Abstract
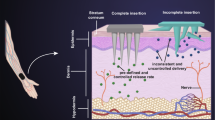
Biodegradable hydrogels are promising biomaterials for use in controlled-release systems for skin tissue regeneration. Controlled delivery systems constitute an important aspect of tissue engineering because they can modulate various physiological responses, including early immune response, tissue remodeling, and cell proliferation and maturation in the wound-healing process. Hydrogels composed of various biomaterials have been developed to overcome the limitations of conventional drug- or protein-delivery systems, such as limited targeting ability, low stability, and the induction of drug resistance. Hydrogels based on keratin, a natural polymer extracted from human hair, can provide adequate cell support and control homeostasis. Consequently, they can be applied for skin tissue engineering. In this study, we prepared degradable, tunable, and biocompatible hydrogels for controllable protein delivery. We synthesized keratin-fibrinogen (KER-FBG) by the chemical coupling reaction and prepared hydrogels through polymerization with thrombin. The structures and morphologies of the KER-FBG hydrogels were confirmed. Furthermore, the mechanical properties, swelling ratio, degradation, release behavior, and biocompatibility were investigated. The KER-FBG hydrogels presented promising biological performance, indicating that the material is suitable as a controlled protein delivery carrier.






Similar content being viewed by others
Data availability
All the data generated during or analyzed within this study are included in this published article.
References
Priya, S. G., Jungvid, H., & Kumar, A. (2008). Skin tissue engineering for tissue repair and regeneration. Tissue Engineering. Part B, Reviews, 14(1), 105–118.
Jones, I., Currie, L., & Martin, R. (2002). A guide to biological skin substitutes. British Journal of Plastic Surgery, 55(3), 185–193.
Langemo, D. K., & Brown, G. (2006). Skin fails too: acute, chronic, and end-stage skin failure. Advances in Skin & Wound Care, 19(4), 206–211.
Bannasch, H., Fohn, M., Unterberg, T., Bach, A. D., Weyand, B., & Stark, G. B. (2003). Skin tissue engineering. Clinics in Plastic Surgery, 30(4), 573–579.
Huang, S., & Fu, X. B. (2010). Naturally derived materials-based cell and drug delivery systems in skin regeneration. Journal of Controlled Release, 142(2), 149–159.
Peppas, N. A. (1997). Hydrogels and drug delivery. Curr Opinion Colloid Inter Sci, 2(5), 531–537.
Selvan, N. K., Shanmugarajan, T. S., & Uppuluri, V. N. V. A. (2020). Hydrogel based scaffolding polymeric biomaterials: approaches towards skin tissue regeneration. Journal of Drug Delivery Science and Technology, 55, 101456.
Kim, H. E., Lee, H. J., Seong, K. Y., Lee, E. S., Yang, S. Y., & Yoon, J. H. (2015). Visible light-triggered on-demand drug release from hybrid hydrogels and its application in transdermal patches. Advanced Healthcare Materials, 4(14), 2071–2077.
Kharaziha, M., Baidya, A., & Annabi, N. (2021). Rational design of immunomodulatory hydrogels for chronic wound healing. Advanced Materials, 33(39), 2100176.
Tavakoli, S., & Klar, A. S. (2020). Advanced hydrogels as wound dressings. Biomole, 10(8), 1169.
Liang, Y. P., He, J. H., & Guo, B. L. (2021). Functional hydrogels as wound dressing to enhance wound healing. ACS Nano, 15(8), 12687–12722.
Chen, J. Y., He, J. H., Yang, Y. T., Qiao, L. P., Hu, J., Zhang, J., & Guo, B. L. (2022). Antibacterial adhesive self-healing hydrogels to promote diabetic wound healing. Acta Biomaterialia, 146, 119–130.
Li, M., Li, H. C., Li, X. G., Zhu, H., Xu, Z. H., Liu, L. Q., Ma, J. J., & Zhang, M. J. (2017). A bioinspired alginate-gum arabic hydrogel with micro-/nanoscale structures for controlled drug release in chronic wound healing. ACS Applied Materials & Interfaces, 9(27), 22160–22175.
Dreiss, C. A. (2020). Hydrogel design strategies for drug delivery. Current Opinion in Colloid and Interface Science, 48, 1–17.
Mtibe, A., Motloung, M. P., Bandyopadhyay, J., & Ray, S. S. (2021). Synthetic biopolymers and their composites: advantages and limitationsa-an overview. Macromolecular Rapid Communications, 42(15), 2100130.
Sohail, M., Mudassir Minhas, M. U., Khan, S., Hussain, Z., de Matas, M., Shah, S. A., Khan, S., Kousar, M., & Ullah, K. (2019). Natural and synthetic polymer-based smart biomaterials for management of ulcerative colitis: a review of recent developments and future prospects. Drug Delivery and Translational Research, 9(2), 595–614.
Tabata, Y. (2004). Tissue regeneration based on tissue engineering technology. Congenit Anomal (Kyoto), 44(3), 111–124.
Shavandi, A., Silva, T. H., Bekhit, A. A., & Bekhit, A. E. A. (2017). Keratin: dissolution, extraction and biomedical application. Biomaterials Science, 5(9), 1699–1735.
Wang, B., Yang, W., McKittrick, J., & Meyers, M. A. (2016). Keratin: Structure, mechanical properties, occurrence in biological organisms, and efforts at bioinspiration. Progress in Materials Science, 76, 229–318.
Placone, J. K., Navarro, J., Laslo, G. W., Lerman, M. J., Gabard, A. R., Herendeen, G. J., Falco, E. E., Tomblyn, S., Burnett, L., & Fisher, J. P. (2017). Development and characterization of a 3D printed, keratin-based hydrogel. Annals of Biomedical Engineering, 45(1), 237–248.
Pechter, P. M., Gil, J., Valdes, J., Tomic-Canic, M., Pastar, I., Stojadinovic, O., Kirsner, R. S., & Davis, S. C. (2012). Keratin dressings speed epithelialization of deep partial-thickness wounds. Wound Rep Regenerat, 20(2), 236–242.
Ham, T. R., Lee, R. T., Han, S., Haque, S., Vodovotz, Y., Gu, J., Burnett, L. R., Tomblyn, S., & Saul, J. M. (2016). Tunable keratin hydrogels for controlled erosion and growth factor delivery. Biomacromolecules, 17(1), 225–236.
Navarro, J., Clohessy, R. M., Holder, R. C., Gabard, A. R., Herendeen, G. J., Christy, R. J., Burnett, L. R., & Fisher, J. P. (2020). In vivo evaluation of three-dimensional printed, keratin-based hydrogels in a porcine thermal burn model. Tissue Engineering Part A, 26(5–6), 265–278.
Reinke, J. M., & Sorg, H. (2012). Wound repair and regeneration. European Surgical Research, 49, 35–43.
Kumar, V., Bouameur, J. E., Bär, J., Rice, R. H., Hornig-Do, H. T., Roop, D. R., Schwarz, N., Brodesser, S., Thiering, S., Leube, R. E., Wiesner, R. J., Vijayaraj, P., Brazel, C. B., Heller, S., Binder, H., Löffler-Wirth, H., Seibel, P., & Magin, T. M. (2015). A keratin scaffold regulates epidermal barrier formation, mitochondrial lipid composition, and activity. Journal of Cell Biology, 211(5), 1057–1075.
Sadeghi, S., Nourmohammadi, J., Ghaee, A., & Soleimani, N. (2020). Carboxymethyl cellulose-human hair keratin hydrogel with controlled clindamycin release as antibacterial wound dressing. International Journal of Biological Macromolecules, 147, 1239–1247.
Choi, W. S., Kim, J. H., Ahn, C. B., Lee, J. H., Kim, Y. J., Son, K. H., & Lee, J. W. (2021). Development of a multi-layer skin substitute using human hair keratinic extract-based hybrid 3D printing. Polymers, 13(16), 2584.
Islam, M. T., Laing, R. M., Wilson, C. A., McConnell, M., & Ali, M. A. (2022). Fabrication and characterization of 3-dimensional electrospun poly(vinyl alcohol)/keratin/chitosan nanofibrous scaffold. Carbohydrate Poly, 275, 118682.
Mitura, S., Sionkowska, A., & Jaiswal, A. (2020). Biopolymers for hydrogels in cosmetics: review. Journal of Materials Science. Materials in Medicine, 31(6), 31–50.
Cao, Y., Yao, Y. Q., Li, Y., Yang, X. X., Cao, Z. Y., & Yang, G. (2019). Tunable keratin hydrogel based on disulfide shuffling strategy for drug delivery and tissue engineering. Journal of Colloid and Interface Science, 544, 121–129.
Grigsby, W. J., Scott, S. M., Plowman-Holmes, M. I., Middlewood, P. G., & Recabar, K. (2020). Combination and processing keratin with lignin as biocomposite materials for additive manufacturing technology. Acta Biomaterialia, 104, 95–103.
Almany, L., & Seliktar, D. (2005). Biosynthetic hydrogel scaffolds made from fibrinogen and polyethylene glycol for 3D cell cultures. Biomaterials, 26(15), 2467–2477.
Eyrich, D., Brandl, F., Appel, B., Wiese, H., Maier, G., Wenzel, M., Staudenmaier, R., Goepferich, A., & Blunk, T. (2007). Long-term stable fibrin gels for cartilage engineering. Biomaterials, 28(1), 55–65.
Ao, Q., Wang, S. L., He, Q., Ten, H., Oyama, K., Ito, A., He, J., Javed, R., Wang, A. J., & Matsuno, A. (2020). Fibrin glue/fibronectin/heparin-based delivery system of BMP2 induces osteogenesis in MC3T3-E1 cells and bone formation in rat calvarial critical-sized defects. ACS Applied Materials & Interfaces, 12(11), 13400–13410.
Melly, L., Grosso, A., Stanciu Pop, C., Yu-Hsuan, C., Nollevaux, M. C., Schachtrup, C., Marsano, A., Di Maggio, N., Rondelet, B., & Banfi, A. (2020). Fibrin hydrogels promote scar formation and prevent therapeutic angiogenesis in the heart. Journal of Tissue Engineering and Regenerative Medicine, 14(10), 1513–1523.
Kang, H. J., Ko, N. R., Oh, S. J., An, S. Y., Hwang, Y. S., & Kim, S. Y. (2021). Injectable human kair keratin-fibrinogen hydrogels for engineering 3D microenvironments to accelerate oral tissue regeneration. International Journal of Molecular Sciences, 22(24), 13269.
Guo, W. J., Leu, W. T., Hsiao, S. H., & Liou, G. S. (2006). Thermal degradation behaviour of aromatic poly(ester-amide) with pendant phosphorus groups investigated by pyrolysis-GC/MS. Poly Degrad Stability, 91(1), 21–30.
Yan, Q., Zheng, H. N., Jiang, C., Li, K., & Xiao, S. J. (2015). EDC/NHS activation mechanism of polymethacrylic acid: anhydride versus NHS-ester. RSC Advances, 5(86), 69939–69947.
Karageorgiou, V., & Kaplan, D. (2005). Porosity of 3D biomaterial scaffolds and osteogenesis. Biomaterials, 26(27), 5474–5491.
Luo, T. Y., Tan, B. W., Zhu, L. J., Wang, Y. T., & Liao, J. F. (2022). A review on the design of hydrogels with different stiffness and their effects on tissue repair. Frontiers in Bioengineering and Biotechnology, 10, 817391.
Xue, R. Y., Li, J. Y. S., Yeh, Y. T., Yang, L., & Chien, S. (2013). Effects of matrix elasticity and cell density on human mesenchymal stem cells differentiation. Journal of Orthopaedic Research, 31(9), 1360–1365.
Gu, Y., Ji, Y. W., Zhao, Y. H., Liu, Y., Ding, F., Gu, X. S., & Yang, Y. M. (2012). The influence of substrate stiffness on the behavior and functions of Schwann cells in culture. Biomaterials, 33(28), 6672–6681.
Peng, Q. Y., Chen, J. S., Wang, T., Peng, X. W., Liu, J. F., Wang, X. G., Wang, J. M., & Zeng, H. B. (2020). Recent advances in designing conductive hydrogels for flexible electronics. Infomat, 2(5), 843–865.
Zhang, X. N., Wang, Y. J., Sun, S. T., Hou, L., Wu, P. Y., Wu, Z. L., & Zheng, Q. (2018). A tough and stiff hydrogel with tunable water content and mechanical properties based on the synergistic effect of hydrogen bonding and hydrophobic interaction. Macromolecules, 51(20), 8136–8146.
Hoare, T. R., & Kohane, D. S. (2008). Hydrogels in drug delivery: Progress and challenges. Polymer, 49(8), 1993–2007.
Rawn, J. D., & Ouellette, R. J. (2018). Organic Chemistry: Structure, Mechanism, Synthesis (pp. 763–799). Cambridge US: Academic Press.
Hori, K., Sotozono, C., Hamuro, J., Yamasaki, K., Kimura, Y., Ozeki, M., Tabata, Y., & Kinoshita, S. (2007). Controlled-release of epidermal growth factor from cationized gelatin hydrogel enhances corneal epithelial wound healing. Journal of Controlled Release, 118(2), 169–176.
Babich, H., & Sinensky, M. C. (2001). Indirect cytotoxicity of dental materials: a study with Transwell inserts and the neutral red uptake assay. Altern Lab Ani, 29(1), 9–13.
Werner, S., Krieg, T., & Smola, H. (2007). Keratinocyte-fibroblast interactions in wound healing. The Journal of Investigative Dermatology, 127(5), 998–1008.
Zhu, J. M., & Marchant, R. E. (2011). Design properties of hydrogel tissue-engineering scaffolds. Expert Review of Medical Devices, 8(5), 607–626.
Bordeleau, F., Bessard, J., Sheng, Y. L., & Marceau, N. (2008). Keratin contribution to cellular mechanical stress response at focal adhesions as assayed by laser tweezers. Biochemistry and Cell Biology, 86(4), 352–359.
Laly, A. C., Sliogeryte, K., Pundel, O. J., Ross, R., Keeling, M. C., Avisetti, D., Waseem, A., Gavara, N., & Connelly, J. T. (2021). The keratin network of intermediate filaments regulates keratinocyte rigidity sensing and nuclear mechanotransduction. Science Advances, 7(5), 6187.
Feroz, S., Muhammad, N., Ratnayake, J., & Dias, G. (2020). Keratin—Based materials for biomedical applications. Bioactive Materials, 5(3), 496–509.
Borrelli, M., Joepen, N., Reichl, S., Finis, D., Schoppe, M., Geerling, G., & Schrader, S. (2015). Keratin films for ocular surface reconstruction: evaluation of biocompatibility in an in-vivo model. Biomaterials, 42, 112–120.
Lin, C. W., Chen, Y. K., Tang, K. C., Yang, K. C., Cheng, N. C., & Yu, J. S. (2019). Keratin scaffolds with human adipose stem cells: Physical and biological effects toward wound healing. Journal of Tissue Engineering and Regenerative Medicine, 13(6), 1044–1058.
Acknowledgements
This research was supported by a National Research Foundation of Korea (NRF) grant funded by the Korean government (MSIT) (NRF-2020R1A2C2011937, 2020R1C1C1007129), a grant of the Korea Health Technology R&D Project through the Korea Health Industry Development Institute (KHIDI) funded by the Ministry of Health & Welfare (HI22C1572) and R&BD Program through the INNOPOLIS funded by Ministry of Science and ICT (2021-IT-RD-0059-01-101).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare that they have no known competing financial interests or personal relationships that could have influenced the work reported in this study.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Min, S.J., Lee, J.S., Nah, H. et al. Degradable and Tunable Keratin-fibrinogen Hydrogel as Controlled Release System for Skin Tissue Regeneration. J Bionic Eng 20, 1049–1059 (2023). https://doi.org/10.1007/s42235-022-00317-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s42235-022-00317-7