Key summary points
We aimed to determine outcomes of hip fracture in centenarians.
AbstractSection FindingOne-year mortality following a hip fracture was 53.8% (95% CI 47.2 to 60.3%). Dementia (26.2%, 95% CI 15.7 to 38.2%) and hypertension (15.6%, 95% CI 3.4 to 33.1%) were the most common comorbidities.
AbstractSection MessageEffective cross-discipline communication and intervention is suggested to promote treatment outcomes.
Abstract
Purpose
Outcomes of hip fractures in centenarians remain underreported owing to the small number of patients reaching 100 years of age. This review aimed to determine outcomes of hip fracture in centenarians and to identify the most common comorbidities among centenarians with hip fracture to better characterise this population.
Methods
Published and unpublished literature databases, conference proceedings and the reference lists of included studies were searched to the 25th of January 2023. A random-effects meta-analysis was performed. Included studies were appraised using tools respective of study design.
Results
Twenty-three studies (6970 centenarians) were included (retrospective period: 1990–2020). The evidence was largely moderate to low in quality. One-year mortality following a hip fracture was 53.8% (95% CI 47.2 to 60.3%). Pooled complication rate following a hip fracture in centenarians was 50.5% (95% CI 25.3 to 75.6%). Dementia (26.2%, 95% CI 15.7 to 38.2%), hypertension (15.6%, 95% CI 3.4 to 33.1%), and diabetes (5.5%, 95% CI 1.9 to 10.7%) were the most common comorbidities among centenarians with hip fracture.
Conclusion
Hip fractures in centenarians typically involve complex patient presentations with diverse comorbidities. However, the current evidence-base is moderate to low in quality. Effective cross-discipline communication and intervention is suggested to promote treatment outcomes.
Similar content being viewed by others
Introduction
The number of oldest-old is increasing in high income countries [1], with declining mortality in the 80 years and older age group and improved treatments contributing to an increasing number of centenarians in the last decades. The number of centenarians is projected to increase to between 13 and 50 million individuals worldwide during the twenty-first century [2]. Centenarians experience a higher mortality than other older age groups, such as those aged 80–99 years [1].
Older people are susceptible to trauma owing to an increased risk of delirium and dementia [3], incontinence, frailty, impaired vision and drug interactions [4]. In addition, side effects of commonly used drugs with central nervous system effects (such as benzodiazepines and anti-psychotics) can increase risk of falls, as well as orthostatic hypotension. Resulting fractures are the third most common cause of hospitalisation for this population [5]. Fractures in older people can lead to significant disruptions in daily activities and loss of independence. A review of outcomes following hip fracture estimated between 40 and 60% of patients do not recover their pre-fracture level of mobility, while 30 to 60% do not regain their level of independence for basic activities of daily living [6].
Outcomes of hip fracture in centenarians remain comparatively under-explored owing to the small number of patients reaching 100 years of age [7]. This group of patients are at particular risk of poor outcomes following hip fracture. Centenarians have a high comorbidity burden and polypharmacy, resulting in increased surgical risk [8]. Progressively poorer bone quality than younger individuals predisposes the oldest of people to more complex fractures [9].
To the authors’ knowledge, no systematic reviews have been undertaken assessing the outcomes or characterisation of centenarians who have sustained a hip fracture. Understanding hip fracture outcomes of people 100 years and older is required considering the number of centenarians is projected to increase [2]. Though negative outcomes may be expected due to a high comorbidity burden, these are yet to be formally synthesised. Accordingly, this review aimed to determine outcomes of hip fracture in centenarians and to identify the most common comorbidities among centenarians with hip fractures to better characterise this population.
Methods
The PRISMA 2020 checklist was satisfied in the reporting of this systematic review [10]. The protocol for this systematic review was prospectively registered (PROSPERO Registration: CRD42022377719).
Study eligibility
Studies were eligible if they reported outcomes of treatment for hip fractures in centenarians (both conservative and surgical), and/or comorbidities in centenarians who sustain a hip fracture. Both full-texts and abstracts were included. Eligible study designs were case series, case–control, cross-sectional and cohort studies, as well as randomised controlled trials. Both retrospective and prospective studies were eligible. Papers not reporting original data such as literature or systematic reviews were excluded, along with case reports and letters to the editor. There was no constraint based on language, publication status or patient demographics. Eligibility assessment was performed independently by two reviewers (DAAL, CKB). Disagreements regarding study eligibility were solved through discussion.
Search strategy and data extraction
We searched the following electronic databases via OVID: MEDLINE, Global Health, and Embase. Currently registered studies were reviewed using the databases: ISRCTN registry, the National Institute for Health Research Portfolio, the UK National Research Register Archive, the WHO International Clinical Trials Registry Platform, and OpenSIGLE (system for information on grey literature in Europe). Conference proceedings from the European Federation of National Associations of Orthopaedics and Traumatology (EFORT), British Orthopaedic Association (BOA) and British Trauma Society (BTS) were searched. The reference lists of included studies were also searched (backwards-searching). Finally, papers citing the studies included were also reviewed for eligibility (forward-searching).
Database search and data extraction were conducted independently by two reviewers (DAAL, CKB). Searches were conducted twice for quality assurance. The final search was completed on the 25th of January 2023. The search strategy is presented in Appendix 1 and modified for each respective database.
Data were extracted onto a data extraction template. Data extracted included: baseline characteristics including number of patients, treatment received, patient sex, age, study location, fracture type, fracture management, comorbid diseases, mortality and complications.
Outcomes
All-cause mortality was calculated, including in-hospital mortality, mortality at 1, 3, 6 months, and 1-year post-fracture. At this extreme of age, mortality beyond 1 year was excluded, as it may be unrelated to the hip fracture. Other outcomes included prevalence of comorbidities in centenarians and non-centenarians, and complications (occurrence and rate) over follow-up periods. The latter were not restricted to a specific time after fracture, since no study defined the duration of the observation period for which complications were monitored. Therefore, we assumed these took place before the final follow-up period post-operatively reported in the studies.
Methodological appraisal
Level of evidence and risk of bias of each included study were evaluated independently by two reviewers (DAAL, CKB). The level of evidence of the studies presented was determined with the March 2009 Oxford Centre for Evidence-Based Medicine: Levels of Evidence (5 = lowest level of evidence, corresponding to case reports; 1a = highest level of evidence, corresponding systematic reviews of randomised controlled trials) [11]. Each study was appraised with an appraisal tool reflecting the study design. Accordingly, tools used included the Institute of Health Economics case series studies quality appraisal checklist [12] and the Downes and Black Tool for cross-sectional studies [13].
Data analysis
Where sufficient (at least two) and homogeneous studies reported on the same outcome, a random-effects meta-analysis was performed using MetaXL version 5.3 software (EpiGear International Pty Ltd, Wilston, Queensland, Australia). Data on prevalence was presented as weighted prevalence percentage and 95% confidence intervals (CI). Data on continuous outcomes, i.e. Charlson Comorbidities Index (CCI) was presented as weighed mean difference and 95% CI. Statistical heterogeneity was assessed using Cochran’s Q value and Higgins I2 statistic for each pooled analysis. This was interpreted in accordance with Higgins and Green [14]. Subgroup analysis of surgical management of hip fractures was undertaken, comparing mortality following surgical intervention with the overall cohort mortality (irrespective of treatment received).
Results
Search results
In total, 4671 records were screened, of which 23 studies were eligible and evaluated 6970 centenarians (Fig. 1, Table 1). Mean patient age was 101.5 (range 100–111) years. Twenty-two studies reported patient sex (816 males, 11.7% and 6133 females, 88.3%). No study reported whether their patients had concomitant injuries, patient osteoporotic status, nor commented on the severity of hip fracture.
Study quality assessments
All studies identified were case series or cross-sectional studies, with a corresponding level of evidence being four. Whether relevant outcome measures were established a-[ priori or if outcome assessors were blinded to intervention administered were unclear for all studies (Table 2). Overall, the majority of studies included exhibited methodological limitations pertaining to low level of evidence and concerns regarding risk of bias.
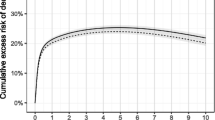
Mortality outcomes of hip fractures in centenarians
Mortality was assessed in all 23 included studies (Appendix 2). One-year mortality was 53.8% (n = 1341). Mortality following a hip fracture was 14.1% (n = 5695) in-hospital (Table 3, Fig. 2). A sub-group analysis of surgical management of hip fractures was also performed. This included 16 studies (n = 4875) [4, 7, 15,16,17,18,19,20,21,22,23,24,25,26,27,28]. One-year mortality following surgical intervention was 51.2% (n = 706). In-hospital mortality was 16.0% (n = 4464) (Table 4, Fig. 3).
Secondary outcomes
Complications following hip fractures in centenarians
Nine studies (n = 340) [4, 7, 16, 17, 19, 28, 30, 32, 33] reported data on the number of patients exhibiting complications for meta-analysis (Appendix 3). Pooled complication rate was 50.5%. Six studies (n = 4244 patients) [17, 25, 27, 28, 32, 33] presented data on post-operative complications. Pneumonia was the most common complication following treatment of hip fracture in centenarians. This occurred in 10.0%. This was followed by urinary tract infection (3.7%), arrhythmia (3.2%), heart failure (2.9%), anaemia (2.8%) and intensive care unit admission (2.3%). Other complications had an incidence of less than 2% (Table 5).
Comorbidities in centenarians with a hip fracture
A total of ten studies (n = 5158 patients) [4, 7, 16,17,18, 27, 28, 31, 33, 34] reported on the number and type of comorbidities observed and presented data to be included in the meta-analysis (Appendix 4).
Dementia was the most commonly reported comorbidity (26.2%), followed by hypertension (15.6%), diabetes (5.5%), and cancer (3.7%). Unspecified cardiovascular disease had a pooled prevalence of 7.5%, but studies reporting this comorbidity did not specify what pathology was observed [7, 17, 33] (Table 6).
Centenarians vs. non-centenarians: co-morbidities
Three studies presented data on comorbid disease prevalence in centenarians and non-centenarians who sustained a hip fracture [26, 29, 31]. Mosfeldt et al. [31] reported centenarians with a hip fracture had a lower median CCI than patients aged 70–99 years with a hip fracture (0 vs 1, P < 0.001). In addition, centenarian were less likely to suffer from renal disease (P = 0.01), congestive heart failure (P = 0.003), diabetes mellitus (P = 0.005), cerebrovascular disease (P = 0.002), peripheral vascular disease (P < 0.001), pulmonary disease (P < 0.001), ulcer disease (P = 0.04), malignancy (P < 0.001), rheumatic disorders (P = 0.002), dementia (P < 0.001), and less likely to use anti-osteoporotic medications (P < 0.001). There were non-statistically significant differences between groups in number of patients with liver disease, myocardial infarction, paralysis, and fracture type. In addition, Blanco et al. [26] found centenarians had a lower incidence of cognitive impairment (P < 0.001) and were taking a lower number of medications (P = 0.034) than patients aged 80–99 years.
It was possible to pool data comparing CCI between patients aged 65–99 years (n = 167,065) and centenarians (n = 1198) in two studies [26, 29]. Charlson Comorbidity Index was significantly lower in centenarians (mean difference − 0.27; 95% CI − 0.11 to − 0.43; I2 81.3%).
Discussion
Knowledge of the mortality associated with hip fracture provides further evidence of the importance of health professionals to hold informed discussions with patients and relatives regarding prognosis following this injury type. However, the majority of studies included in this review exhibited methodological limitations pertaining to low level of evidence and concerns regarding risk of bias. Caution should, therefore, be placed when interpreting these findings.
Due to increasing mortality with age, it is important to ascertain whether hip fractures lead to increased mortality in centenarians. A single study found centenarians with a hip fracture had a lower mean survival time and hospitalization-free survival time than those without a hip fracture [22]. Further research should perform such analysis to more reliably establish the disease-specific mortality associated with hip fracture. Alvarez et al. [35] stratified mortality in centenarians according to degree of frailty. “Robust” and “intermediate” centenarians (higher cognitive and physical capabilities than frail centenarians) had a mortality of less than 10% within a year. A pooled 1-year mortality of 51% was calculated in this meta-analysis. Therefore, centenarians with hip fracture may experience a higher mortality than centenarians without hip fracture. Further research matching centenarians with hip fracture and autonomous centenarians without a hip fracture is required to validate this hypothesis.
Current evidence suggests centenarians suffering from a hip fracture have a higher pre-injury functional status [30], lower medication burden [26, 30], and a lower number of comorbidities [26, 29, 31] than their younger peers (with the latter demonstrated by meta-analysis). Individuals suffering from hip fractures are more likely to be ambulatory [7]. This may render centenarians suffering from hip fractures a self-selecting group, with a lower comorbidity burden allowing them to ambulate, and subsequently fall. This may explain the lower prevalence of comorbidities when compared to a random selection of older people [33]. However, we can only draw conclusions based on our study population (centenarians with hip fractures). Our findings are not applicable to centenarians without hip fractures. In addition, they are hindered by the low level of evidence of the studies included in this review.
Dementia was the most commonly reported comorbidity, being present in over a quarter of patients suffering from a hip fracture (26.2%). This is lower than the estimated 40% prevalence in patients over 100 years of age [36]. This may be explained by the fact that centenarians with moderate-severe dementia are mostly dependent on a wheelchair for ambulation, and are hence less susceptible to falls and hip fractures. Hypertension was the second most common comorbidity, with a pooled prevalence of 15.6%. Antihypertensive medication use may predispose fall injuries among older people [37]. Mazzola et al. [22] matched centenarians with and without a hip fracture, and found the former were more likely to be on an antihypertensive agent. However, whether hypertension itself or taking antihypertensive medications are the culprits remains unclear. A lower prevalence of hypertension was noted in this meta-analysis than is usually reported in other population-based studies [38]. Centenarians with multiple morbidities, requiring multiple medications like anti-hypertensives, are more likely to be less ambulatory. Therefore, hypertension as a comorbidity may be under-represented in our study population. Other medications which may increase the risk of falls in the elderly include diuretics, sedatives, hypnotics, antidepressants, benzodiazepines and nonsteroidal anti-inflammatory drugs [39]. Though medication reviews are commonly performed in clinical practice regardless of patient age, these are particularly relevant for centenarians given the detrimental outcomes resulting from fractures.
Pneumonia was the most common complication following treatment of hip fracture in centenarians, occurring in 10.0% of patients. This was followed by urinary tract infection (3.7%). Infective presentations could be attributed to centenarians with hip fractures having a long hospital stay (calculated at 28.95 days on average). Considering infection were the two most common complications, antibiotic prophylaxis in centenarians with a hip fracture may be warranted. Other common complications included arrhythmia (3.2%), heart failure (2.9%), and anaemia (2.8%). These may prompt cardiovascular input. Cases of hip fracture in centenarians are typically complex, with potentially multiple comorbidities and complications. A multidisciplinary approach is required for optimal treatment, with orthogeriatricians’ involvement advocated by European and UK guidelines [40, 41].
Sub-group analysis comparing overall mortality irrespective of treatment, and mortality in patients undergoing surgical repair indicated similar survival and overlapping confidence intervals up to 1 year after the hip fracture. Therefore, surgical repair following a hip fracture may not provide an additional benefit in terms of mortality reduction. A fixed fracture may lead to improved pain management, quality of life, ease of nursing and personal care, which would justify operative intervention. This meta-analysis cannot determine whether surgical repair yields better functional outcomes or lower complication rates than conservative management due to the lack of studies evaluating these parameters in operative and conservative interventions separately. Further study should explore these parameters to ascertain whether non-operative treatment leads to increased functional recovery.
Time-to-surgery was reported in 11 studies. These ranged from 1.6 to 4 days. This is in contrast with current treatment guidelines, which recommend surgery be performed within 24 h of admission [40, 41]. Such delay could be explained by the need for medical optimisation before orthopaedic surgery can be performed on centenarians [42]. However, lack of capacity in the operating theatre and/or ageism may be contributing factors [43]. Only one study reported that, of nine patients, seven were operated within 48 h, whereas the remaining two were delayed due to medical stabilisation. Further work on hip fractures in centenarians should report reasons for delays in time to surgery, given this is a negative prognostic indicator and must be addressed [44].
Our review was limited by the inclusion of studies with varying dates and duration of retrospective periods. As surgical procedures may have changed over the course of long time periods, the mortality data may be affected. In addition, to calculate mortality regardless of treatment, patients who did not undergo surgical repair were included. These patients may have had severe comorbidities or have been at the end of life, which could have increased the mortality figures calculated. Current evidence has limitations which must be improved to increase the understanding of outcomes of fractures in centenarians. Firstly, the vast majority of studies carried a low level of evidence with major concerns regarding their risk of bias. All studies were case series, which is the most feasible study design to evaluate outcomes of fractures in centenarians given the small number of patients reaching this age. To conduct large clinical trials of this population, a national or international network of trial centres would be warranted. Secondly, only two studies reported patient ethnicity [23, 27]. Studies also poorly reported the characteristics of their cohort in relation to concomitant injuries and osteoporotic status. Given that both factors significantly impact on prognosis, this is an important limitation which should be addressed in future study reporting on this population. Thirdly, no studies clarified the time-frame following fracture within which complications were identified. Therefore, it is not possible to determine when these occur following hip fractures in centenarians. Fourthly, 12 studies did not report time-to-surgery. This is a crucial parameter for successful operation and survival, and is particularly important for prognosis in centenarians [44]. Further research should report on this parameter given its impact on prognosis. Finally, there was a very low number of studies reporting outcomes for surgical and conservative management separately. The comparison of these approaches, investigating both mortality but also health-related quality of life, is required to improve understanding on what is the best care for people aged 100 years and older who experience hip fracture.
Conclusion
Hip fractures in centenarians typically involve complex patient presentations with diverse comorbidities. Dementia, hypertension and diabetes are the most common comorbidities in centenarians with a hip fracture. However, the majority of studies included in this review exhibited methodological limitations pertaining to low level of evidence and concerns regarding risk of bias. Therefore, it is difficult to give a more precise description of mortality and comorbidities in centenarians. Effective cross-discipline communication and discussion with patients and carers regarding higher mortality rates are advised.
References
Human Mortality Database, Human Mortality Database. 2020. https://www.mortality.org/Home/Index. Accessed 29 Jun 2023.
Robine JM, Cubaynes S (2017) Worldwide demography of centenarians. Mech Ageing Dev 165:59–67. https://doi.org/10.1016/j.mad.2017.03.004
Allan LM, Ballard CG, Rowan EN, Kenny RA (2009) Incidence and prediction of falls in dementia: a prospective study in older people. PLoS ONE 4:e5521. https://doi.org/10.1371/journal.pone.0005521
Coutinho ESF, Fletcher A, Bloch KV, Rodrigues LC (2008) Risk factors for falls with severe fracture in older people living in a middle-income country: a case control study. BMC Geriatr 8:21. https://doi.org/10.1186/1471-2318-8-21
López-Torres II, Sanz-Ruiz P, Montero-Fernández N, Chana F, Serra-Rexach JA, Benjumea-Carrasco A et al (2020) Surgical treatment of hip fracture in centenarians: complications and independent risk factors of death. Injury 51(1):S25–S29. https://doi.org/10.1016/j.injury.2020.03.053
Dyer SM, Crotty M, Fairhall N, Magaziner J, Beaupre LA, Cameron ID et al (2016) A critical review of the long-term disability outcomes following hip fracture. BMC Geriatr 16:158. https://doi.org/10.1186/s12877-016-0332-0
Kent MJR, Elliot RR, Taylor HP (2009) Outcomes of trauma in centenarians. Injury 40:358–361. https://doi.org/10.1016/j.injury.2008.10.017
Langenhan R, Müller F, Füchtmeier B, Probst A, Schütz L, Reimers N (2022) Surgical treatment of proximal femoral fractures in centenarians: prevalence and outcomes based on a German multicenter study. Eur J Trauma Emerg Surg. https://doi.org/10.1007/s00068-022-02184-7
Herron J, Hutchinson R, Lecky F, Bouamra O, Edwards A, Woodford M et al (2017) The impact of age on major orthopaedic trauma: an analysis of the United Kingdom trauma audit research network database. Bone Joint J 99B:1677–1680. https://doi.org/10.1302/0301-620X.99B12.BJJ-2016-1140.R2
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, The PRISMA et al (2020) statement: an updated guideline for reporting systematic reviews. BMJ 2021:372. https://doi.org/10.1136/bmj.n71
Centre for Evidence-Based Medicine, Oxford Centre for Evidence-Based Medicine: Levels of Evidence (March 2009). 2020. https://www.cebm.ox.ac.uk/resources/levels-of-evidence/oxford-centre-for-evidence-based-medicine-levels-of-evidence-march-2009. Accessed 02 Dec 2022.
Institute of Health Economics, Case Series Studies Quality Appraisal Checklist. 2014. https://www.ihe.ca/research-programs/rmd/cssqac/cssqac-about. Accessed 02 Dec 2022.
Downes MJ, Brennan ML, Williams HC, Dean RS (2016) Development of a critical appraisal tool to assess the quality of cross-sectional studies (AXIS). BMJ Open 6:e011458. https://doi.org/10.1136/bmjopen-2016-011458
Higgins JPT, Green S. Cochrane Handbook for Systematic Reviews of Interventions. 2011. https://handbook-5-1.cochrane.org/front_page.htm, 2011. Accessed 02 Dec 2022.
Forster MC, Calthorpe D (2000) Mortality following surgery for proximal femoral fractures in centenarians. Injury 31:537–539. https://doi.org/10.1016/S0020-1383(00)00049-8
Oliver CW, Burke C (2004) Hip fractures in centenarians. Injury 35:1025–1030. https://doi.org/10.1016/j.injury.2003.10.004
Shabat S, Mann G, Gepstein R, Fredman B, Folman Y, Nyska M (2004) Operative treatment for hip fractures in patients 100 years of age and older: is it justified? J Orthop Trauma 18:431–435. https://doi.org/10.1097/00005131-200408000-00007
Verma R, Rigby AS, Shaw CJ, Mohsen A (2009) Acute care of hip fractures in centenarians—do we need more resources? Injury 40:368–370. https://doi.org/10.1016/j.injury.2008.09.008
Tarity TD, Smith EB, Dolan K, Rasouli MR, Maltenfort MG (2013) Mortality in centenarians with hip fractures. Orthopedics 36:e282–e287. https://doi.org/10.3928/01477447-20130222-15
Ng WX, Kwek EBK. Operative outcomes in centenarians with hip fractures (Abstract). Singapore Health and Biomedical Congress. 2015. Singapore, Singapore.
Buchanan D, Shastri-Hurst N, Odede S, Sonsale P, Banerjee B. Outcome following surgery for proximal femur fractures in centenarians. Am Res J Orthop Traumatol. 2016; 2016(7).
Mazzola P, Rea F, Merlino L, Bellelli G, Dubner L, Corrao G et al (2016) Hip fracture surgery and survival in centenarians. J Gerontol A Biol Sci Med Sci 71:1514–1518. https://doi.org/10.1093/gerona/glw016
Cheung MY, Ho AWH, Wong SH (2017) Operative outcome of Hong Kong centenarians with hip fracture. Hong Kong Med J 23:63–66. https://doi.org/10.12809/hkmj164823
Moore J, Carmody O, Carey B, Harty JA, Reidy D (2017) The cost and mortality of hip fractures in centenarians. Ir J Med Sci 186:961–964. https://doi.org/10.1007/s11845-017-1589-9
Morice A, Reina N, Gracia G, Bonnevialle P, Laffosse JM, Wytrykowski K et al (2017) Proximal femoral fractures in centenarians. A retrospective analysis of 39 patients. Orthop Traumatol Surg Res 103:9–13. https://doi.org/10.1016/j.otsr.2016.09.025
Blanco JF, de Casa C, Sánchez de Vega R, Hierro-Estévez MA, González-Ramírez A, Pablos-Hernández C (2020) Oldest old hip fracture patients: centenarians as the lowest complexity patients. Aging Clin Exp Res 32:2501–2506. https://doi.org/10.1007/s40520-020-01476-5
Ogawa T, Schermann H, Kobayashi H, Fushimi K, Okawa W, Jinno T (2021) Age and clinical outcomes after hip fracture surgery: do octogenarian, nonagenarian and centenarian classifications matter? Age Ageing 50:1952–1960. https://doi.org/10.1093/ageing/afab137
Sarasa-Roca M, Torres-Campos A, Redondo-Trasobares B, Angulo-Castano MC, Gómez-Vallejo J, Albareda-Albareda J (2022) Fractura de cadera en pacientes centenarios, ¿qué podemos esperar? Revista Española de Cirugía Ortopédica y Traumatología 66:267–273. https://doi.org/10.1016/j.recot.2021.04.004
Manoli A, Driesman A, Marwin RA, Konda S, Leucht P, Egol KA (2017) Short-term outcomes following hip fractures in patients at least 100 years old. J Bone Jt Surg Am. 99:e68. https://doi.org/10.2106/JBJS.16.00697
Barceló M, Francia E, Romero C, Ruiz D, Casadermont J, Torres OH (2018) Hip fractures in the oldest old. Comparative study of centenarians and nonagenarians and mortality risk factors. Injury 49:2198–2202. https://doi.org/10.1016/j.injury.2018.09.043
Mosfeldt M, Madsen CM, Lauritzen JB, Jørgensen HL (2019) Centenarian hip fracture patients: a nationwide population-based cohort study of 507 patients. Acta Orthop 90:342–347. https://doi.org/10.1080/17453674.2019.1602386
Dick AG, Davenport D, Bansal M, Burch TS, Edwards MR (2017) Hip fractures in centenarians: has care improved in the national hip fracture database era? Geriatr Orthop Surg Rehabil 8:161–165. https://doi.org/10.1177/2151458517722104
Barrett-Lee J, Barbur S, Johns J, Pearce J, Elliot RR (2021) Hip fractures in centenarians: a multicentre review of outcomes. Ann R Coll Surg Engl 103:59–63. https://doi.org/10.1308/rcsann.2020.0203
Bermejo Boixareu C, Guijarro Valtuena A, Cedeno Veloz AB, Gonzalo Lazaro G, Saez Lopez P, Ojeda-Thies C, et al. Comparison of clinical features and outcomes in different older age groups with hip fracture (Abstract). World congress on osteoporosis, osteoarthritis and musculoskeletal diseases. 2020. Virtual.
Alvarez JA, Medford A, Strozza C, Thinggaard M, Christensen K (2021) Stratification in health and survival after age 100: evidence from Danish centenarians. BMC Geriatr 21:406. https://doi.org/10.1186/s12877-021-02326-3
Beker N, Sikkes SAM, Hulsman M, Tesi N, van der Lee SJ, Scheltens P et al (2020) Longitudinal maintenance of cognitive health in centenarians in the 100-plus study. JAMA Netw Open 3:e200094. https://doi.org/10.1001/jamanetworkopen.2020.0094
Bromfield SG, Ngameni CA, Colantonio LD, Bowling CB, Shimbo D, Reynolds K et al (2017) Blood pressure, antihypertensive polypharmacy, frailty, and risk for serious fall injuries among older treated adults with hypertension. Hypertension 70:259–266. https://doi.org/10.1161/HYPERTENSIONAHA.116.09390
Richmond R, Law J, Kay-Lambkin F (2011) Higher blood pressure associated with higher cognition and functionality among centenarians in Australia. Am J Hypertens 24:299–303. https://doi.org/10.1038/ajh.2010.236
de Jong MR, Van der Elst M, Hartholt KA (2013) Drug-related falls in older patients: implicated drugs, consequences, and possible prevention strategies. Ther Adv Drug Saf 4:147–154. https://doi.org/10.1177/2042098613486829
National Institute for Health and Care Excellence. Hip fracture in adults. 2023. https://www.nice.org.uk/guidance/qs16/chapter/Quality-statements. Accessed 14 Apr 2023.
Wendt K, Heim D, Josten C, Kdolsky R, Oestern HJ, Palm H et al (2016) Recommendations on hip fractures. Eur J Trauma Emerg Surg 42:425–431. https://doi.org/10.1007/s00068-016-0684-3
Escarce JJ, Shea JA, Chen W, Qian Z, Schwartz JS (1995) Outcomes of open cholecystectomy in the elderly: a longitudinal analysis of 21,000 cases in the prelaparoscopic era. Surgery 117:156–164. https://doi.org/10.1016/s0039-6060(05)80079-0
Wyman MF, Shiovitz-Ezra S, Bengel J (2018) Ageism in the health care system: providers, patients, and systems. Contemporary Perspect Ageism 19:193–212. https://doi.org/10.1007/978-3-319-73820-8_13
Liu Z, Du Z, Lu H, Fu Z, Xu H (2022) Delay between admission and surgery as a potential risk factor for postoperative morbidity and mortality in elderly patients with hip fractures: a retrospective study. J Orthop Sci 25:1124–1130. https://doi.org/10.1016/j.jos.2022.07.010
Hogan P, Ferris H, Brent L, McElwaine P, Coughlan T. Characteristics of centenarians in the Irish hip fracture database (Abstract). 67th Annual and Scientific Meeting of the Irish Gerontological Society, Innovation, Advances and Excellence in Ageing. 2019. Cork, Ireland.
Funding
No funding was received to assist with the preparation of this manuscript.
Author information
Authors and Affiliations
Contributions
Conceptualization: DAAL, TS, CBH; methodology: DAAL, TS; database search: DAAL, CKB; study quality assessment: DAAL, CKB; formal analysis and investigation: DAAL; writing—original draft preparation: DAAL; writing—review and editing: TS, CBH; supervision: TS, CBH.
Corresponding author
Ethics declarations
Conflict of interest
On behalf of all authors, the corresponding author states that there is no conflict of interest.
Ethical approval
Not applicable.
Informed consent
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Appendices
Appendix 1: search strategy
Trauma OR orthopaedics OR injury OR fracture.
AND
Centenarian* OR 100 years old.
AND
Outcome* OR discharge OR disab* OR mortality OR management OR treatment OR predisposing OR risk factors OR complication* OR comorbidities OR length of stay.
Deduplicate
Appendix 2: raw data—mortality following hip fractures in centenarians
Study | Mortality |
|---|---|
Oliver and Burke, 2003 [16] | 11.1% in-patient, 33.3% 1-month, 50% 4-month |
López-Torres et al., 2020 [4] | 13.8% in-patient, 21.5% 1-month, 54.2% 1-year |
Morice et al., 2017 [25] | 7.7% in-hospital, 33.3% 3-month, 42.1% after the 1-year |
Sarasa-Roca et al., 2022 [28] | 33.3% in-patient, 41.7% 1-month, 62.5% 6-month, 66.7% 1-year |
Dick et al., 2017 [32] | 30% in-hospital, 30% 1-month, 39% 3-month, 50% 6-month, 77% 1-year |
Mazzola et al., 2016 [22] | 38.8% 6-month, 51.2% 1-year |
Mosfeldt et al., 2019 [31] | 34% 1-month, 49% 3-month, 66% 1-year |
Shabat et al., 2004 [17] | non-op: 75% 1-month, 100% 2-month. Surgical: 5.3% 1-month, 42.1% 6-months, 42.1% 1-year |
Barrett-Lee et al., 2021 [33] | 27% 1-month, 40% 3-month, 55% 1-year |
Moore et al., 2017 [24] | 22% in-patient, 22% 1-month, 71% 1-year |
Bermejo Boixareu et al., 2020 [34] | 20.16% 1-month |
Hogan et al., 2019 [45] | 12.3% in-patient |
Ng and Kwek, 2015 [20] | Surgical: 0 1-month, 0 3-month, 16.7% 6-month, 33.3% 1-year. non-op: 14.3% 1-month, 28.6% 3-month, 42.8% 6-month, 57.2% 1-year |
Tarity et al., 2013 [19] | operative: 15% in-patient, 20% 1-month, 30% 3-month, 45% 6-months, 60% 1-year. Non-op: 100% 3-month |
Barceló et al., 2018 [30] | 41.4% 3-month, 62.1% 1-year |
Cheung et al., 2017 [23] | 8% 1-month, 25% 6-month, 37% 1-year |
Forster and Calthorpe, 2000 [15] | 31% 1-month, 50% 6-month, 56% 1-year |
Verma et al., 2009 [18] | 17.3% in-patient |
Ogawa et al., 2021 [27] | 3.2% in-patient |
Manoli et al., 2017 [29] | 7.4% in-patient |
Langenhan et al., 2022 [7] | 18.8% in-patient, 27.1% 1-month, 42.4% 3-month, 55.3% 6-month, 61.2% 1-year |
Blanco et al., 2020 [26] | 8.3% in-patient, 8.9% 1-month, 40% 1-year |
Buchanan et al., 2016 [21] | 34.4% in-patient, 31.3% 1-month, 62.5% 4-month |
Appendix 3: raw data—complications observed in centenarians with a hip fracture
Study | Complication rate | Complications observed |
|---|---|---|
Oliver and Burke, 2003 [16] | 11.1% | Not reported |
López-Torres et al., 2020 [4] | 16.9% | Not reported |
Morice et al., 2017 [25] | Not reported | Early dislocation of bipolar hip prothesis (3), surgical-site infection (2), heart failure (1), delirium (2), pneumonia (2), and pyelonephritis (2) |
Sarasa-Roca et al., 2022 [28] | 100% | Pneumonia (4), respiratory insufficiency (4), heart failure (5), anaemia (6), pulmonary oedema (1), arrhythmia (1), acute kidney injury (2), portal hypertension (1), prosthetic dislocation (1) |
Dick et al., 2017 [32] | 71% | Urinary tract infection (5), pneumonia (10), coronary heart disease (2), atrial fibrillation (2), deep vein thrombosis (1), cardiac arrest (1) |
Shabat et al., 2004 [17] | 21.7% | wound hematoma (2), urinary tract infection, arrhythmia (2) |
Barrett-Lee et al., 2021 [33] | 46.5% | urinary tract infection (3), acute kidney injury (3), anaemia (2), pneumonia (7), arrhythmia (1), gastrointestinal bleed (1), pulmonary oedema (1), surgical-site infection (1), transient ischaemic attack (1), |
Tarity et al., 2013 [19] | 43% | Not reported |
Barceló et al., 2018 [30] | 97% | Not reported |
Ogawa et al., 2021 [27] | Not reported | respiratory complications (161), heart failure (120), coronary heart disease (65), stroke (35), pulmonary embolism (16), renal failure (19), intensive care unit admission (145), surgical site hematoma (22) |
Langenhan et al., 2022 [7] | 28.2% | Not reported |
Appendix 4: raw data—comorbidities in centenarians with a hip fracture
Study | Comorbidities (number of patients) |
|---|---|
Oliver and Burke, 2003 [16] | Dementia (5), heart failure (5), breast cancer (1) |
López-Torres et al., 2020 [4] | Hypertension (43), dementia (27), osteoarthritis (15), heart failure (14), cancer (13), cerebrovascular disease (11), type 2 diabetes mellitus (11), atrial fibrillation (10) |
Sarasa-Roca et al., 2022 [28] | Dementia (6), stroke (4), coronary heart disease (1), cancer (1), depression (1) |
Mosfeldt et al., 2019 [31] | heart failure (85), coronary heart disease (21), type 2 diabetes mellitus (11), cerebrovascular disease (50), peripheral vascular disease (6), pulmonary disease (12), peptic ulcer (18), cancer (23), rheumatoid arthritis (6), dementia (16), renal disease (2), liver disease (1), |
Shabat et al., 2004 [17] | Hypertension (11), cardiovascular disease (8), type 2 diabetes mellitus (10), Parkinson's disease (13), dementia (15) audio visual impairment (17) |
Barrett-Lee et al., 2021 [33] | heart disease (16), respiratory disease (4), chronic kidney disease (23), dementia (16) |
Bermejo Boixareu et al., 2020 [34] | dementia (83) |
Verma et al., 2009 [18] | Heart disease (6), pneumonia (1) |
Ogawa et al., 2021 [27] | Coronary heart disease (55), heart failure (640), peripheral vascular disease (23), cerebrovascular disease (301), dementia (811), pulmonary disease (172), connective tissues disease (3), peptic ulcer (140), type 2 diabetes mellitus (267), renal disease (131), cancer (75), liver disease (3), hypertension (1627), coronary heart disease (331), Parkinson's Disease (16), anaemia (179) |
Langenhan et al., 2022 [7] | Dementia (47), hypertension (60), type 2 diabetes mellitus (22), cardiovascular disease (58), cancer (12), pulmonary disease (5) |
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Abelleyra Lastoria, D.A., Benny, C.K., Smith, T. et al. Outcomes of hip fracture in centenarians: a systematic review and meta-analysis. Eur Geriatr Med 14, 1223–1239 (2023). https://doi.org/10.1007/s41999-023-00866-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s41999-023-00866-y