Abstract
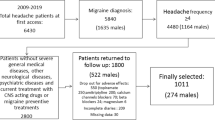
To study the short- and long-term effects of preventive treatment in a cohort of migraine patients, enlightening possible predictive factors for ineffectiveness and also analyzing the preventive’s dropout rates, clarifying the underlying reasons. This retrospective analysis included 210 patients who received a diagnosis of migraine without aura (MO), migraine with aura (MA), or chronic migraine (CM), according to ICHD-3 diagnostic criteria, with indication for prophylactic treatment. Three groups were defined and studied regarding the efficacy of oral preventives and dropout rates: group A referred to patients treated with a first preventive, group B with a second, and group C a third, respectively. Overall efficacy of our preventive treatment was low with 40% of patients improving with their first preventive. Also, successive prophylactic attempts were associated with progressively lower rates of efficacy. Patients in whom coexisted MOH (medication overuse headache) had lower rates of preventive inefficacy. The preventive’s dropout rates observed were also high (reaching 63.2% in subgroup C patients) with adverse drug reactions such as weight gain and cognitive dysfunction being the main reason for this. The modest effect of the oral preventive drugs as well as the high proportion of patients who dropped out due to drug side events confirms that in a significant proportion of patients, oral preventives can only delay a more focused therapeutic approach such as the new therapies with monoclonal CGRP antibodies.

Similar content being viewed by others
Data Availability
The data that support the findings of this study are available on request from the corresponding author. The data are not publicly available due to privacy or ethical restrictions.
Code Availability
Not applicable.
References
World Health Organization (WHO) Disease burden and mortality estimates. 2018
Sacco S, Braschinsky M, Ducros A, Lampl C, Little P, van den Brink AM, Pozo-Rosich P, Reuter U, de la Torre ER, Sanchez Del Rio M, Sinclair AJ, Katsarava Z, Martelletti P. European headache federation consensus on the definition of resistant and refractory migraine : developed with the endorsement of the European Migraine & Headache Alliance (EMHA). J Headache Pain. 2020;21(1):76. https://doi.org/10.1186/s10194-020-01130-5.
Lipton RB, Bigal ME, Diamond M, Freitag F, Reed ML, Stewart WF. Migraine prevalence, disease burden, and the need for preventive therapy. Neurology. 2007;68(5):343–9. https://doi.org/10.1212/01.wnl.0000252808.97649.21.
Silberstein SD, Winner PK, Chmiel JJ. Migraine preventive medication reduces resource utilization. Headache. 2003;43(3):171–8. https://doi.org/10.1046/j.1526-4610.2003.03040.x.
Silberstein SD. Preventive migraine treatment. Continuum (Minneap Minn). 2015;21(4 Headache):973–89. https://doi.org/10.1212/CON.0000000000000199.
Sprenger T, Viana M, Tassorelli C. Current prophylactic medications for migraine and their potential mechanisms of action. Neurotherapeutics. 2018;15(2):313–23. https://doi.org/10.1007/s13311-018-0621-8.
Aurora SK, Dodick DW, Turkel CC, et al. OnabotulinumtoxinA for treatment of chronic migraine: results from the double-blind, randomized, placebo-controlled phase of the PREEMPT 1 trial. Cephalalgia. 2010;30:793–803. https://doi.org/10.1177/0333102410364676.
Edvinsson L. The journey to establish CGRP as a migraine target: a retrospective view. Headache. 2015;55:1249–55. https://doi.org/10.1111/head.12656.
Ailani J, Burch RC, Robbins MS. The American Headache Society Consensus statement: update on integrating new migraine treatments into clinical practice. Headache J Head Face Pain. 2021;61(7):1021–39. https://doi.org/10.1111/head.14153.
Parreira E. Recomendações Terapêuticas Para Cefaleias da Sociedade Portuguesa de Cefaleias – 2021. Sinapse. 2021;21(supplement 1):3–100.
D’Antona L, Matharu M. Identifying and managing refractory migraine: barriers and opportunities? J Headache Pain. 2019;23:20.
Edvinsson L, Haanes KA, Warfvinge K, Krause DN. CGRP as the target of new migraine therapies - successful translation from bench to clinic. Nat Rev Neurol. 2018;14(6):338–50. https://doi.org/10.1038/s41582-018-0003-1.
Ford JH, Schroeder K, Buse DC, et al. Predicting initiation of preventive migraine medications: exploratory study in a large US medical claims database. Curr Med Res Opin. 2020;36(1):51–614. https://doi.org/10.1080/03007995.2019.1657716.
Piccinni C, Cevoli S, Ronconi G, et al. A real-world study on unmet medical needs in triptan-treated migraine: prevalence, preventive therapies and triptan use modification from a large Italian population along two years. J Headache Pain. 2019;20(1):74. https://doi.org/10.1186/s10194-019-1027-7.
García-Azorin D, Santos-Lasaosa S, Gago-Veiga AB, Viguera Romero J, Guerrero-Peral AL. Real world preventative drug management of migraine among Spanish neurologists. J Headache Pain. 2019;20(1):19. https://doi.org/10.1186/s10194-019-0971-6.
Sacco S, Lampl C, Amin FM, Braschinsky M, Deligianni C, Uludüz D, Versijpt J, Ducros A, Gil-Gouveia R, Katsarava Z, Martelletti P, Ornello R, Raffaelli B, Boucherie DM, Pozo-Rosich P, Sanchez-Del-Rio M, Sinclair A, Maassen van den Brink A, Reuter U. European Headache Federation (EHF) consensus on the definition of effective treatment of a migraine attack and of triptan failure. J Headache Pain. 2022;23(1):133. https://doi.org/10.1186/s10194-022-01502-z.
Headache Classification Subcommittee of International headache Society. The international classification of headache disorders, 2nd edition. Cephalalgia. 2004;24(Suppl. 1):24–36
De Tommaso M, Delussi M. Failure of preventive treatments in migraine: an observational retrospective study in a tertiary headache center. SSRN Electron J. 2020. https://doi.org/10.2139/ssrn.3566240.
Steiner TJ, Jensen R, Katsarava Z, et al. Aids to management of headache disorders in primary care (2nd edition): on behalf of the European Headache Federation and Lifting The Burden: the Global Campaign against Headache. J Headache Pain. 2019;20(1):57. https://doi.org/10.1186/s10194-018-0899-2.
Diener HC, Agosti R, Allais G, Bergmans P, Bussone G, Davies B, Ertas M, Lanteri-Minet M, Reuter U, Sánchez Del Río M, Schoenen J, Schwalen S, van Oene J; TOPMAT-MIG-303 Investigators Group. Cessation versus continuation of 6-month migraine preventive therapy with topiramate (PROMPT): a randomised, double-blind, placebo-controlled trial. Lancet Neurol. 2007 Dec;6(12):1054–62. https://doi.org/10.1016/S1474-4422(07)70272-7. Erratum in: Lancet Neurol. 2008 Jan;7(1):25.
Sacco S, Cerone D, Carolei A. Comorbid neuropathologies in migraine: an update on cerebrovascular and cardiovascular aspects. J Headache Pain. 2008;9:237–48. https://doi.org/10.1007/s10194-008-0048-4.
Schulman EA, Lake AE 3rd, Goadsby PJ, Peterlin BL, Siegel SE, Markley HG, Lipton RB. Defining refractory migraine and refractory chronic migraine: proposed criteria from the refractory headache special interest section of the American headache society. Headache. 2008;48:778–82. https://doi.org/10.1111/j.1526-4610.2008.01132.x.
Vandenbussche N, Laterza D, Lisicki M, Lloyd J, Lupi C, Tischler H, Toom K, Vandervorst F, Quintana S, Paemeleire K, Katsarava Z. Medication-overuse headache: a widely recognized entity amidst ongoing debate. J Headache Pain. 2018;19(1):50. https://doi.org/10.1186/s10194-018-0875-x.
Weatherall MW. The diagnosis and treatment of chronic migraine. Ther Adv Chronic Dis. 2015;6(3):115–23. https://doi.org/10.1177/2040622315579627.
Boes CJ, Capobianco DJ. Chronic migraine and medication-overuse headache through the ages. Cephalalgia. 2005;25(5):378–90. https://doi.org/10.1111/j.1468-2982.2005.00868.x.
Author information
Authors and Affiliations
Contributions
All the authors were involved in the conception of the work and the acquisition, analysis an interpretation of data. A.F and S.M. were responsible for drafting of the work, revising it critically for important intellectual content and agreement in all aspects related to the accuracy or integrity.
Corresponding author
Ethics declarations
Ethics Approval
This study was approved by the local Ethics Committee—Ethics and health commission of Hospital of Braga, Portugal.
Consent to Participate
Oral informed consent for inclusion in the study were obtained from all subjects.
Consent for Publication
All authors gave written and verbal informed consent for publication.
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Medicine
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Ferreira, A., Marques, S.R., Lopes, S. et al. Preventive Oral Treatment in Migraine: Efficacy and Dropout Rates Observed at a Tertiary Headache Center. SN Compr. Clin. Med. 5, 38 (2023). https://doi.org/10.1007/s42399-022-01369-w
Accepted:
Published:
DOI: https://doi.org/10.1007/s42399-022-01369-w