Abstract
Purpose
Primary aldosteronism (PA) is the most frequent type of endocrine hypertension. In our previous studies, we introduced two modified diagnostic tests for PA, the post-dexamethasone saline infusion test (DSIT) and the overnight dexamethasone, captopril, and valsartan test (DCVT). In this study, we aimed to validate both tests in respect to the biochemical and clinical response of a cohort of hypertensive patients in pre- and post-surgical setting.
Methods
We retrospectively studied 41 hypertensive patients (16 males), with a median (IQR, range) age of 50 (16, 35–74) years and positive histology for adrenal adenoma. Preoperatively, all patients had a single adenoma on CT and a diagnosis of PA with either DSIT or DCVT. The defined daily dose (DDD) of hypertensive drugs was assessed pre- and postoperatively. DSIT or DCVT and basal ARR were reassessed postoperatively.
Results
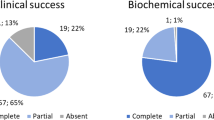
Two of the 41 patients failed to suppress aldosterone post-surgery, leading to a post-adrenalectomy biochemical cure rate of 95%, while blood pressure was improved in 36 patients, leading to a clinical cure rate of 88% as assessed by the DDD methodology.
Conclusions
The present study was a proof-of-concept process to validate two modified diagnostic tests for PA in clinical practice. These tests, used to diagnose a group of patients with PA, successfully assessed their biochemical cure post-adrenalectomy at rates similar to those reported in the literature.


Similar content being viewed by others
Data availability statement
The data are available on request
Data availability
The data are available on demand.
Code availability
Not applicable
References
Gouli A, Kaltsas G, Tzonou A, Markou A, Androulakis II, Ragkou D, Vamvakidis K, Zografos G, Kontogeorgos G, Chrousos GP, Piaditis G (2011) High prevalence of autonomous aldosterone secretion among patients with essential hypertension. Eur J Clin Invest 41:1227–1236
Piaditis G, Markou A, Papanastasiou L, Androulakis II, Kaltsas G (2015) Progress in aldosteronism: a review of the prevalence of primary aldosteronism in pre-hypertension and hypertension. Eur J Endocrinol 172:R191–R203
Rossi GP, Cesari M, Cuspidi C, Maiolino G, Cicala MV, Bisogni V, Mantero F, Pessina AC (2013) Long-term control of arterial hypertension and regression of left ventricular hypertrophy with treatment of primary aldosteronism. Hypertension 62:62–69
Funder JW, Carey RM, Mantero F, Murad MH, Reincke M, Shibata H, Stowasser M, Young WF Jr (2016) The management of primary aldosteronism: case detection, diagnosis, and treatment: an Endocrine Society Clinical Practice Guideline. J Clin Endocrinol Metab 101:1889–1916
Markou A, Sertedaki A, Kaltsas G, Androulakis II, Marakaki C, Pappa T, Gouli A, Papanastasiou L, Fountoulakis S, Zacharoulis A, Karavidas A, Ragkou D, Charmandari E, Chrousos GP, Piaditis GP (2015) Stress-induced aldosterone hyper-secretion in a substantial subset of patients with essential hypertension. J Clin Endocrinol Metab 100:2857–2864
Piaditis GP, Kaltsas GA, Androulakis II, Gouli A, Makras P, Papadogias D, Dimitriou K, Ragkou D, Markou A, Vamvakidis K, Zografos G, Chrousos G (2009) High prevalence of autonomous cortisol and aldosterone secretion from adrenal adenomas. Clin Endocrinol (Oxf) 71:772–778
Tsiavos V, Markou A, Papanastasiou L, Kounadi T, Androulakis II, Voulgaris N, Zachaki A, Kassi E, Kaltsas G, Chrousos GP, Piaditis GP (2016) A new highly sensitive and specific overnight combined screening and diagnostic test for primary aldosteronism. Eur J Endocrinol 175:21–28
Markou A, Pappa T, Kaltsas G, Gouli A, Mitsakis K, Tsounas P, Prevoli A, Tsiavos V, Papanastasiou L, Zografos G, Chrousos GP, Piaditis GP (2013) Evidence of primary aldosteronism in a predominantly female cohort of normotensive individuals: a very high odds ratio for progression into arterial hypertension. J Clin Endocrinol Metab. 98(4):1409–1416
Dekkers T, Prejbisz A, Kool LJS, Groenewoud HJMM, Velema M, Spiering W, Kołodziejczyk-Kruk S, Arntz M, Kądziela J, Langenhuijsen JF, Kerstens MN, van den Meiracker AH, van den Born BJ, Sweep FCGJ, Hermus ARMM, Januszewicz A, Ligthart-Naber AF, Makai P, van der Wilt GJ, Lenders JWM, Deinum J, Investigators SPARTACUS (2016) Adrenal vein sampling versus CT scan to determine treatment in primary aldosteronism: an outcome-based randomised diagnostic trial. Lancet Diabetes Endocrinol 4:739–746
Beuschlein F, Mulatero P, Asbach E, Monticone S, Catena C, Sechi LA, Stowasser M (2017) The SPARTACUS trial: controversies and unresolved issues. Horm Metab Res 49:936–942
Muth A, Ragnarsson O, Johannsson G, Wängberg B (2015) Systematic review of surgery and outcomes in patients with primary aldosteronism. Br J Surg 102:307–317
Yang Y, Reincke M, Williams TA (2019) Treatment of unilateral PA by adrenalectomy potential reasons for incomplete biochemical cure. Exp Clin Endocrinol Diabetes 127:100–108
Perysinakis I, Marakaki C, Avlonitis S, Katseli A, Vassilatou E, Papanastasiou L, Piaditis G, Zografos GN (2013) Laparoscopic adrenalectomy in patients with subclinical Cushing syndrome. Surg Endosc 27:2145–2148
Kim K, Kim JK, Lee CR, Kang SW, Lee J, Jeong JJ, Nam KH, Chung WY (2019) Surgical outcomes of laparoscopic adrenalectomy for primary hyperaldosteronism: 20 years of experience in a single institution. Ann Surg Treat Res 96:223–229
Fassnacht M, Arlt W, Bancos I, Dralle H, Newell-Price J, Sahdev A, Tabarin A, Terzolo M, Tsagarakis S, Dekkers OM (2016) Management of adrenal incidentalomas: European Society of Endocrinology Clinical Practice Guideline in collaboration with the European Network for the Study of Adrenal Tumors. Eur J Endocrinol 175:G1–G34
Papanastasiou L, Markou A, Pappa T, Gouli A, Tsounas P, Fountoulakis S, Kounadi T, Tsiama V, Dasou A, Gryparis A, Samara C, Zografos G, Kaltsas G, Chrousos G, Piaditis G (2014 Aug) Primary aldosteronism in hypertensive patients: clinical implications and target therapy. Eur J Clin Invest. 44(8):697–706. https://doi.org/10.1111/eci.12286
Modolo R, de Faria AP, Ritter AM, Coca A, Moreno H (2016 Jan 1) Defined daily dose (DDD) and its potential use in clinical trials of resistant hypertension. Int J Cardiol. 202:515–516
World Health Organization Collaborating Centre for Drug Statistics Methodology. ATC classification index with DDDs Access [2021 January 11]; Available from: http://www.whocc.no/atc_ddd_publications/atc_ddd_index/
Meyer A, Brabant G, Behrend M (2005) Long-term follow-up after adrenalectomy for primary aldosteronism. World J Surg 29:155–159
Wang W, Hu W, Zhang X, Wang B, Bin C, Huang H (2012) Predictors of successful outcome after adrenalectomy for primary aldosteronism. Int Surg 97:104–111
Waldmann J, Maurer L, Holler J, Kann PH, Ramaswamy A, Bartsch DK, Langer P (2011) Outcome of surgery for primary hyperaldosteronism. World J Surg 35:2422–2427
Lumachi F, Ermani M, Basso SM, Armanini D, Iacobone M, Favia G (2005) Long-term results of adrenalectomy in patients with aldosterone-producing adenomas: multivariate analysis of factors affecting unresolved hypertension and review of the literature. Am Surg 71:864–869
Proye CA, Mulliez EA, Carnaille BM, Lecomte-Houcke M, Decoulx M, Wémeau JL, Lefebvre J, Racadot A, Ernst O, Huglo D, Carré A (1998) Essential hypertension: first reason for persistent hypertension after unilateral adrenalectomy for primary aldosteronism? Surgery 124:1128–1133
Williams TA, Lenders JWM, Mulatero P, Burrello J, Rottenkolber M, Adolf C, Satoh F, Amar L, Quinkler M, Deinum J, Beuschlein F, Kitamoto KK, Pham U, Morimoto R, Umakoshi H, Prejbisz A, Kocjan T, Naruse M, Stowasser M, Nishikawa T, Young WF Jr, Gomez-Sanchez CE, Funder JW, Reincke M, Primary Aldosteronism Surgery Outcome (PASO) investigators (2017) Outcomes after adrenalectomy for unilateral primary aldosteronism: an international consensus on outcome measures and analysis of remission rates in an international cohort. Lancet Diabetes Endocrinol 5:689–699
Blumenfeld JD, Sealey JE, Schlussel Y, Vaughan ED Jr, Sos TA, Atlas SA, Müller FB, Acevedo R, Ulick S, Laragh JH (1994) Diagnosis and treatment of primary hyperaldosteronism. Ann Intern Med 121:877–885
Alexandraki KI, Antonopoulou I, Papaioannou TG, Kykalos S, Sotiropoulos GC, Kolomodi D, Ntokos G, Pateas K, Aggeli C, Kaltsas GA, Zografos GN (2020) Accuracy of adrenal imaging modalities in predicting histological tumor dimension following adrenalectomy. Arch Balk Med Union 55:375–381
Young WF, Stanson AW, Thompson GB, Grant CS, Farley DR, van Heerden JA (2004) Role for adrenal venous sampling in primary aldosteronism. Surgery 136:1227–1235
Kempers MJ, Lenders JW, van Outheusden L, van der Wilt GJ, Schultze Kool LJ, Hermus AR, Deinum J (2009) Systematic review: diagnostic procedures to differentiate unilateral from bilateral adrenal abnormality in primary aldosteronism. Ann Intern Med 151:329–337
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics approval
The study protocol was approved by the Institutional Ethics Committee of the General Hospital of Athens “G. Gennimatas”, and informed consent was obtained from all the study participants.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Alexandraki, K.I., Markou, A., Papanastasiou, L. et al. Surgical treatment outcome of primary aldosteronism assessed using new modified diagnostic tests. Hormones 20, 359–368 (2021). https://doi.org/10.1007/s42000-021-00280-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s42000-021-00280-8