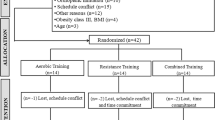
Endurance exercise training studies performed in our laboratories (Liverpool, Perth, Nijmegen) which met the following criteria were included in this analysis: (1) completion of moderate-intensity supervised exercise ≥ 8 weeks; (2) the exercise sessions consisted of endurance (aerobic) exercise involving large muscle groups or combined aerobic and resistance exercise (CARE) sessions; (3) exercise training was performed ≥ 2 times per week with a duration of ≥ 30 min; (4) measurements of baseline FMD and age were available to categorize a priori endothelial function based on [27] equations, (5) endothelial function (FMD) measurements were performed strictly adhering to expert consensus guidelines [55, 56], (6) the exercise study was approved by the local ethics committees and conformed to the standards of the Declaration Helsinki. Participants were asked not to modify their diet and lifestyle factors during the programme, no studies controlled the participants’ diet throughout their study. Smokers were excluded as well as studies which included children, adolescents, or pregnant women. Additionally, any changes in brachial artery diameter or FMD that was > 3 times the overall standard deviation were removed. This led to the inclusion of 19 studies (Table 1) with 338 participants for this secondary analysis, with a wide range of different health statuses included: healthy young, older sedentary, individuals with non-alcoholic fatty liver disease (NAFLD), polycystic ovary syndrome (PCOS), type 2 diabetes, elite rowers, and individuals with CVD risk. Please see Table 1 for further details.
We performed a power calculation, to achieve a power of 80% with level of significance of 5% (two side) based on the ability to detect a 1% difference in the change in FMD over time between the two groups, with a standard deviation of the difference of 2.5%, we need to include at least 99 participants in each group.
Experimental Design
Subject characteristics and traditional CV risk factors were recorded pre and post exercise training. All physiological measures pre and post the exercise intervention were performed following an overnight fast and participants were asked to abstain from strenuous exercise for > 24 h and caffeine and alcohol for > 12 h before testing. Post measurements were completed 1–4 days following the last exercise session. Presence of pre-training endothelial dysfunction was determined using published FMD reference values [27]. Specifically, individuals were categorised as possessing “reduced endothelial function, R-EF” when pre-training FMD was lower than the age- and sex specific FMD reference values using the 50th percentile as the cut-off value [27] and preserved endothelial function (P-EF) when at or above the 50th percentile for age- and sex specific FMD reference values.
Experimental Procedures
Subject Characteristics
Subject characteristics were measured pre and post the exercise training intervention. Height, weight, body mass index (BMI), waist circumference and waist to hip ratio were measured using standard methods. Body fat percentage was measured either via dual X-Ray Absorptiometry (DXA) or skin fold measurements using standard techniques. Measurements of blood pressure were conducted after ≥ 5-min rest in a seated or supine position using a manual or automated sphygmomanometer and were repeated at least twice and were averaged.
Cardiopulmonary Fitness
Peak oxygen consumption (VO2peak) was measured during a maximal graded exercise test on a treadmill, a cycle ergometer or a rower. VO2peak values are presented relative to body weight (ml/kg/min) (Supplementary Table 1).
Endothelial Function
FMD assessments were performed in a quiet, temperature-controlled laboratory at the same time of day to avoid diurnal effects. Participants were asked to avoid alcohol, caffeine consumption and vigorous exercise for ≥ 12 h before testing. Subjects rested for ≥ 15 min in the supine position. The participants’ arm was extended and positioned at an angle ∼80 degree from the torso. A rapid inflation and deflation pneumatic cuff was positioned on the forearm and inflated to suprasystolic pressure to induce ischemia. B-mode images were obtained with a ≥ 7.5 MHz multifrequency linear array probe attached to a high-resolution ultrasound machine was used to image the brachial artery in the distal one-third of the upper arm. One study used a Megas ultrasound device (Esaote, Firenze, Italy), whilst all other studies used either the Aspen Acuson (Mountain view, CA, USA) or a Terason, t3000, (Aloka, Burlington, MA, USA) (Supplementary Table 1). Baseline diameter, flow and shear stress measurements were recorded for ≥ 1 min before the forearm cuff was inflated for 5 min. Diameter and flow recordings resumed 30 s prior to cuff deflation and continued for 3 min post deflation. FMD was calculated as peak artery diameter following hyperaemia, expressed as % increase using an allometric model. All analysis was performed using custom designed edge detection and wall tracking software which is largely independent of investigator bias (Woodman et al. 2001).
Cardiovascular Blood Parameters
Venous blood samples were taken to assess fasted glucose, total cholesterol, high density lipoprotein (HDL) cholesterol, low-density lipoprotein (LDL) cholesterol as well as triglycerides. The blood samples were analysed in accredited laboratory facilities.
Statistical Analysis
The effect of a priori endothelial function on improvements in endothelial function and CVD risk factors in response to exercise training were determined using a two-way mixed design general linear model, with a within subject factor of time (pre- versus post-training) and a between subject factor of group (endothelial function vs endothelial dysfunction). Data analysis was performed using SPSS (Version 26; SPSS Inc., Chicago, IL). Statistical significance was delimited at P < 0.05 and exact P values are cited (P values of ‘0.000’ provided by the statistics package are reported as < 0.001).
Results
A total of 338 participants were included in the study. Following the age- and sex-based reference values, we classified 123 (56 female, 67 male) participants as possessing preserved endothelial function (P-EF) and 215 (69 female, 146 male) as having a priori reduced endothelial function (R-EF). The duration of exercise training varied, with n = 127 having undertaken an 8-week exercise intervention (P-EF: n = 40, R-EF: n = 87), n = 164 completed a 12-week intervention (P-EF: n = 58, R-ED: n = 106), n = 15 completed a 16-week intervention (P-EF: n = 5, R-EF: n = 10), and n = 32 completed a ≥ 24-week intervention (P-EF: n = 20, R-EF: n = 12). Details of the exercise training interventions are summarised in Table 1.
Baseline Characteristics
Prior to training, we found no differences between P-EF versus R-ED in general characteristics or in cardio-respiratory fitness (Table 2). Regarding traditional CVD risk factors, we found significantly higher baseline systolic blood pressure, triglycerides and fasted glucose levels in R-EF, whilst no differences were found for diastolic or mean blood pressure, cholesterol, LDL and HDL (Table 2). As a consequence of the group allocation, the R-EF-group demonstrated a significantly lower FMD%, compared to those with P-EF.
Impact of Exercise Training
Cardiovascular Risk Factors
Exercise training caused modest but significant reductions in body weight, BMI, percentage body fat, waist circumference, blood pressure (diastolic, systolic and mean) and total cholesterol (all P < 0.05). The magnitude of these changes were not different between preserved P-EF and R-ED (Table 3). Exercise training did not significantly alter serum levels of glucose, triglycerides, HDL and LDL (Table 3).
Cardiorespiratory Fitness
Exercise training improved cardiorespiratory fitness in those with preserved endothelial function and with reduced endothelial function [F(1, 291) = 136.199, P < 0.001]. This effect of training on VO2peak was not significantly different between groups with both groups showing a significant improvement [interaction, F (1, 291) = 1.402, P = 0.237] (Table 3).
Brachial Artery Diameter and Endothelial Function
Brachial artery FMD increased over time in response to exercise training [F (1, 335) = 10.092, P = 0.002], which differed between groups [interaction effect; F (1, 335) = 42.942, P < 0.001] (Table 2). Post-hoc tests indicated little change in FMD% in preserved EF, whilst an increase was found in ED (P < 0.001). Exercise training significantly increased resting brachial artery diameter [F (1, 322) = 9.334, P = 0.002]. The magnitude of this increase in resting diameter following exercise training was not different between groups [F (1, 322) = 0.056, P = 0.813].
Discussion
The aim of the present study was to investigate whether a priori endothelial function status is associated with distinct training-induced improvement in traditional CV risk factors, cardiorespiratory fitness, and vascular function. To this end, we performed analysis on 338 participants who all underwent supervised exercise training in our laboratory, with pre- and post-training evaluation of endothelial function, cardiovascular risk factors and fitness. Overall, our data suggest that exercise training improved cardiorespiratory fitness, flow-mediated dilation and some (i.e. body weight, BMI, body fat percentage, waist circumference and blood pressure) but not all (i.e. fasting glucose, HDL, LDL and triglycerides) cardiovascular risk factors. After dividing the group into a priori reduced endothelial function (R-ED; n = 215) and preserved endothelial function (P-EF; n = 123), we found comparable improvements in cardiovascular risk factors and physical fitness following exercise training in both groups. Interestingly, only those with a priori endothelial dysfunction demonstrated improvement in endothelial function (FMD%) after exercise training, whereas no change was found in subjects with P-EF who started with higher endothelial function, supporting previous findings [17]. Overall, our study suggests that the benefits of exercise training on many clinically important risk factors are independent of a priori endothelial dysfunction status,although a period of 8–12 weeks of moderate intensity exercise may not enhance endothelial function in those with P-EF.
Previous epidemiology research has shown that moderate to vigorous physical activity is beneficial for reducing adverse outcomes, however the shape of the association is dependent upon health. A curvilinear association between healthy and individuals with CV risk factors and PA whilst a linear association was found between individuals with CVD [4]. This supports our findings that individuals do benefit from physical activity however, the response may be different between those with have reduced endothelial function and preserved endothelial function. A unique aspect of our study was our classification of individuals into endothelial function or dysfunction by comparing individuals’ FMD-values with recently published age- and sex- specific reference intervals for FMD [27]. Sex and age specific recommendations were important to consider as higher FMD in females, but also the steeper decline in FMD with age, compared with males may relate to differences in sex hormones, especially since oestrogen has been linked to cardioprotective properties [39]. Adopting this approach, we observed a relatively large population with a priori reduced endothelial function (63.6%), which is the direct consequence of the inclusion of a substantial number of training studies in clinical populations and those with CV risk factors (Table 1). Findings from our study are in line with our previous observations [16, 20, 35] in that regular exercise training is capable of improving endothelial function, especially in those with a priori endothelial dysfunction [16, 36, 61] (Table 3). Indeed, endothelial dysfunction is related to chronic exposure to CV risk factors [12, 15] and CVDs [1, 26]. Furthermore, findings from our study are in line with our previous observations [35], Green, Maiorana et al. [20], Green, Eijsvogels et al. [16] in that regular exercise training is capable of improving endothelial function, especially in those with a priori endothelial dysfunction [16, 36, 61] (Table 3).
The key finding from this study is that exercise training is associated with improved CV risk factors and enhanced physical fitness; an observation that is not related to a priori endothelial status. Our previous work found that improvements in cardiovascular risk factors also occur irrespective of changes in physical fitness [24]. In fact, lower pre-training values for fitness and impaired CV risk factors or vascular function, are associated with larger training induced improvements in endothelial function in both males and females [16, 20, 35]. These previous studies and the results of the present study provide evidence to support the potency of supervised exercise training interventions to improve cardiovascular risk factors in those with a priori higher risk and/or endothelial dysfunction [4]. Indeed, those with CVD and CV risk factors typically are also characterised with endothelial dysfunction [23, 31], demonstrates smaller benefits from regular physical activity in terms of relative risk reduction for all-cause mortality and cardiovascular events. Key differences relate to study design, with our study examining changes in risk factors within subjects following (supervised) exercise training in groups of strictly selected and defined groups of healthy individuals, CVD risk and CVD. Accordingly, effects from our work can be directly related to exercise training. Studies adopting an epidemiological approach are strong in the volume and number of participants, but causal links are difficult to make, whilst levels of physical activity are estimated using (subjective) questionnaires. Such differences may contribute to the distinct findings between intervention studies and epidemiological cohort observations.
Our study has potential clinical implications; it further highlights the importance and benefits of exercise in healthy and CVD populations. Although those with reduced endothelial function had more cardiovascular disease risk factors at baseline, significant increase in FMD and improvements in risk factors were found in this population. Improvements in FMD are vital due to its prognostic value [19], with a meta-analysis suggesting that per 1% higher FMD, the risk of experiencing a cardiovascular event is 13% lower [30]. Endothelial dysfunction is an independent predictor of future cardiac events in patients with and without established coronary artery disease [44, 60]. In the current study, both groups showed improvements in multiple cardiovascular disease risk factors thus highlighting the importance of exercise training in both clinical and healthy populations. Nonetheless, it is important to highlight that subjects with endothelial dysfunction, even following the comparable improvements in cardiovascular risk factors following exercise training, presented with higher cardiovascular risk factors compared to those in the P-EF group. As this difference remained present following exercise training, this may contribute to observations from epidemiological studies, but also highlight the importance to remain physically active.
Some limitations of our study must be discussed. Firstly, controversy exists about what cut-off value represents true endothelial dysfunction, especially in relation with coronary artery endothelial function [2]. However, we quantified presence of endothelial dysfunction using the recently published age- and sex-based reference value data [27]. Importantly, these reference values were constructed based on laboratories that adopted guideline-based approaches and similar methodology to evaluate the FMD [2, 11, 54]. Whilst a strength of our study is the detailed evaluation of fitness, cardiovascular risk factors and vascular health, a limitation is that we were unable to relate these changes directly to future clinical endpoints (e.g. mortality, morbidity). Finally, our analysis only included studies in which participants completed endurance exercise or combined aerobic and resistance training, therefore results from this study cannot be extrapolated to resistance training or high intensity interval training.
In conclusion, we found that regular exercise training, irrespective of the presence of a priori endothelial dysfunction, improves physical fitness and cardiovascular risk factors, whilst only those with a priori endothelial dysfunction demonstrated improvement in endothelial function. Therefore, this study further highlights the importance of exercise training, even in those with endothelial dysfunction, to improve clinically relevant markers of cardiovascular risk.
References
Al Suwaidi J, Higano ST, Holmes DR Jr, Lennon R, Lerman A. Obesity is independently associated with coronary endothelial dysfunction in patients with normal or mildly diseased coronary arteries. J Am Coll Cardiol. 2001;37(6):1523–8.
Anderson TJ, Uehata A, Gerhard MD, Meredith IT, Knab S, Delagrange D, Lieberman EH, Ganz P, Creager MA, Yeung AC, Selwyn AP. Close relation of endothelial function in the human coronary and peripheral circulations. J Am Coll Cardiol. 1995;26(5):1235–41.
Ashor AW, Lara J, Siervo M, Celis-Morales C, Oggioni C, Jakovljevic DG, Mathers JC. Exercise modalities and endothelial function: a systematic review and dose–response meta-analysis of randomized controlled trials. Sports Med. 2015;45(2):279–96.
Bakker EA, Lee DC, Hopman MTE, Oymans EJ, Watson PM, Thompson PD, Thijssen DHJ, Eijsvogels TMH. Dose–response association between moderate to vigorous physical activity and incident morbidity and mortality for individuals with a different cardiovascular health status: A cohort study among 142,493 adults from the Netherlands. PLoS Med. 2021;18(12):e1003845.
Benda NM, Seeger JP, Stevens GG, Hijmans-Kersten BT, van Dijk AP, Bellersen L, Lamfers EJ, Hopman MT, Thijssen DH. Effects of high-intensity interval training versus continuous training on physical fitness, cardiovascular function and quality of life in heart failure patients. PLoS One. 2015;10(10):e0141256.
Birk GK, Dawson EA, Atkinson C, Haynes A, Cable NT, Thijssen DH, Green DJ. Brachial artery adaptation to lower limb exercise training: role of shear stress. J Appl Physiol. 2012;112(10):1653–8.
Black MA, Cable NT, Thijssen DH, Green DJ. Impact of age, sex, and exercise on brachial artery flow-mediated dilatation. Am J Physiol Heart Circ Physiol. 2009;297(3):H1109–16.
Buckley BJ, Thijssen DH, Murphy RC, Graves LE, Cochrane M, Gillison F, Crone D, Wilson PM, Whyte G, Watson PM. Pragmatic evaluation of a coproduced physical activity referral scheme: a UK quasi-experimental study. BMJ open. 2020;10(10):e034580.
Buckley BJ, Watson PM, Murphy RC, Graves LE, Whyte G, Thijssen DH. Carotid artery function is restored in subjects with elevated cardiovascular disease risk after a 12-week physical activity intervention. Can J Cardiol. 2019;35(1):23–6.
Blair SN, Kohl HW 3rd, Barlow CE, Paffenbarger RS Jr, Gibbons LW, Macera CA. Changes in physical fitness and all-cause mortality: a prospective study of healthy and unhealthy men. JAMA. 1995;273(14):1093–8.
Broxterman RM, Witman MA, Trinity JD, Groot HJ, Rossman MJ, Park SY, Malenfant S, Gifford JR, Kwon OS, Park SH, Jarrett CL, Shields KL, Hydren JR, Bisconti AV, Owan T, Abraham A, Tandar A, Lui CY, Smith BR, Richardson RS. Strong relationship between vascular function in the coronary and brachial arteries: a clinical coming of age for the updated flow-mediated dilation test? Hypertension. 2019;74(1):208–15.
Celermajer DS, Sorensen KE, Spiegelhalter DJ, Georgakopoulos D, Robinson J, Deanfield JE. Aging is associated with endothelial dysfunction in healthy men years before the age-related decline in women. J Am Coll Cardiol. 1994;24(2):471–6.
Dunn AL, Marcus BH, Kampert JB, Garcia ME, Kohl HW 3rd, Blair SN. Reduction in cardiovascular disease risk factors: 6-month results from Project Active. Prev Med. 1997;26(6):883–92.
Fiuza-Luces C, Santos-Lozano A, Joyner M, Carrera-Bastos P, Picazo O, Zugaza JL, Izquierdo M, Ruilope LM, Lucia A. Exercise benefits in cardiovascular disease: beyond attenuation of traditional risk factors. Nat Rev Cardiol. 2018;15(12):731–43.
Ford MA, McConnell JP, Lavi S, Rihal CS, Prasad A, Sandhu GS, Hartman SJ, Lerman LO, Lerman A. Coronary artery endothelial dysfunction is positively correlated with low density lipoprotein and inversely correlated with high density lipoprotein subclass particles measured by nuclear magnetic resonance spectroscopy. Atherosclerosis. 2009;207(1):111–5.
Green DJ, Dawson EA, Groenewoud HMM, Jones H, Thijssen DHJ. Is flow-mediated dilation nitric oxide mediated? A meta-analysis. Hypertension. 2014;63(2):376–82.
Green DJ, Eijsvogels T, Bouts YM, Maiorana AJ, Naylor LH, Scholten RR, Spaanderman ME, Pugh CJ, Sprung VS, Schreuder T, Jones H, Cable T, Hopman MT, Thijssen DH. Exercise training and artery function in humans: nonresponse and its relationship to cardiovascular risk factors. J Appl Physiol. 2014;117(4):345–52.
Green DJ, Hopman MTE, Padilla J, Laughlin MH, Thijssen DHJ. Vascular adaptation to exercise in humans: role of hemodynamic stimuli. Physiol Rev. 2017;97(2):495–528.
Green DJ, Jones H, Thijssen D, Cable NT, Atkinson G. Flow-mediated dilation and cardiovascular event prediction: does nitric oxide matter? Hypertension. 2011;57(3):363–9.
Green DJ, Maiorana A, O'Driscoll G, Taylor R. Effect of exercise training on endothelium-derived nitric oxide function in humans. J Physiol. 2004;561(1):1–25.
Green DJ, O'Driscoll G, Joyner MJ, Cable NT. Exercise and cardiovascular risk reduction: time to update the rationale for exercise? J Appl Physiol. 2008;105(2):766–8.
Green DJ, Walsh JH, Maiorana A, Best MJ, Taylor RR, O'Driscoll JG. Exercise-induced improvement in endothelial dysfunction is not mediated by changes in CV risk factors: pooled analysis of diverse patient populations. Am J Physiol-Heart Circ Physiol. 2003;285(6):H2679–87.
Grover-Páez F, Zavalza-Gómez AB. Endothelial dysfunction and cardiovascular risk factors. Diabetes Res Clin Pract. 2009;84(1):1–10.
Hartman YA, Hopman MTE, Schreuder TH, Verheggen RJHM, Scholten RR, Oudegeest-Sander MH, Poelkens F, Maiorana AJ, Naylor LH, Willems PH, Tack CJ, Thijssen DHJ, Green DJ. Improvements in fitness are not obligatory for exercise training-induced improvements in CV risk factors. Physiol Rep. 2018;6(4):e13595.
Haynes A, Naylor LH, Spence AL, Robey E, Cox KL, Maslen BA, Lautenschlager NT, Carter HH, Ainslie PN, Green DJ. Effects of land versus water walking interventions on vascular function in older adults. Med Sci Sports Exerc. 2021;53(1):83–9.
Hetzel J, Balletshofer B, Rittig K, Walcher D, Kratzer W, Hombach V, Häring HU, Koenig W, Marx N. Rapid effects of rosiglitazone treatment on endothelial function and inflammatory biomarkers. Arterioscler Thromb Vasc Biol. 2005;25(9):1804–9.
Holder SM, Bruno RM, Shkredova DA, Dawson EA, Jones H, Hopkins ND, Hopman MTE, Bailey TG, Coombes JS, Askew CD, Naylor L, Maiorana A, Ghiadoni L, Thompson A, Green DJ, Thijssen DHJ. Reference intervals for brachial artery flow-mediated dilation and the relation with cardiovascular risk factors. Hypertension. 2021;77(5):1469–80.
Hopkins ND, Dengel DR, Stratton G, Kelly AS, Steinberger J, Zavala H, Marlatt K, Perry D, Naylor LH, Green DJ. Age and sex relationship with flow-mediated dilation in healthy children and adolescents. J Appl Physiol. 2015;119(8):926–33.
Huang G, Shi X, Gibson CA, Huang SC, Coudret NA, Ehlman MC. Controlled aerobic exercise training reduces resting blood pressure in sedentary older adults. Blood Press. 2013;22(6):386–94.
Inaba Y, Chen JA, Bergmann SR. Prediction of future cardiovascular outcomes by flow-mediated vasodilatation of brachial artery: a meta-analysis. Int J Cardiovasc Imaging. 2010;26:631–40.
Jay Widmer R, Lerman A. Endothelial dysfunction and cardiovascular disease. Global Cardiol Sci Pract. 2014;2014(3):43.
Jeong S-W, Kim S-H, Kang S-H, Kim H-J, Yoon C-H, Youn T-J, Chae I-H. Mortality reduction with physical activity in patients with and without cardiovascular disease. Eur Heart J. 2019;40(43):3547–55.
Leung FP, Yung LM, Laher I, Yao X, Chen ZY, Huang Y. Exercise, vascular wall and cardiovascular diseases: an update (Part 1). Sports Med. 2008;38(12):1009–24.
MacLeod S, Terada T, Chahal BS, Boulé NG. Exercise lowers postprandial glucose but not fasting glucose in type 2 diabetes: a meta-analysis of studies using continuous glucose monitoring. Diabetes Metab Res Rev. 2013;29(8):593–603.
Maiorana A, O'Driscoll G, Taylor R, Green D. Exercise and the nitric oxide vasodilator system. Sports Med. 2003;33(14):1013–35.
Maiorana AJ, Naylor LH, Exterkate A, Swart A, Thijssen DHJ, Lam K, O'Driscoll G, Green DJ. The impact of exercise training on conduit artery wall thickness and remodeling in chronic heart failure patients. Hypertension. 2011;57(1):56–62.
Maxwell JD, France M, Finnigan LE, Carter HH, Thijssen DH, Jones H. Can exercise training enhance the repeated remote ischaemic preconditioning stimulus on peripheral and cerebrovascular function in high-risk individuals? Eur J Appl Physiol. 2021;121:1167–78.
Mensah GA, Roth GA, Fuster V. The global burden of cardiovascular diseases and risk factors: 2020 and beyond. J Am Coll Cardiol. 2019;74(20:2529–32.
Miller VM, Duckles SP. Vascular actions of estrogens: functional implications. Pharmacol Rev. 2008;60(2):210–41.
Miller G, Maxwell J, Thompson A, Cable N, Low D, George K, Jones H. The effects of exercise training in the cold on cerebral blood flow and cerebrovascular function in young healthy individuals. Auto Neurosci. 2022;238:102945.
Moholdt T, Wisløff U, Nilsen TIL, Slørdahl SA. Physical activity and mortality in men and women with coronary heart disease: a prospective population-based cohort study in Norway (the HUNT study). Eur J Prev Cardiol. 2008;15(6):639–45.
Mons U, Hahmann H, Brenner H. A reverse J-shaped association of leisure time physical activity with prognosis in patients with stable coronary heart disease: evidence from a large cohort with repeated measurements. Heart. 2014;100(13):1043–9.
Naylor LH, O'Driscoll G, Fitzsimons M, Arnolda LF, Green DJ. Effects of training resumption on conduit arterial diameter in elite rowers. Med Sci Sports Exerc. 2006;38(1):86–92.
Neunteufl T, Heher S, Katzenschlager R, Wölfl G, Kostner K, Maurer G, Weidinger F. Late prognostic value of flow-mediated dilation in the brachial artery of patients with chest pain. Am J Cardiol. 2000;86(2):207–10.
Pugh CJ, Sprung V, Jones H, Richardson P, Shojaee-Moradie F, Umpleby AM, Green DJ, Cable NT, Trenell M, Kemp GJ. Exercise-induced improvements in liver fat and endothelial function are not sustained 12 months following cessation of exercise supervision in nonalcoholic fatty liver disease. Int J Obes. 2016;40(12):1927–30.
Roth GA, Mensah GA, Fuster V. The global burden of cardiovascular diseases and risks: a compass for global action. Am Coll Cardiol Found Washington DC. 2020;76(25):2980–1.
Scholten RR, Thijssen DJ, Lotgering FK, Hopman MT, Spaanderman ME. Cardiovascular effects of aerobic exercise training in formerly preeclamptic women and healthy parous control subjects. Am J Obstet Gynecol. 2014;211(5):516.e1–e11.
Schreuder TH, Duncker DJ, Hopman MT, Thijssen DH. Randomized controlled trial using bosentan to enhance the impact of exercise training in subjects with type 2 diabetes mellitus. Exp Physiol. 2014;99(11):1538–47.
Schreuder TH, Nyakayiru J, Houben J, Thijssen DH, Hopman MT. Impact of hypoxic versus normoxic training on physical fitness and vasculature in diabetes. High Alt Med Biol. 2014;15(3):349–55.
Seals DR, Jablonski KL, Donato AJ. Aging and vascular endothelial function in humans. Clin Sci. 2011;120(9):357–75.
Sorensen K, Celermajer DS, Georgakopoulos D, Hatcher G, Betteridge DJ, Deanfield JE. Impairment of endothelium-dependent dilation is an early event in children with familial hypercholesterolemia and is related to the lipoprotein (a) level. J Clin Investig. 1994;93(1):50–5.
Sprung VS, Cuthbertson DJ, Pugh C, Aziz N, Kemp GJ, Daousi C, Green DJ, Cable NT, Jones H. Exercise training in polycystic ovarian syndrome enhances flow-mediated dilation in the absence of changes in fatness. Med Sci Sports Exerc. 2013;45(12):2234–42.
Taddei S, Virdis A, Mattei P, Ghiadoni L, Gennari A, Fasolo CB, Sudano I, Salvetti A. Aging and endothelial function in normotensive subjects and patients with essential hypertension. Circulation. 1995;91(7):1981–7.
Takase B, Uehata A, Akima T, Nagai T, Nishioka T, Hamabe A, Satomura K, Ohsuzu F, Kurita A. Endothelium-dependent flow-mediated vasodilation in coronary and brachial arteries in suspected coronary artery disease. Am J Cardiol. 1998;82(12):1535–9.
Thijssen DH, Black MA, Pyke KE, Padilla J, Atkinson G, Harris RA, Parker B, Widlansky ME, Tschakovsky ME, Green DJ. Assessment of flow-mediated dilation in humans: a methodological and physiological guideline. Am J Physiol-Heart Circ Physiol. 2011;300(1):H2–12.
Thijssen DH, Bruno RM, van Mil ACCM, Holder SM, Faita F, Greyling A, Zock PL, Taddei S, Deanfield JE, Luscher T, Green DJ, Ghiadoni L. Expert consensus and evidence-based recommendations for the assessment of flow-mediated dilation in humans. Eur Heart J. 2019;40(30):2534–47.
Thijssen D, De Groot P, Smits P, Hopman M. Vascular adaptations to 8‐week cycling training in older men. Acta Physiol (Oxf). 2007;190(3):221–8.
Tinken TM, Thijssen DHJ, Hopkins N, Dawson EA, Cable NT, Green DJ. Shear stress mediates endothelial adaptations to exercise training in humans. Hypertension. 2010;55(2):312–8.
Tinken TM, Thijssen DH, Black MA, Cable NT, Green DJ. Time course of change in vasodilator function and capacity in response to exercise training in humans. J Physiol. 2008;586(20):5003–12.
Vita JA, Keaney JF Jr. Endothelial function: a barometer for cardiovascular risk? Am Heart Assoc. 2002;106:640–2.
Walsh JH, Bilsborough W, Maiorana A, Best M, O'Driscoll GJ, Taylor RR, Green DJ. Exercise training improves conduit vessel function in patients with coronary artery disease. J Appl Physiol. 2003;95(1):20–5.
Yao F, Liu Y, Liu D, Wu S, Lin H, Fan R, Li C. Sex differences between vascular endothelial function and carotid intima-media thickness by Framingham Risk Score. J Ultrasound Med. 2014;33(2):281–6.
Funding
The authors have not disclosed any funding.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of Interest
The authors declare that no funds, grants or other support were received during the preparation of this manuscript. The authors have no relevant financial or non-financial interests to disclose. Individual study data collection was obtained from studies published by Toni M Tinken, Mark A Black, Birk, Jamie Pugh, Victoria S Sprung, Benjamin JR Buckley, Gemma D Miller, Joseph D Maxwell, Dick HJ Thijssen, Tim HA Schreuder, Gerwen Lammers, Ralph R Scholten, Nathalie MM Brenda, Danny J Green, Louise H Naylor, Andrew Haynes, Lauren McKeown. All individual study data was collated by Dick HJ Thijssen and Danny J Green. Analysis was performed by Hannah L McLellan, Dick HJ Thijssen and Ellen A Dawson. The first draft of the manuscript was written by Hannah L McLellan and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript. For each individual study, ethical approval was received from the university that each study took place in and was performed in line with the principles of the Declaration of Helsinki. Informed consent was obtained from all individual participants included in the study
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
McLellan, H.L., Dawson, E.A., Hopkins, N.D. et al. Relation Between Endothelial Dysfunction and Exercise Training-Mediated Adaptation in Cardiovascular Risk Factors, Cardiorespiratory Fitness, and Vascular Health in Humans: A secondary analysis. J. of SCI. IN SPORT AND EXERCISE (2024). https://doi.org/10.1007/s42978-023-00270-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s42978-023-00270-9