Abstract
We investigated the conceptualization and impact of adverse childhood experiences (ACEs) in a sample of 231 children ages 3–5 living in poverty and experiencing homelessness, focusing specifically on caregiver well-being and housing instability. Data was collected using the Neurodevelopmental Ecological Screening Tool (NEST), which screens for developmental risk and resilience across three domains (neurodevelopmental, caregiver, and environment). We used structural equation modelling (SEM) to test the association between domains and ACE scores and assessed the impact on neurodevelopmental constructs. Fifty-five percent of the sample had high ACE scores (> 3), which were associated with lower attention, social skills, and emotional regulation. ACEs were strongly associated with 0.17 standard deviation units of higher levels of caregiver distress (p < .001), which was also associated with 0.26 standard deviation units of lower levels of child neurodevelopmental functioning (p = .001). For each unit increase in housing instability, there was a three-fourths increase in ACE (0.78 ACE at p = .004); four or more moves were associated with the worst neurodevelopmental outcomes (53% of the sample). We must use an ecological, developmental lens to understand how early adversity impacts children, at what age, and in what context. Housing stability plays a critical role in developmental well-being and should be accounted for in conceptualizations of child ACE scales. Caregiver and child relationships are reciprocal, and so the impacts of ACEs are also bidirectional. Our policies and practices at individual, community, and systemic levels should account for these dynamics to improve child well-being.
Similar content being viewed by others
Young children develop at an extraordinary pace, building brain circuitry that lays the foundation for the rest of their lives (Schore, 2001). At every point, they are influenced by caregivers and their environment. Ideally, warm, responsive, and engaging caregivers buffer stress and children live in an environment that is safe, supportive, and developmentally nourishing. However, when these conditions are not met, children’s experiences of stress and trauma may negatively impact developmental well-being (Center on the Developing Child at Harvard University, 2015). Adverse childhood experiences (ACEs), particularly those that occur during sensitive periods of development, can lead to developmental delay. At extreme levels, for example, when children are exposed to six or more risk factors, the chance that they will have a developmental delay is 90% (Center on the Developing Child at Harvard University, n.d.).
One way of supporting children and their caregivers is to routinely screen for risk and protective factors, including the presence of ACEs. Early detection of ACEs coupled with timely intervention can reduce the negative sequelae of events across the lifespan (Dube et al., 2001a). Routine screening for ACEs and the provision of treatment to the child and other household members have been suggested, along with assessment of other risk exposures known to be strongly associated with ACEs (Dong et al., 2004). As Chapman et al., (2007) noted in their review of ACEs and mental health, “adverse childhood events are a set of modifiable risk factors and intervening to reduce these risk factors may have far-reaching implications in terms of mental health promotion and mental illness prevention” (p. 360).
The increased awareness of ACEs among direct service providers has led to many researchers noting the limitations of using an individual’s ACE score, in the absence of other factors, as an individual measure of health outcomes for adults (Ford et al., 2019) as it may misclassify risk and lead to mismatches in service need (Anda et al., 2020). Despite this concern, the ACE study has “raised awareness of the childhood origins of public health problems for policymakers and legislators” (Anda et al., 2020, p. 293). In addition, numerous studies document the potentially detrimental impact of early adversity on the developing child’s neurophysiology. Stress reactivity, emotion regulation, and cognitive function are all subject to impact leading to maladaptive developmental trajectories that can be extend into adolescence, and, in some cases, adulthood (Kerker et al., 2015; Nelson & Gabard-Durnam, 2020; Richards & Wadsworth, 2004; Shonkoff 2012; Tottenham, 2020). Shonkoff (2016) contends that “abundant evidence also indicates that the longer we wait to intervene the more difficult it becomes to achieve healthy outcomes” (p. 1003).
Research on the exact pathways and mechanisms of how adversity during childhood impacts outcomes throughout the lifespan is constantly emerging, revealing strong associations of the lasting effects on adult health and functioning (McGinnis et al., 2022; Miller et al., 2011). In their comprehensive review of why and how early adversity influences development, Ellis et al. (2022) discuss how threat (early experiences of violence, harm, unpredictability) and/or early deprivation within the caregiving system or child’s environment differentially impacts the developing brain structurally and functionally. They attempt to move the research beyond thinking of risk as merely cumulative (as with the original use of the ACE scale) and towards a more integrated, contextualized understanding of the associations between types of risk and impact on the developing child. Such an integrated model would necessarily take into account risk factors to the child across various domains, including the caregiving system and the larger community and cultural context in which the family is embedded. Similarly, Shonkoff (2016) explains that while ACEs “quantify risk (but not diagnosis) or later health problems,” identifying early adversity and the mechanistic links to impairment for the child is essential to “construct an integrated approach to the prevention and management of stress-related disorders beginning in the earliest years” (p. 1004).
We agree with these scholars and purport that the use of newly developed ACE scales for children is not the same as the original scale’s retrospective use with adults. With adults, we look back at cumulative risk and use population-based algorithms to identify public health level associations between early stress and later disease. With children, we look forward at the associations and mechanisms that impact ongoing development. With children, its use is clearly different and has the potential to increase providers’ understanding of children’s needs and identify early risks to development (Cibralic et al., 2022; Cronholm et al., 2015; Finklehor et al., 2013) allowing for a more holistic approach. Focused intervention on mediating variables across a child’s ecology, if targeted, might right a developmental trajectory gone askew.
In the current study, we utilized a modified version of a child ACE scale and examined its associations with other variables (e.g., housing and caregiver distress). We created an algorithm that analyzes the associations of individual risk factors to the child defined as early childhood ACEs with the child’s neurodevelopmental status, as well as associations between child developmental functioning and caregiver mental health and broader living conditions.
We are not the first to use ACEs with children in this way. ACEs and their association to outcomes for young children have been assessed previously by several researchers (Bernard et al., 2022; Blodgett, 2012; Kerker et al., 2015; Marie-Mitchell & O’Connor, 2013; Ports et al., 2021). For example, using data from the National Survey of Child and Adolescent Wellbeing II gathered from 2008 to 2009, ACEs experienced before age 5 were found to have short-term effects on the functioning of young children, specifically the social-emotional health of preschoolers (Kerker et al., 2015). McKelvey et al., (2017a, 2017b) examined associations between childhood ACEs for children ages birth to age 5 in a home visiting context and found strong associations between an ACE score of 4 or more for the child and risk for developmental delay. These studies identify the immediate impact of ACEs on certain aspects of a young child’s development and advocate early identification and remediation to not only improve outcomes for the child, but which may lead to better longer term health outcomes.
Other studies have examined the associations between childhood ACEs and other factors including ACEs for the parent, socioeconomic status (SES), and race. In a retrospective study of adolescents, Ports et al., (2021) reported positive associations between maternal and child ACE reported to have occurred at age 5 and worse outcomes in adolescence. The relationship is not simple. They found that socioeconomic status and home ownership moderated these impacts variably across racial groups during the earliest years of life. For Black families in particular, SES and homeownership significantly reduced the intergenerational cycle of ACEs. Home ownership weakened the strength of this relationship, but for Black mother–child dyads only. Wealth was protective for Blacks and Hispanics; neither factor was protective for White children. Thus, discussions of ACE for young children cannot be viewed in isolation from the family context or larger sociocultural and economic conditions of their lives. The consequences of poverty and racial discrimination—less wealth accumulation, lower home ownership most notably for Black families—appear to alter how early adversities impact the child. These researchers contend that a study of ACEs must include examining the relationship between economic position, race, and adversity, and that the experience of discrimination for Black families is unique, exerting a particularly potent influence on child development. For this group, even housing stability through affordable rental housing may be beneficial.
Measuring ACE in childhood enables us to see how children are being affected as they are developing and to identify ways across the child-family-environmental systems to mitigate the impact. However, exactly how to modify the traditional scale for young children, what it should include, and how it can be used in practice are still open for debate. For young children, notably those under age 6, the scale first requires modification to be used as a parent report tool. Next, research must help to determine which risk factors are most relevant—and to date, there is no consensus on child ACE items. For example, one tool piloted in 2013 by Marie-Mitchell and Connor used a six- and seven-item child ACE scale to capture early adversities such as domestic violence, suspected maltreatment, and substance use, mental illness, criminal behavior, and single parenthood for the caregivers. They identified specific outcomes consistent with other studies between higher child ACEs and developmental delays and behavior problems in a sample of children ages 4–5. Blodget & Lanigan (2018) modified the scale for use with children in a public elementary school, replacing child maltreatment questions with ones about involvement in child welfare. In another study (Blodgett, 2012), they modified the original ACE scale to include questions about child welfare and homelessness among children ages 3–5 whose families were involved in a federal Safe Start initiative. Here, caregiver and child ACE scores were moderately correlated (r = 0.30, p < 0.05) and child ACE scores were associated with increases in developmental risk as measured by the Devereux Early Childhood Assessment (DECA) tool. The specific impact of homelessness on child outcomes was not investigated.
Concerns about the use of ACE notwithstanding and acknowledging that the evidence base for is still being built (Cibralic et al., 2022), these studies and the science of child development challenge the notion that ACE scores should never be used for individual assessment. At least for young children, the impacts appear to be immediate, moderated by a variety of sociocultural factors, embedded within the caregiving system, and amenable to intervention if identified. This paper describes our effort to modify the traditional ACE scale and create a version that can be used individually with children ages 3–5 living in poverty and experiencing housing instability. Routine, developmentally grounded, ecologically based screening is particularly salient for children from low-income populations, where ACEs are typically higher than in the general population (Kerns et al., 2017; Wade et al., 2016). While 25% of the general population experience two or more ACEs and 12% experience four or more (Felitti et al., 1998), children who live below the Federal Poverty Line (FPL) are five times more likely to experience four or more ACEs (Halfon et al., 2017). Early identification of risk is critical; without it, the impacts of exposure to adversity are far more difficult to mitigate (Center on the Developing Child, 2007).
From 2017 to 2020, we endeavored to create an online ecological screening tool for use by paraprofessionals, wherein they could work with caregivers to screen young children living in low-resource environments for risk and resilience factors across three domains of well-being: neurodevelopment, caregiver well-being, and environment. These efforts were funded by the National Institute of Health and Human Development (NICHD) and have been described in several publications (DeCandia et al., 2020, 2021). As part of this project, we embedded our modified version of the ACE scale. In this paper, we first briefly review the ACE scale literature relevant to the ways that we adapted the scale for its use within the tool we created. We then describe our method of modifying the scale to include housing instability and report the results of a series of the analyses we conducted to ascertain how these modified ACE items related to the children’s developmental risk.
Literature Review
From Retrospective Adult Screening to Proactive Child ACE Screening
As originally conceptualized, the ACE scale (a 10-question-item list with yes/no answers) is to be completed by an adult (age 18 +), answering retrospectively about their life experiences (Felitti et al., 1998). Items are categorized into subtypes that include childhood maltreatment (abuse—physical, emotional/verbal, sexual; neglect—physical/emotional) and family/household dysfunction (parental divorce/separation; domestic violence; substance use; mental illness; caregiver incarceration). Research on exposure to ACEs has illuminated the impact of trauma across the lifespan and across myriad areas of well-being—exploring everything from smoking, severe obesity, and physical inactivity to depressed mood and suicide attempts (Felitti et al., 1998). Researchers concluded that the “impact of these adverse childhood experiences on adult health status is strong and cumulative” (Felitti et al., 1998, p. 251). These findings have been replicated across dozens of studies (e.g., Dietz et al., 1999; Dube et al., 2001a; Dube et al., 2001b; Giano et al., 2020; Hughes et al., 2017; Weiss & Wagner, 1998).
While this retrospective adult-focused model is quite helpful in some contexts, there is a growing movement to address ACEs earlier and preventatively (Narayan et al., 2021), thereby determining ways to buffer the impact of ACEs already accumulated and reduce the risk of further exposure. One step in this process is develop consensus around which items should be included in a child ACE scale. Many of these efforts have focused on expanding the traditional ACE items to include a more ecological focus. For example, Cronholm and colleagues (2015) examined “conventional ACE” versus “expanded ACE” and learned that 14% of adverse experiences would have gone unrecognized by the conventional model. These included community violence, racial discrimination, feeling that the neighborhood was unsafe, bullying, and foster care. Using the same data set,
Lê-Scherban (2018) and colleagues noted that there are intergenerational associations between parent ACE and worse child health, health behaviors, and health care use/access. Researchers concluded that “conventional ACE score may fail to capture the full spectrum of relevant childhood adversities” (LeSherban, 2018, p. 6).
In conceptualizing the ACEs embedded in our ecological screening tool (see DeCandia et al., 2020, 2021), we sought to investigate the difference in developmental well-being when housing instability was accounted for as part of a modified ACE scale, building on the work described by previous ACE researchers and practitioners (Cronholm et al., 2015; Finkelhor et al., 2013; Lê-Scherban et al., 2018; Sacks et al., 2014). Additionally, we were interested in young children (ages 3–5) in particular. Newer research highlights the importance of also investigating the timing of ACE in a child’s development and the outcome. For example, Hambrick et al., (2019a, b) identified the perinatal time period as the most significant developmental period when health outcomes are adversely impacted by experiences of early impoverishment and neglect. Although children are affected at all times in their lives, it is the perinatal period where the impact seems to be the greatest. Hambrick et al., (2019a, b) found the strongest associations between early life adversity and worse neurocognitive development, relational health, and self-regulatory capacities of children ages 8–10 years old, with variations noted in when the stress occurred and which factor was most impacted. They conclude that stress in early childhood was associated with more neurocognitive difficulties, and stress in later childhood was associated with more relational difficulties. For children, the timing of when ACE occur is as important as how many and which ones are experienced.
Housing Instability and Developmental Impact
One stressor that is known to detrimentally impact young children’s development is housing insecurity (Cutts et al., 2011). This involves conditions such as overcrowding and multiple moves. Other housing factors typically examined include housing quality which is associated with poorer mental health (Rollings et al., 2017). Sandel and colleagues (2017) noted that housing instability defined as inability to pay rent, frequent moves, and outright homelessness all had a significant impact on caregiving adults but also on the well-being of the children such that the more adverse housing experiences a family had, the greater the odds of maternal depression, poor child health, and increased hospitalizations. Despite this, housing and homelessness are not routinely included in health screening tools. Only as the health industry begins to address the social determinants of health (SDOH) is housing instability being included in screeners for adult health issues (Chhabra et al., 2019). We have yet to see housing questions in any child development screeners (see DeCandia et al., 2020 wherein we include a review of specific tools), nor are we are of any ACE scales for children that incorporate question about housing stability. This presents a significant gap in the scientific literature among childhood ACEs. Also, critical to acknowledge is the role of racism and discrimination: For children of color living in poverty, the impact of ACEs for the child and caregiver is more pronounced and requires not just individualized but broader social-ecological interventions (e.g., affordable housing) to effectively buffer the impact (Ports et al., 2021).
Episodes of homelessness often punctuate years of housing instability (Gultekin & Brush, 2017; Hayes et al., 2013). The typical family experiencing homelessness in the USA consists of a mother and her two young children (Bassuk & Beardslee, 2014; Weinreb et al. 2006). These families move frequently—on average four times in the 2 years prior to entering shelter (Hayes et al., 2013). Even after leaving a housing program, the majority tend to remain highly mobile. In one study, 63% of families moved at least once following shelter discharge, mainly due to poor living conditions or being unable to pay rent (Collins et al., 2019). These results are similar to those reported by (Hayes et al. (2013), which indicates that 63% and 49% of families were residentially unstable at 15 and 30 months post placement, respectively. In addition, as more than one-third of children who are homeless have been involved in a child protection investigation (Guarino & Bassuk, 2010), the chances of experiencing out-of-home placement are exacerbated for some.
Housing insecurity impacts the social fabric of the family as supports are frayed (Pinderhughes et al., 2001). Women who experienced high housing mobility and episodes of homelessness also report high rates of childhood and later adult trauma, broken family relationships, and social isolation. They experience multiple system failures across the educational, housing, and state safety networks that contributed to these unstable living situations (Gultekin & Brush, 2017). The impact on the very young can be profound. In one study, instability—defined rather conservatively for children as having moved two or more times in a year—was associated with worse caregiver health (notably maternal depression) and in some cases higher rates of food insecurity. These factors were strongly associated with poor child health and increased developmental risk (Pinderhughes et al., 2001).
As one would expect, children living in stressful conditions experienced increased health and well-being risks due to the COVID-19 pandemic. As supports and resources to address the housing and food insecurity were less available, confusion and disruptions in homeless services amassed (Shi et al., 2020). Families and children experiencing homelessness saw increases in social isolation, domestic violence, and risk for maltreatment (Silliman Cohen & Bosk, 2020) exacerbating already poorer health and developmental outcomes (Coughlin et al., 2020). Societal inequities in the ability to safely work and receive support seen between lower and higher income groups and racial minorities and Whites (Ray & Rojas, 2020) were also magnified by the pandemic. The cost to vulnerable and housing insecure children is still being assessed.
Several researchers have demonstrated that issues of race, poverty, economics, and geographical location are intertwined with early adversity for young children. They argue, and we agree, that ACEs must be culturally contextualized to understand the relative impact for different racial and ethnic groups, of different socioeconomic classes, in different locales (Bernard et al., 2021; Bruner, 2017). While we must understand the mechanisms underlying the developmental impact to help individual children, we must also situate the etiology of adversity outside the individual to effectively target interventions that address underlying inequities. Housing inequity and other forms of structural racism have been linked to poorer outcomes for children and adults. Individual interventions such as early childhood interventions and parenting supports are needed to mediate the individual impacts and enrich the lives of developing the child; so too are community-level interventions to account for differential impacts across racial groups borne from deeply embedded cultural and systemic discriminatory practices and policies (Shonkoff, 2016). Racial discrimination acts like a conventional ACE for Black children and is associated with worse mental health outcomes (Bernard et al., 2022), even after controlling for conventional forms of child abuse and neglect (Mendez et al., 2022). When this conceptualization is applied to a screening tool, at minimum, an ecological frame, inclusive of culturally specific child ACEs such as housing instability, is essential to identify interventions at multiple levels—child, caregiver, and environment—that can improve developmental trajectories for young children.
Intergenerational Approach
In addition to external forces and SDOH on developmental outcomes, caregiver well-being is also an important factor that can mediate the impact. Caregivers can serve as critical buffers for children, mitigating the impact of stress in ways that is protective to their development (Center on the Developing Child at Harvard University, 2009; Herbers et al., 2011; National Research Council & the Institute of Medicine, 2009a; 2009b). However, caregivers may come to the family system with their own history of trauma, which in turn may affect risk and resilience processes over the course of their lives as parents (Narayan et al., 2021).
Research indicates that parents with greater exposure to ACEs are more likely to have children with behavioral health problems (Schickendanz, 2018). Caregiver well-being (e.g., parental depression) and poor parenting both negatively influence a child’s social-emotional development; for very young children, the higher the number of ACE for the mother, the more developmental challenges across domains faced by the child (Folger et al., 2018). So why do so many kids fare well despite early adversity? Positive, responsive, supportive parenting can mediate the impact of stress on children, leading to more resilient outcomes (National Research Council & Institute of Medicine, 2009b; Perlman et al., 2012). However, many parents struggling with multiple adversities are simply too depleted to buffer the impact. Healthy nutrition, sleep, and exercise are critical for good health (Lopresti et al., 2013; Walsh, 2011) but are difficult for parents to obtain when living without resources or moving between shelters, motels, and overcrowded situations with family or friends.
The well-being of children’s primary caregivers is critical to understanding the risk and protective factors that contribute to developmental well-being. There is a direct relationship between parenting stress and ACEs among adults from low SES groups (Borja et al., 2019; Moe et al., 2018; Steele et al., 2016), leading many to recommend ACE screening for new parents to minimize intergenerational transmission through problematic parenting practices (Steele et al., 2016). However, as Borja et al. (2019) discuss, high parental ACE exposure may not continue into adulthood, suggesting “the resilience of some parents who, despite their exposure to ACEs, can prevent the heightened exposure of their children to adversities” (p. 264). We join the movement for an intersectional, resilience-based view of children’s development.
Method
To specifically investigate young children’s exposure to adverse events, we used two different conceptualizations of ACE: the first is a modified version of Blodgett’s ACE scale (2012) and the second includes the addition of items focusing on homelessness and residential instability. Specifically, we ask the following questions:
-
1.
For young children living in poverty, to what extent does exposure to ACEs inform their risk for developmental delay?
-
2.
How, if at all, does the chronicity of residential instability during early childhood contribute to how we conceptualize ACEs?
-
3.
To what extent does caregiver well-being mediate the impacts of child ACE exposure, including residential instability?
We hypothesized that among the children in our sample, the higher the ACE score, the greater the risk for developmental delay. Conversely, an ACE score that is low (e.g., 1 or 0) will be more prevalent among children developing according to typical trajectories. We predicted that expanding the child ACE score to include residential instability would increase the likelihood of developmental risk and that children who have higher rates of residential instability will be at more risk than those who have less frequent moves. Finally, we hypothesized that caregiver well-being will serve as a protective factor, mediating the impact of child ACEs and residential instability on developmental well-being. We conclude with a discussion of these findings, focusing especially on the value, utility, and potential consequences of the use of ACE screening as a part of a developmental risk assessment for children.
Sample
The sample for this study consisted of 231 children ages 3 to 5. All were either homeless or recently housed (in the 30 days prior) during data collection. To qualify for participation in the study, the inclusion criteria for caregivers were as follows: receiving services through a program serving homeless families and working with a case manager or program staff; ability to speak English and read at the 6th grade level; have at least one child ages 3 to 5; have the cognitive capacity and willingness to be consented (see informed consent process below); and willingness to participate in study activities. Caregivers who did not meet these criteria were excluded from the study.
Children were nearly evenly split among gender (52% male, 48% female) and age (28% age 5, 31% age 4, and 41% age 3). The caregivers completing the survey were primarily mothers (93%), but some fathers (5%) and other caregivers (2%) also participated. Eighty-four percent of the children and 79% of the caregivers were non-White. Children’s race and ethnicity were distributed as follows: 43% African American, 16% White, 5% Other, 2% Native American, 2% Hawaiian. Thirty-one percent of participating caregivers identified their child as Hispanic. The caregiver breakdown was similar: 50% African American, 21% White, 20% Hispanic, 4% Other, 2% Native American, and 2% Hawaiian. These data are summarized in Table 1.
The sample was recruited from nine organizations in seven US states, all of which served homeless families. Participating programs had to meet the following inclusion criteria: be a program serving homeless children and families; have paraprofessional, non-clinically trained staff (e.g., case managers) willing to administer the instrument to caregivers of children ages 3 to 5; provide access to computers and the Internet for completing the instrument with caregivers; and be willing to support recruitment (distribute recruitment flyers and help to identify participants). Sites were located in California, Illinois, Massachusetts, North Carolina, Texas, Utah, and Virginia.
Data Collection
After completing informed consent with a trained member of the study staff, the child’s caregiver was guided by a case manager through the Neurodevelopmental Ecological Screening Tool (NEST), an online screening tool consisting of 105 multiple-choice questions across three domains (neurodevelopmental, caregiver, and environment). Children did not answer any questions directly; all data were collected from caregivers and NEST was administered by case managers.
Measures
The data for this study come from the validation of the Neurodevelopmental Ecological Screening Tool (NEST). NEST consists of items related to risk and protective factors most relevant to the developmental trajectories of children experiencing poverty (Buckner et al., 2009; Center on the Developing Child at Harvard University, 2007, 2009, 2015; Gerhardt, 2004; Ginsburg, 2007; National Research Council and Institute of Medicine, 2000, 2009b; Shonkoff & Meisels, 2000). It is designed to screen children for developmental risk and resilience across three domains and 13 constructs. The neurodevelopmental domain’s five constructs include motor skills, functional communication, neurocognitive executive functions, adaptability and coping, and social-emotional functioning, and each of these five constructs is comprised of sub-constructs. The caregiver domain is comprised of three constructs: depression (as measured by the Patient Health Questionnaire-9 [PHQ-9]; see Kroenke and Spitzer, 2002), post-traumatic stress disorder (PTSD) symptomology (as measured by the PCL-5; see Weathers et al., 2013), and overreactive parenting (as measured by five items on The Parenting Scale; see Arnold et al., 1993). The environment domain is comprised of five constructs: child ACE, residential instability/homelessness, health care access, food security, and lead exposure. See Fig. 1 for a visual summary. The tool is psychometrically validated and can detect clinically significant developmental delays among young children experiencing homelessness (DeCandia et al., 2021).
Modification of the ACE Scale for NEST
Embedded in NEST is a modified ACE scale (“NEST ACE”) which includes nine items; we modified the scale that Blodgett (2012) used by eliminating one item—housing/homelessness—in favor of more detailed questions on the same topic elsewhere in NEST. We then conceptualized an “Expanded NEST ACE” scale, which adds residential instability to the list of items on the NEST ACE (see Table 2).
Data Analysis
To begin our analyses, we used the framework presented in Fig. 1 to estimate the association between NEST ACE scores and neurodevelopmental domain scores. We then examined residential instability and its relationship to NEST ACE. Finally, we selected sub-constructs that had an association with ACE scores and then estimated a structural equation model (SEM) to test the association of between the caregiver domain, the neurodevelopmental domain, and ACE scores, adjusting for race, ethnicity, age, and gender or relation to the child. The SEM model was estimated using full information maximum likelihood (FIML) to account for missing data. To analyze our data, we used Stata 15.1.
Results
Research Question #1: For Young Children Living in Poverty, to What Extent Does Exposure to ACEs Inform Their Risk for Developmental Delay?
Our first research question pertained to understanding the ACE scores among young children and how they relate to risk for developmental delay. We had complete NEST ACE data for 200 study participants. Of that group, the mean ACE for our sample was 2.57. Forty-five percent of the children in our sample had a NEST ACE of three or more. To conduct a more detailed analysis, we categorized responses based on number of ACEs: none, low, high, and severe. The caregivers of 18.5% (37 children) of our sample reported “none” for the NEST ACE measure. We considered one or two ACEs as “low,” a category into which 36% (72 children) of our sample fell. An ACE of 3, 4, or 5 was considered “high”; 36.5% of our sample (73 children) fell here. Nine percent (18 children) were categorized as “severe,” with ACEs of six or more. These data are summarized in Table 3.
The neurodevelopmental domain of NEST includes fine/gross motor skills, functional communication, neurocognitive executive functions (e.g., attention, problem-solving), adaptability and coping, and social-emotional functioning. Higher scores in this domain are associated with better functioning in the area (e.g., a higher communication score is associated with higher functional communication skills). Scores are age-graded in 6-month intervals to account for developmental growth. Using OLS regressions with ACE scores as the dependent variable, we separately tested each of the sub-constructs mentioned in Fig. 2. Our analyses indicate that higher ACE scores were associated with lower attention, social skills, and emotional regulation. Communication, cognitive processing, and problem-solving were not associated with ACEs in our model. See Table 4.
Research Question #2: How, if at all, Does the Chronicity of Residential Instability During Early Childhood Contribute to How We Conceptualize ACEs?
For the children in our sample, their NEST ACE score was high even without the enumeration of residential instability/homelessness (see Tables 2 and 4). To explore further the impact of exposure to adverse experiences on young children, we conceptualized an Expanded NEST ACE model, adding residential instability to the list outlined in NEST ACE (see Table 2). All children in our sample were either currently homeless or had recently moved to permanent housing at the time of our study. With this as a baseline, we sought to explore the chronicity of residential instability. To do so, we asked the following question: How many times has your child moved in their lifetime? Choices were as follows: never/once; 2–3 times; 4–5 times; 6 + times. Of the 225 children for whom we had data to this question, 7% had never moved. Approximately 40% had moved two to three times, while 32% had moved four to five times, and 21% had moved more than six times. In other words, over half (53%) of the sample had moved four times or more.
Given these findings, we then investigated the connection between housing instability and ACE scores. A bivariate regression model indicated that each unit increase in housing instability is associated with an increase of three-fourths of an ACE (0.78 ACE at p = 0.004). Because of this strong association, we were interested in creating more differentiation to see if it shed any light on the phenomena. To do so, we conceptualized a dichotomized version of the NEST ACE scale, wherein ACEs of 4 or 5 were assigned a value of 1 (4 + ACES = 1) of the housing instability question into the NEST ACE. Adding the dichotomized residential instability question identified 14 individuals (7%) that had a 0 ACE score (0–3 moves), increasing differentiation of distress at the lower end of the ACE. Thus, we are able to see the relative impact of zero to three moves on a subset of the sample as compared to those who moved four or more times, more than four moves being associated with worse neurocognitive domain scores.
Research Question #3: To What Extent Does Caregiver Well-being Mediate the Impacts of Child ACE Exposure, Including Residential Instability?
We measured caregiver well-being across three constructs known to impact the well-being of young children that are also highly prevalent among families living in poverty: parental depression (Bassuk & Beardslee, 2014), trauma symptomology (Hayes et al., 2013), and authoritarian parenting styles, which are characterized by overreactive parenting behaviors and low responsiveness to the child’s needs (Baumrind, 1966; Steele et al., 2005). More than half (51%) of our sample reported some level of parental depression. Of that group, 30% scored positive for mild depression, 8% moderate, 10% moderate severe, and 3% severe. Thirty-five percent of the sample reported significant post-traumatic stress symptoms and reached the cutoff threshold to be considered at-risk for post-traumatic stress disorder (PTSD). Symptom expression included intrusive thoughts (35%), high levels of upset when reminded of stressful experiences (36%), feelings of isolation (30%), avoidance (27%), irritability (22%), and difficulty concentrating (23%). Finally, most parents (58%) reported a non-overreactive parenting style. Depression, trauma exposure, and overreactive parenting were all moderately associated with ACEs (see Table 4).
SEM Mediation Model
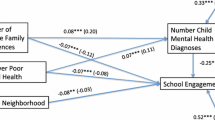
The broad conceptual model of NEST argues that environment and caregiving have a direct effect on children’s neurodevelopment. Furthermore, it is predicated on the understanding that the effect of the environment also impacts children through the effect of the environment on their caregiver. For the SEM mediation model, this hypothesis is tested by modeling the effects of ACE scores on children’s functioning both through direct paths and mediated through caregiver scores. Figure 2 shows the estimated model and Table 5 shows the results from the model. As shown in the model, ACE scores were regressed on the neurodevelopmental and caregiver domains. On the neurodevelopmental domain, we adjusted for race, gender and age; on the caregiver domain, we adjusted for age, race, and caregiver status.
Table 5 shows the model fits the data with RMSEA scores below 0.05 and CFI/TLI scores above 0.95. The coefficient of determination suggests that the model accounts for 40% of the variance in the data. The findings of the SEM model support the hypothesis that ACE scores affect children’s neurodevelopmental risk and that approximately half of the effect is direct (60%), and half the effect is mediated through the caregiver domain (40%).
ACEs were associated with 0.17 standard deviation units of higher levels of caregiver distress (p < 0.001), and higher levels of caregiver distress were associated with 0.26 standard deviation units of lower levels of child neurodevelopmental functioning (p = 0.001). Girls and older children tended to demonstrate overall higher levels of neurodevelopmental functioning.
Our main hypothesis was that ACEs will affect child neurodevelopmental functioning both directly and through the caregiver. We found evidence to support this hypothesis. Half of the effect of ACE on child scores is direct but was not statistically significant. However, the combination of the direct effect of ACEs on the child domain (Fig. 2 Path C) and the indirect effect of ACEs through the caregiver domain (Fig. 2 Paths A + B) was associated with a 0.10 standard deviation unit lower neurodevelopmental domain score.
Discussion
Retrospective studies clearly document the significant and potentially lifelong impact that adverse childhood experiences exert on human development; the impact of ACE experienced in childhood on the child as they are developing is less clear. Also less well known is how the impacts of ACEs in children are related to the well-being of their caregivers, or to what extent sociocultural factors (e.g., racism) act as ACEs in a child’s life. It is clear that Black children have a different level of exposure to a variety of ACEs than their White counterparts, and that supportive environmental factors (e.g., safe neighborhoods, reduced parental incarceration, safe schools and places to play) reduce the potency of the adversity experienced early in life (Melton-Fant, 2019). There are many ways to interrupt potential negative developmental trajectories. As ACES occur at all levels—individual, family, community, cultural—preventing and mitigating ACEs must take a multilevel approach as well.
Our findings will be discussed with respect to the three questions posed by this study: (1) rates of ACEs among low-income children experiencing homelessness and the associated risk of developmental delay; (2) appropriateness of considering residential instability as an ACE for young children; and (3) the impact of ACE on child functioning as a function of their caregiver’s well-being. Our examination of residential instability and exposure to adverse childhood experiences confirmed—in some cases dramatically—the deep, multi-directional relationship of the child to their caregiver and environment. We discuss our findings in relationship to research, practice, and policy.
Rates of ACE Among Homeless Children
First, we identified the high number of ACEs already experienced by young children experiencing homelessness, with nearly half (45.5%) already experiencing three or more ACE in their young lives. Although slightly more than half had low scores, the fact that so many were already at a high risk for poorer health outcomes based on cumulation of experience alone was alarming.
Practitioners, researchers, and policymakers are interested in the impact of ACE on adults and children alike. Felitti et al. (1998) original Kaiser Permanente study utilized subjects that were mostly White, middle or upper class, and with college educations. Even among this more resourced group, ACEs were found to be more common than anticipated; a quarter of respondents experienced two or more ACEs. The accumulation of ACE beyond three for adults is associated with a myriad of poor health outcomes. Since the original study, some researchers have explored the prevalence and impact of ACE in other subgroups; younger children are of particular interest due to the impact of stress on brain development. The brain evolves from building basic neural networks to gradually integrating more complex systems related to the prefrontal cortex and limbic system; exposure to adversity early in this process results in increased risk for a broad range of developmental difficulties often disrupting self-regulatory capacities, the bedrock of resilience (Bick & Nelson, 2016; Buckner et al., 2009).
For children living in poverty, the effect may be compounded. Poverty and ACEs tend to co-occur; the impacts are often intergenerational. Structural inequities in our culture embedded in institutions, policies, and practices impact what individuals can access (e.g., housing, jobs) and, consequently, how well they are able to thrive. For example, ACEs in childhood can lead to difficulties with education and employment in adulthood (Metzler et al., 2017). Our sample confirmed that the rates of ACE for young children living below the poverty line are higher than for the general population. For this group of children, who were also primarily children of color experiencing homelessness, 45% had already experienced three or more conventional ACEs; 9% reported six or more. By comparison, national figures estimate that 35% of all children (17 or younger) have experienced one or two ACEs and 11% of all US children have experienced three or more ACEs (Sacks et al., 2014). Families make up a third of the total homeless population and these numbers are likely to rise as a result of the pandemic. These same families are disproportionately Black and Hispanic. The majority of children in these families are under age 6 (Yamashiro & McLaughlin, 2021). That we know that racial discrimination in all its forms negatively impacts communities and individuals and that almost half of these young children are already experiencing early adversities putting them at risk for serious developmental challenges should focus policymakers and practitioners alike to provide more intensive support for this population.
NEST’s ecological framework points towards multilevel solutions. Individually, children found to be at-risk can be seen by child development counselors and specialists. At the caregiver level, parents struggling with depression can be identified for intervention to reduce parental stress and/or provide parent skills training and support. Structurally, at community and societal levels, policies can direct funding to high need groups to increase eligibility and access to effective home visiting support, high-quality early education and care programs, safe communities, and affordable/accessible health care, to name a few. Individual and programmatic approaches to intervention, while necessary for the individual, are not enough. By conceptualizing structural inequities and racism as underlying the adversities experienced, and by extending the ACE framework to incorporate the disproportionate influence ACEs have on children of color (Galán,et al., 2022), funding and intervention must specifically address environmental factors by improving schools, neighborhoods, and access to affordable housing.
Defining Housing as an ACE for Young Children
The second major finding is that the chronicity of housing instability was quite high for over half the families involved in the study; 53% had moved more than four times. Our analysis identified that for each move the family makes, the child’s ACE score increases by three-fourths. Thus, a young child with a low ACE score of 2 may not be thought as at-risk developmentally. But, when residential instability is factored in, that same child who moved four times actually has an ACE score of 5 and is now in the higher risk group.
This finding is highly significant and evolves our understanding of housing and child development a step further. The inclusion of residential instability is an important construct to include in any ACE scale for young children. As a field, we are likely underestimating the impact of ACE on their development if we do not inquire about housing status. The results of this study suggest that we begin by defining residential instability as four or more moves for preschool children. That number may be different for younger or older children as the impact of ACEs on children appears to be affected by their stage of development and by the timing of ACE experiences (McKelvey et al., 2017a, 2017b). More research is needed in this area.
Housing cannot be considered just an adult issue. Among young children of preschool age who experience homelessness and instability, far too many are already at-risk from more “standard” ACE. If we stop there, however, the picture is incomplete and our attempt to identify and service those most in need misses the mark. In short, housing instability and poverty are an ACE for young children, especially children of color (Ports et al., 2021)—one that significantly increases their developmental risk. Our data are among the first to document that multiple moves for a child increase their ACE score, which impacts the child’s development across domains directly and indirectly through their caregiver. As our sample was purposely restrictive to families in shelter, we cannot speak to the differential impact of SES on developmental functioning, although previous research certainly supports this concern. We hope to further validate NEST on larger, more diverse samples and hope others will seek to explore NEST with other populations as well.
As for housing, study results echo the call of others to provide families experiencing homelessness with access and services and stable, affordable housing. Furthermore, if we continue to delay making this a priority, the effects on children and families will likely be felt for generations to come. We recommend that housing instability be formally defined as an ACE in any scales for young children. This may be most relevant for very low-income groups who are highly mobile, but as we did not have a high-income comparison group, we cannot say for certain, so inclusion in any ACE scale across all young child groups is recommended at this time. More research is needed into the relationship between housing as an ACE for children at different stages of development.
Caregiver Well-being: a Portal for the Impact of Child ACE
Our third finding was not necessarily new or unexpected. ACEs for children were strongly associated with higher levels of caregiver distress, and higher levels of caregiver distress (depression and post-trauma symptoms), which in turn was associated with lower levels of child neurodevelopmental functioning. Girls and older children tended to demonstrate overall higher levels of neurodevelopmental functioning, which is also in line with the literature. This finding validates a well-known understanding—that caring for the parents is essential to ensure the health of the child. The interactive nature of the caregiver-child relationship is highlighted by this finding. However, the impact is not solely on the child. Caregivers are also impacted when their child is hurt or suffering, which in turn impacts the child. The reciprocal nature of influence of adversity on kids and their caregivers is perhaps not unexpected, but further highlights the need to identify risks and work with the family as a whole to mediate the impact.
New Directions for Research, Practice, and Policy
Policies and practices that support stable housing not only serve a family’s immediate needs but also have positive long-term health impacts for caregivers and children (Pinderhuges et al., 2007). Primary prevention of evictions and housing disruption is, of course, the ideal; no young child should have to move repeatedly in their young lives. They need stability, predictability, and routines to support healthy development. For those already disrupted from their homes, secondary and tertiary prevention is needed to prevent further risk and intervene to mediate the impacts that have already occurred. This requires a re-envisioning of federal and local housing efforts to provide services to support caregivers as the prime mediators of adversity, and a joining of housing with early childhood policy and practice. Doing so would ensure that families with young children are stabilized quickly.
From the research perspective, understanding ACEs in both parents and children gives us more information on how we might mitigate effects and craft interventions. For the children in our study, higher ACE scores were associated with worse functioning in the areas of attention, social skills, and emotional regulation, but not in the areas of communication, cognitive processing, and problem-solving. We offer two possible explanations. First, the association between higher ACEs and social-emotional functioning is possibly an indirect effect and influenced by the caregiver’s well-being. Second, the timing of ACE in a child’s early years may differentially impact developmental outcomes. For example, one study that examined ACE exposure and screening among infants and toddlers found that cognitive, language, and motor domains were more influenced by ACEs occurring close to the time of developmental screening, whereas exposure at any period in early development had negative consequences on socioemotional functioning (McKelvey et al., 2017a, b).
This raises several questions relative to our sample. When did ACEs occur for the children screened by NEST? Is there a differential impact on aspects of child development measured by NEST? Does that impact change based on age of the child at the time of testing? We cannot answer these questions based on these data, although it appears that the younger a child is when adversity occurs, the worse the potential impact (Lanier et al., 2017). An investigation of the timing of these experiences (prenatally, infancy, early childhood) was beyond the scope of this screener. Research suggests that we need to fine tune the identification of those most at-risk and locate the developmental period in which the adversity occurred. We concur with others in the field in calling for a more dynamic and complex model of ACEs’ impact on child development, and a more developmentally nuanced ACE questionnaire for young children (Narayan et al., 2021).
Early adversity impacts development; on that the research is unchallenged. However, when considering the impact on children, the answers are not simple. We agree with colleagues that our science must evolve to contextualizing ACEs within sociocultural and economic contexts imbued with inequity and discriminatory policies and practices and account for the differential impacts across groups. The emerging evidence is compelling that, at least for children, a cumulative ACE score on its own is not enough. We must understand the associations among ACEs, caregivers, and environmental conditions, thereby identifying the various pathways and mechanisms underlying the relative impact of adversity on children from different groups. By doing so, we will be in a better position to target mediating variables (e.g., maternal depression, child self-regulatory skills) for intervention and to support moderator variables (e.g., cultural values) for improved well-being (Shonkoff, 2016). It is essential that anyone working with at-risk children applies both a developmental lens and ecological perspective in research and practice to understand how early adversity impacts children, at what age, and in what context. Adapting this framework, this study lends support for two important factors associated with worse child outcomes: housing disruption and caregiver well-being. Both are key to understanding how a child may fare developmentally. Both need to be included in any investigation of ACE during childhood; and both need to be embedded into the policies and practices of agencies and systems serving families experiencing homelessness.
Conclusion
ACE prevalence and impact during early childhood is an emerging field of research. Although our study contributes to this knowledge base, it is by no means a comprehensive review of ACE among preschool children or for homeless and low-income children. We hope others will look carefully at this high-risk population in a broader way than convention dictates. We urge researchers and practitioners to formally include residential instability in their ACE questionnaires, especially for very young children, whose development is more susceptible to various forms of instability and their caregiver’s well-being. The Expanded NEST ACE scale offers one potential avenue to do so. By situating a child’s early experience within the broad context of their lives, we can better target interventions to support children and their caregivers, and address needs in their home environments.
Data Availability
Due to the nature of this research, participants of this study did not agree for their data to be shared publicly, so supporting data is not available.
References
Anda, R. F., Porter, L. E., & Brown, D. W. (2020). Inside the adverse childhood experience score: Strengths, limitations, and misapplications. American Journal of Preventive Medicine, 59(2), 293–295.
Arnold, D. S., O’Leary, S. G., Wolff, L. S., & Acker, M. M. (1993). The Parenting Scale: A measure of dysfunctional parenting and discipline situations. Psychological Assessment, 5(2), 137–144.
Bassuk, E. L., & Beardslee, W. R. (2014). Depression in homeless mothers: Addressing an unrecognized public health issue. American Journal of Orthopsychiatry, 84(1), 73–81.
Baumrind, D. (1966). Effects of authoritative parental control on child behavior. Child Development, 37(4), 887–907.
Bernard, D. L., Calhoun, C. D., Banks, D. E., Halliday, C. A., Hughes-Halbert, C., & Danielson, C. K. (2021). Making the “C-ACE” for a culturally-informed adverse childhood experiences framework to understand the pervasive mental health impact of racism on Black youth. Journal of Child & Adolescent Trauma, 14(2), 233–247.
Bernard, D. L., Smith, Q., & Lanier, P. (2022). Racial discrimination and other adverse childhood experiences as risk factors for internalizing mental health concerns among Black youth. Journal of Traumatic Stress, 35(2), 473–483.
Bick, J., & Nelson, C. A. (2016). Early adverse experiences and the developing brain. Neuropsychopharmacology, 41(1), 177.
Blodgett, C. (2012). Adopting ACES screening and assessment in child serving systems. Unpublished manuscript, Area Health Education Center, Washington State University, Spokane, WA.
Borja, S., Nurius, P. S., Song, C., & Lengua, L. J. (2019). Adverse childhood experiences to adult adversity trends among parents: Socioeconomic, health, and developmental implications. Children and Youth Services Review, 100, 258–266.
Bruner, C. (2017). ACE, place, race, and poverty: Building hope for children. Academic Pediatrics, 17(7), S123–S129.
Buckner, J. C., Mezzacappa, E., & Beardslee, W. R. (2009). Self-regulation and its relations to adaptive functioning in low-income youths. American Journal of Orthopsychiatry, 79(1), 19–30.
Center on the Developing Child at Harvard University (2009). Maternal depression can undermine the development of young children: Working paper no. 8. Retrieved from http://www.developingchild.harvard.edu
Center on the Developing Child at Harvard University (2015). Supportive relationships and active skill-building strengthen the foundations of resilience: Working paper no. 13. Retrieved from www.developingchild.harvard.edu
Center on the Developing Child at Harvard University. (n.d.). Five numbers to remember about early childhood development. Retrieved from www.developingchild.harvard.edu
Center on the Developing Child (2007). The impact of early adversity on child development (InBrief). Retrieved from www.developingchild.harvard.edu
Chapman, D. P., Dube, S. R., & Anda, R. F. (2007). Adverse childhood events as risk factors for negative mental health outcomes. Psychiatric Annals, 37(5), 359.
Cibralic, S., Alam, M., Diaz, A. M., Woolfenden, S., Katz, I., Tzioumi, D., ... & Eapen, V. (2022). Utility of screening for adverse childhood experiences (ACE) in children and young people attending clinical and healthcare settings: A systematic review. BMJ open, 12(8), e060395
Chhabra, M., Sorrentino, A. E., Cusack, M., Dichter, M. E., Montgomery, A. E., & True, G. (2019). Screening for housing instability: Providers’ reflections on addressing a social determinant of health. Journal of General Internal Medicine., 34(7), 1213–1219.
Collins, C. C., Bai, R., Crampton, D., Fischer, R. D’Andrea, R., Dean, K., ... Cherney, E. (2019). Implementing housing first with families and young adults: Challenges and progress toward self-sufficiency. Children and Youth Services Review, 96, 34-46
Coughlin, C. G., Sandel, M., & Stewart, A. M. (2020). Homelessness, children, and COVID-19: A looming crisis. Pediatrics, 146(2).
Cronholm, P. F., Forke, C. M., Wade, R., Bair-Merritt, M. H., Davis, M., Harkins-Schwarz, M.,... Fein, J. A. (2015). Adverse childhood experiences: Expanding the concept of adversity. American Journal of Preventative Medicine, 49(3), 354-361
Cutts, D. B., Meyers, A. F., Black, M. M., Casey, P. H., Chilton, M., Cook, J. T., … Frank, D. A. (2011). US Housing insecurity and the health of very young children. American Journal of Public Health, 101(8), 1508–1514
DeCandia, C. J., Volk, K. T., Unick, G. J., Rose, L., & Donegan, W. (2020). Developing a screening tool for young children using an ecological framework. Infants and Young Children, 33(4), 237.
DeCandia, C.J., Unick, J., Volk, K., Donegan, L.R. (2021). Validating the neurodevelopmental domain of neurodevelopmental ecological screening tool: An ecological screener for use with 3-5 Year-old children impacted by poverty and homelessness. Journal of Psychoeducational Assessment, 39(5), 531–548. https://doi.org/10.1177/07342829211005575
Dietz, P. M., Spitz, A. M., Anda, R. F., Williamson, D. F., McMahon, P. M., Santelli, J. S., ...Kendrick, J. S. (1999). Unintended pregnancy among adult women exposed to abuse or household dysfunction during their childhood. JAMA, 282(14), 1359-1364
Dong, M., Anda, R. F., Felitti, V. J., et al. (2004). The interrelatedness of multiple forms of childhood abuse, neglect, and household dysfunction. Child Abuse and Neglect, 28(7), 771–784.
Dube, S. R., Anda, R. F., Felitti, V. J., Chapman, D. P., Williamson, D. F., & Giles, W. H. (2001a). Childhood abuse, household dysfunction, and the risk of attempted suicide throughout the life span: Findings from the adverse childhood experiences study. JAMA, 286(24), 3089–3096.
Dube, S. R., Anda, R. F., Felitti, V. J., Croft, J. B., Edwards, V. J., & Giles, W. H. (2001b). Growing up with parental alcohol abuse: Exposure to childhood abuse, neglect, and household dysfunction. Child Abuse and Neglect, 25(12), 1627–1640.
Ellis, B. J., Sheridan, M. A., Belsky, J., & McLaughlin, K. A. (2022). Why and how does early adversity influence development? Toward an integrated model of dimensions of environmental experience. Development and Psychopathology, 34(2), 447–471.
Felitti, V. J., Anda, R. F., Nordenberg, D., Williamson, D. F., Spitz, A. M., Edwards, V., ... & Marks, J. S. (1998). Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults: The adverse childhood experiences (ACE) study. American Journal of Preventive Medicine, 14(4), 245–258.
Finkelhor, D., Shattuck, A., Turner, H., & Hamby, S. (2013). Improving the adverse childhood experiences study scale. JAMA Pediatrics, 167(1), 70–75.
Folger, A. T., Eismann, E. A., Stephenson, N. B., Shapiro, R. A., Macaluso, M., Brownrigg, M. E., & Gillespie, R. J. (2018). Parental adverse childhood experiences and offspring development at two years of age. Pediatrics, 141(4), e20172826.
Ford, K., Hughes, K., Hardcastle, K., et al. (2019). The evidence base for routine enquiry into adverse childhood experiences: A scoping review. Child Abuse and Neglect, 91, 131–146.
Galán, C. A., Auguste, E. E., Smith, N. A., & Meza, J. I. (2022). An intersectional-contextual approach to racial trauma exposure risk and coping among Black youth. Journal of Research on Adolescence, 32(2), 583–595.
Gerhardt, S. (2004). Why love matters: How affection shapes a baby’s brain. Routledge.
Giano, Z., Wheeler, D. L., & Hubach, R. D. (2020). The frequencies and disparities of adverse childhood experiences in the U.S. BMC Public Health, 20, 1327. https://doi.org/10.1186/s12889-020-09411-z
Ginsburg, K. R. (2007). The importance of play in promoting healthy child development and maintaining strong parent-child bonds. Pediatrics, 119(1), 182–191.
Guarino, K., & Bassuk, E. L. (2010). Ending child homelessness in America. American Journal of Orthopsychiatry, 80(4), 496–504.
Gultekin, L., & Brush, B. L. (2017). In their own words: Exploring family pathways to housing instability. Journal of Family Nursing, 23(1), 90–115.
Halfon, N., Larson, K., Son, J., Lu, M., & Bethell, C. (2017). Income inequality and the differential effect of adverse childhood experiences in US children. Academic Pediatrics, 17(7S), S70-78.
Hambrick, E. P., Brawner, T. W., Perry, B. D., Brandt, K., Hofmeister, C., & Collins, J. O. (2019). Beyond the ACE score: Examining relationships between timing of developmental adversity, relational health and developmental outcomes in children. Archives of Psychiatric Nursing, 33(3), 238–247.
Hambrick, E. P., Brawner, T. W., & Perry, B. D. (2019). Timing of early-life stress and the development of brain-related capacities. Frontiers in Behavioral Neuroscience, 13, 183.
Hayes, M., Zonneville, M., & Bassuk, E. (2013). The SHIFT Study final report: Service and housing interventions for families in transition. The National Center on Family Homelessness. Newton, MA
Herbers, J. E., Cutuli, J. J., Lafavor, T. L., Vrieze, D., Leibel, C., Obradovi´c, J., & Masten, A. S. (2011). Direct and indirect effects of parenting on the academic functioning of young homeless children. Early Education & Development, 22, 77–104.
Hughes, K., Bellis, M. A., Hardcastle, K. A., Sethi, D., Butchart, A., Mikton, C., Jones, L., & Dunne, M. P. (2017). The effect of multiple adverse experiences on health: A systemic review and meta-analysis. The Lancet., 2(8), E356–E366.
Kerker, B. D., Zhang, J., Nadeem, E., Stein, R. E., Hurlburt, M. S., Heneghan, A., ... & Horwitz, S. M. (2015). Adverse childhood experiences and mental health, chronic medical conditions, and development in young children. Academic pediatrics, 15(5), 510-517
Kerns, C. M., Newschaffer, C. J., Berkowitz, S., & Lee, B. K. (2017). Examining the association of autism and adverse childhood experiences in the national survey of children’s health: The important role of income and co-occurring mental health conditions. Journal of Autism and Developmental Disorders, 47(7), 2275–2281.
Kroenke, K., & Spitzer, R. L. (2002). The PHQ-9: A new depression diagnostic and severity measure. Psychiatric Annals, 32(9), 509–515.
Lanier, P., Maguire-Jack, K., Lombardi, B., Frey, J., & Rose, R. A. (2017). Adverse childhood experiences and child health outcomes: Comparing cumulative risk and latent class approaches. Maternal and Child Health Journal, 22(3), 288–297.
Lê-Scherban, F., Wang, X., Boyle-Steed, K. H., & Pachter, L. M. (2018). Intergenerational associations of parent adverse childhood experiences and child health outcomes. Pediatrics, 141(6), e20174274.
Lopresti, A. L., Hood, S. D., & Drummond, P. D. (2013). A review of lifestyle factors that contribute to important pathways associated with major depression: Diet, sleep and exercise. Journal of Affective Disorders, 148(1), 12–27.
Marie-Mitchell, A., & O’Connor, T. G. (2013). Adverse childhood experiences: Translating knowledge into identification of children at risk for poor outcomes. Academic Pediatrics, 13(1), 14–19.
McGinnis, E. W., Sheridan, M., & Copeland, W. E. (2022). Impact of dimensions of early adversity on adult health and functioning: A 2-decade, longitudinal study. Development and Psychopathology, 1–12.
McKelvey, L. M., Selig, J. P., & Whiteside-Mansell, L. (2017a). Foundations for screening adverse childhood experiences: Exploring patterns of exposure through infancy and toddlerhood. Child Abuse and Neglect, 70, 112–121.
McKelvey, L. M., Conners Edge, N. A., Fitzgerald, S., Kraleti, S., & Whiteside-Mansell, L. (2017b). Adverse childhood experiences: Screening and health in children from birth to age 5. Families Systems & Health, 35(4), 420.
Melton-Fant, C. (2019). Childhood adversity among Black children: The role of supportive neighborhoods. Children and Youth Services Review, 105, 104419.
Mendez, L., Mozley, M. M., & Kerig, P. K. (2022). Beyond trauma exposure: Discrimination and posttraumatic stress, internalizing, and externalizing problems among detained youth. Journal of Interpersonal Violence, 37(3–4), 1825–1851. https://doi.org/10.1177/0886260520926314
Metzler, M., Merrick, M. T., Klevens, J., Ports, K., & Ford, D. C. (2017). Adverse childhood experiences and life opportunities: Shifting the narrative. Children and Youth Services Review, 72, 141–149.
Miller, G. E., Chen, E., & Parker, K. J. (2011). Psychological stress in childhood and susceptibility to the chronic diseases of aging: Moving toward a model of behavioral and biological mechanisms. Psychological Bulletin, 137(6), 959–997.
Moe, V., Von Soest, T., Fredriksen, E., Olafsen, K. S., & Smith, L. (2018). The multiple determinants of maternal parenting stress 12 months after birth: The contribution of antenatal attachment style, adverse childhood experiences, and infant temperament. Frontiers in Psychology, 9, 1987.
Narayan, A. J., Lieberman, A. F., & Masten, A. S. (2021). Intergenerational transmission and prevention of adverse childhood experiences (ACEs). Clinical Psychology Review., 85, 101997.
National Research Council and Institute of Medicine (NRC & IOM). (2009a). Depression in parents, parenting, and children: Opportunities to improve identification, treatment, and prevention. Committee on Depression, Parenting Practices, and the Healthy Development of Children. Board on Children, Youth, and Families. Division of Behavioral and Social Sciences and Education. Washington, DC: National Academies Press
National Research Council and Institute of Medicine. (2000). From neurons to neighborhoods: The science of early childhood development. Shonkoff, J. P., & Phillips, D. A. (Eds.): National Academy Press. Washington, D.C
National Research Council and Institutes of Medicine. (2009b). Preventing mental, emotional, and behavioral disorders among young people: Progress and possibilities. Committee on Prevention of Mental Disorders and Substance Abuse Among Children, Youth, and Young Adults: Research Advances and Promising Interventions. O’Connell, M.E., Boat, T., & Warner, K.E. (Eds). Board on children, youth, and families, division of behavioral and social sciences and education. Washington, DC: The National Academies Press.
Nelson, C. A., III., & Gabard-Durnam, L. J. (2020). Early adversity and critical periods: Neurodevelopmental consequences of violating the expectable environment. Trends in Neurosciences, 43(3), 133–143.
Perlman, S., Cowan, B., Gewirtz, A., Haskett, M., & Stokes, L. (2012). Promoting positive parenting in the context of homelessness. American Journal of Orthopsychiatry, 82(3), 402–412.
Pinderhughes, E. E., Nix, R., Foster, E. M., Jones, D., & Conduct Problems Prevention Research Group. (2001). Parenting in context: Impact of neighborhood poverty, residential stability, public services, social networks, and danger on parental behaviors. Journal of Marriage and Family, 63(4), 941–953.
Ports, K. A., Tang, S., Treves-Kagan, S., & Rostad, W. (2021). Breaking the cycle of adverse childhood experiences (ACEs): Economic position moderates the relationship between mother and child ACE scores among Black and Hispanic families. Children and Youth Services Review, 127, 106067.
Ray, R., & Rojas, F. (2020). Inequality during the coronavirus pandemic. Contexts: Sociology for the Public. https://contexts.org/blog/inequality-during-the-coronavirus-pandemic. Accessed 15 Oct 2022
Richards, M., & Wadsworth, M. E. J. (2004). Long term effects of early adversity on cognitive function. Archives of Disease in Childhood, 89(10), 922–927.
Rollings, K. A., Wells, N. M., Evans, G. W., Bednarz, A., & Yang, Y. (2017). Housing and neighborhood physical quality: Children’s mental health and motivation. Journal of Environmental Psychology, 50, 17–23.
Sacks, V., Murphey, D., & Moore, K. (2014). Adverse childhood experiences: National and state-level prevalence (research brief # 2014–28). Retrieved from http://www.childtrends.org/wp-content/uploads/2014/07/Brief-adverse-childhoodexperiences_FINAL.pdf
Schore, A. (2001). The effects of early relational trauma on right brain development, affect regulation, and infant mental health. Infant Mental Health Journal, 22(1–2), 201–269.
Shi, Y., Jang, H. S., Keyes, L., & Dicke, L. (2020). Nonprofit service continuity and responses in the pandemic: Disruptions, ambiguity, innovation, and challenges. Public Administration Review, 80(5), 874–879.
Shonkoff, J. P. (2012). Leveraging the biology of adversity to address the roots of disparities in health and development. Proceedings of the National Academy of Sciences, 109(supplement_2), 17302–17307.
Shonkoff, J. P. (2016). Capitalizing on advances in science to reduce the health consequences of early childhood adversity. JAMA Pediatrics, 170(10), 1003–1007.
Shonkoff, J. P., & Meisels, S. J. (2000). Handbook of early childhood intervention.
Silliman Cohen, R. I., & Bosk, E. A. (2020). Vulnerable youth and the COVID-19 pandemic. Pediatrics, 146(1), e20201306.
Steele, R. G., Nesbitt-Daly, J. S., Daniel, R. C., & Forehand, R. (2005). Factor structure of the parenting scale in a low-income African American sample. Journal of Child and Family Studies, 14(4), 535–549.
Tottenham, N. (2020). Early adversity and the neotenous human brain. Biological psychiatry, 87(4), 350–358.
Wade, R., Cronholm, P. F., Fein, J. A., Forke, C. M., Davis, M. B., Harkins-Schwarz, M., ...Bair-Merritt, M. H. (2016). Household and community-level adverse childhood experiences and adult health outcomes in a diverse urban population. Child Abuse & Neglect, 52:135–45
Walsh, R. (2011). Lifestyle and mental health. American Psychologist, 66(7), 579–592.
Weathers, F. W., Litz, B. T., Keane, T. M., Palmieri, P. A., Marx, B. P., & Schnurr, P. P. (2013). The PTSD Checklist for DSM-5 (PCL-5). Retrieved from www.ptsd.va.gov
Weinreb, L. F., Buckner, J. C., Williams, V., & Nicholson, J. (2006). A comparison of the health and mental health status of homeless mothers in Worcester, Mass: 1993 and 2003. American Journal of Public Health, 96(8), 1444–1448.
Weiss, J. S., & Wagner, S. H. (1998). What explains the negative consequences of adverse childhood experiences on adult health? Insights from cognitive and neuroscience research (editorial). American Journal of Preventive Medicine, 14, 356–360.
Yamashiro, A. & McLaughlin, J. (2021). Early childhood homelessness state profiles: 2018–19. U.S. Department of Education, Office of Planning, Evaluation and Policy Development, Office of the Chief Data Officer. https://www2.ed.gov/about/offices/list/opepd/ppss/reports.html. Accessed 15 Oct 2022
Funding
This study was funded by the Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD (Grant #1 R44 HD088291-01). The NICHD approved the study design during the grant review process but was not involved in the decision to submit this paper for publication.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare no competing interests.
Additional information
Research Highlights
• Fifty-five percent of the sample (young children, ages 3–5) had a high child ACE score (> 3), even without the enumeration of residential instability/homelessness.
• ACEs were associated with lower attention, social skills, and emotional regulation but not communication, cognitive processing, and problem-solving skills during the preschool years.
• ACEs were strongly associated with 0.17 standard deviation units of higher caregiver distress (p < .001), which was also associated with 0.26 standard deviation units of lower levels of child neurodevelopmental functioning (p = .001).
• A bivariate regression model indicated that each unit increase in housing instability is associated with an increase by three-fourths of an ACE (0.78 ACE at p = .004). Four or more moves were associated with the worst neurodevelopmental outcomes for children.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
DeCandia, C.J., Volk, K.T. & Unick, G.J. Evolving Our Understanding: Housing Instability as an ACE for Young Children. ADV RES SCI 3, 365–380 (2022). https://doi.org/10.1007/s42844-022-00080-y
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s42844-022-00080-y