Abstract
Introduction
Pediatric data for phenylephrine, a decongestant used in cold medicines, are limited. This study characterized the pharmacokinetics and metabolism of phenylephrine HCl in children aged 2–17 years.
Methods
Forty-one children experiencing nasal congestion were dosed orally with phenylephrine HCl from 2.5 to 10 mg using a modified weight–age schedule. Plasma from blood samples collected up to 4.5 h after dosing was analyzed for phenylephrine. Urine collected over 24 h was analyzed for phenylephrine and metabolites. Blood pressure and pulse were measured after each blood sampling, and electrocardiograms were recorded before and after dosing. Pharmacokinetic parameters were estimated using noncompartmental methods.
Results
Mean phenylephrine total exposure (AUC∞) for children aged 2–5, 6–11, and 12–17 years was 672, 830, and 1020 pg∙h/mL, and mean maximum concentration (Cmax) was 477, 589, and 673 pg/mL, respectively. Times to peak concentration (Tmax) ranged from 0.17 to 1.5 h, and elimination half-life (t½,β) was short from 1.2 to 1.6 h. Oral clearance (CL/F) increased with age, but with allometric scaling for body size, this trend reversed as scaled clearance (CL/F,scaled) was modestly higher in youngest children. No clinically relevant changes in vital signs or electrocardiograms were observed.
Conclusion
A dosing schedule with additional weight–age increments would provide more consistent systemic concentrations as children age and receive the next higher dose. No developmental delays in clearance mechanisms were apparent when oral clearance was scaled for body size. Phenylephrine pharmacokinetics and metabolism were consistent with adult data, although AUC∞ for the youngest group and Cmax for all pediatric groups were lower. Single doses of phenylephrine HCl were well tolerated.
Trial Registration
Clintrials.gov NCT00762567, registered 30 September 2008.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Why was the study carried out? |
A dosing schedule with additional weight–age increments can provide more consistent systemic concentrations as children age and receive the next higher dose. |
What was learned from the study? |
No developmental delays in clearance mechanisms were apparent when oral clearance was scaled for body size. |
The modest decline in scaled oral clearance across the ages from 2 to 17 years may be related to differences in phenylephrine doses administered and their susceptibility to high-first pass effects in the gastrointestinal tract. |
Single oral doses of phenylephrine in this pediatric population were well tolerated. |
Introduction
Phenylephrine hydrochloride (HCl) is indicated for over-the-counter (OTC) use by children and adults for the temporary relief of nasal congestion due to the common cold, hay fever, or other upper respiratory allergies. Its mechanism of action is constriction of blood vessels mainly located in the nasal passages, resulting in decreased blood volume and a decrease in the volume of the nasal mucosa [1, 2]. Although phenylephrine has been used therapeutically worldwide for many years, no pediatric pharmacokinetic data are available. Therefore, this study was conducted to characterize the pharmacokinetics and metabolism of phenylephrine in children and adolescents, aged 2–17 years.
Another purpose of this study was to explore whether a modified weight- and age-based dosing schedule for phenylephrine achieves similar systemic exposure (Cmax and AUC∞) across this pediatric age range. Historically, pediatric dosing has been empirically based on age because pharmacokinetic data were not available. The US monograph regarding product label directions for OTC decongestants and other cold medicines indicates the doses for children aged 2–5 and 6–11 years are ¼ and ½ the adult dose, respectively, whereas the dose for adolescents aged 12–17 years is the same as the adult dose [3]. However, since 2008, the label on OTC medicines containing phenylephrine and other cold medicines intended for children was changed to state, “Do not use for children < 4 years of age.”
Methods
Study Design and Subjects
Children aged 2–11 years and adolescents aged 12–17 years were eligible if they were between the > 5th and < 95th percentile for weight and had a body mass index > 5th and ≤ 90th percentile based on age and sex. The protocol planned to enroll 24 children and 12 adolescents who were experiencing nasal symptoms due to respiratory allergies, but who were otherwise healthy. Prospective subjects were screened by medical history, physical examination, clinical laboratory profile, and vital signs (temperature, pulse, and blood pressure). Females who had reached menarche needed a negative urine pregnancy test at screening and before dose administration on the study day. Prospective subjects were excluded if they had a history or presence of any clinically significant disease or other systemic condition; a known sensitivity or allergy to phenylephrine; taken any prescription or nonprescription medications within 7 days or monoamine oxidase inhibitors within 2 weeks before the study start date; or a history of drug, alcohol, or tobacco use.
Clinical Protocol
Children began a food fast after midnight on the night before dosing. They were permitted to drink 4 oz of water or low- or no-fat milk and consume a specified light breakfast (one or two slices of toast with a pat of butter or serving of jelly, or a bowl of nonsweetened cereal) no less than 2 h before being admitted to the clinical research unit. Children aged 2–4 years remained in the unit until at least 6 h after the dose of phenylephrine, whereas children aged 5–11 years and adolescents aged 12–17 years remained sequestered for 24 h after the dose. A parent or legal guardian stayed with a child throughout the study’s duration.
The dosing schedule had five increments of doses based on age and weight for children aged 2–11 years weighing from 24 to 95 pounds (11–43 kg) and one dose for adolescents aged 12–17 years (Table 1). This modified schedule included more weight–age increments than the US OTC monograph for phenylephrine and other cough, cold, and allergy ingredients, but comparable increments to the pediatric dosing schedule of OTC analgesics. Study personnel administered the commercial phenylephrine HCl liquid (2.5 mg/5 mL) using an oral syringe. Children aged 2–11 years received a single dose of 2.5–7.5 mg phenylephrine based on actual body weight, and adolescents received a single dose of 10 mg phenylephrine HCl as 20 mL liquid. After swallowing the liquid dose, children aged 2–5 years drank 2 oz water, children 6–11 years drank 4 oz, and adolescents 12–17 years drank 6 oz.
An indwelling catheter was inserted after application of a topical anesthetic from which 3-mL blood samples were collected at 10, 20, 30, and 45 min and at 1, 1.5, 2, 2.5, 3, and 3.5 h after the phenylephrine dose. For children who were > 6 years of age, an additional blood sample was collected at 4.5 h. The blood samples were collected into K3EDTA tubes, gently mixed, and centrifuged at approximately 3000g for about 10 min at 4 °C. The harvested plasma was stored in polypropylene cryovials at −70 °C until assayed. Urine was collected from children aged ≥ 5 years and adolescents approximately 15 min before the phenylephrine dose was administered to serve as a blank. All urine was collected throughout 24 h after the dose. The total amount collected was measured by weight, and two 25-mL aliquots were transferred and frozen at −70 °C until assayed.
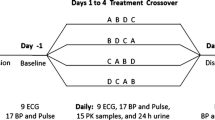
For safety monitoring, blood pressure and pulse were measured before dosing and immediately after each blood sample. Additionally, 12-lead automatic ECGs were recorded before dosing and approximately 40 min after the dose, near the expected maximum phenylephrine plasma concentration. Adverse events were collected during the study beginning at the signing of informed consent and ending when subjects were discharged from the clinic. They included spontaneous reports from subjects and parents, and reports by asking subjects to respond to a nonleading question, such as “How do you feel?”. Children were clinically assessed at the end of the study, which was defined as after the last blood sample (3.5 h after the dose) for children aged 2–4 years and after the 24-h urine collection for children and adolescents aged 5–17 years.
Plasma and Urine Sample Assays
Plasma was assayed directly for unconjugated phenylephrine using a commercial, validated, high-performance liquid chromatography method with tandem mass spectrometry (LC–MS/MS) by PPD Development (Middleton, Wisconsin) [4]. The nominal range of linearity was 10.0–2500 pg/mL. On the basis of quality control (QC) samples run during validation, interday variability was ≤ 11.6%, and interday accuracy ranged from 4.08% to 10.6%. Precision, expressed as percent coefficients of variation (%CV) for the standard curves and QC samples run during the sample assays, ranged from 4.54% to 7.33% and 3.53% to 6.93%, respectively.
Urine samples were analyzed for phenylephrine and metabolites using commercial, validated LS–MS/MS methods by PPD Development: Method P956.00 for unconjugated phenylephrine (PE) and phenylephrine-glucuronide (PE-G), Method P957.00 for 3-hydroxymandelic acid (3-HMA), and Method P958.00 for total PE [5,6,7]. The nominal range of linearity for unconjugated PE and PE-G was 2.0–200 ng/mL, and for 3-HMA and total PE it was 100–5000 ng/mL. The interday variabilities were ≤ 11.0% and interday accuracies ranged from −9.43% to 3.9% across the three assay validations based on assay of QC samples. Precision for standard curves and QC samples run during the sample assays ranged from 1.41% to 7.55% and 2.15% to 5.88% for unconjugated PE, from 2.36% to 9.60% and 5.60% to 9.81% for PE-G, and from 1.56% to 7.40% and 2.42% to 8.45% for 3-HMA. Only one standard curve was generated for total PE.
Pharmacokinetic Analysis
Plasma concentration–time data for phenylephrine were analyzed by noncompartmental methods using Phoenix WinNonlin, Version 6.3 (Pharsight, a Cetera Company). Actual blood sampling timepoints were used in the analysis. Plasma concentrations below the lower limit of quantitation that occurred before and after the maximum concentration were imputed as zero and missing, respectively. A predose blood sample was not collected to limit the number of samples taken per child; therefore, the pharmacokinetic data analysis included the assumption of 0 pg/mL phenylephrine at zero time.
The maximum plasma concentration (Cmax) and the time at which the maximum occurred (Tmax) were determined from individual plasma concentration–time profiles. The terminal elimination rate constant (β) was estimated using linear least-squares regression of the terminal phase of the log concentration–time profile. The terminal elimination half-life (t½,β) was obtained as 0.693/β. Area under the plasma concentration–time curve up to the last observed quantifiable concentration (AUCtlast) was determined using the linear trapezoidal rule. Area under the plasma concentration–time profile from zero to infinite time (AUC∞) was the sum of AUCtlast and the extrapolated area based on the ratio of the last quantifiable plasma concentration and terminal rate constant (Cp/β).
Oral clearance (CL/F) and terminal volume of distribution (Vz/F), both uncorrected for bioavailability (F), were determined as dose/AUC and dose/(AUC*β), respectively. The doses of free base phenylephrine were used in the latter calculations, which were obtained by multiplying by 0.821. In addition, the observed CL/F and Vz/F were allometrically scaled by body weight (BW) to a 70-kg adult using the approach outlined by Anderson et al.: CL/F,scaled = (CL/F)/(BW/70 kg)3/4 and Vz/F,scaled = (Vz/F)/(BW/70 kg) [8].
The amounts of unconjugated phenylephrine and three of its metabolites excreted in the urine were determined as percentages of the administered dose (PDx) using the following methods. First, the amounts of unconjugated PE and the PE-G and 3-HMA metabolites were calculated by multiplying assayed concentrations by the total urine volume collected over 24 h. They were converted into micromoles (μmol) using the appropriate molecular weights. The amount of PE-S excreted was estimated indirectly because it could not be synthesized and assayed directly in urine. An aliquot of urine sample was digested with sulfatase, and the concentration of total PE was assayed. After multiplying by the total urine volume collected over 24 h and converting to micromoles, the amount of PE-S was estimated using the following equation: PE-S (μmol) = total PE (μmol) – unconjugated PE (μmol) − PE-G (μmol).
Safety Assessments
Adverse events were evaluated by incidence, severity, and relationship to study drug. Serial measurements of blood pressure and pulse were reviewed as well as ECG recordings before and after dosing. The ECG device estimated Bazett-corrected QT interval (QTcB) and automatically interpreted the ECG data using pediatric settings. The principal investigator reviewed the ECG tracings for clinical significance. Study personnel recorded abnormal predose ECG readings as significant medical history and abnormal postdose ECG reading as adverse events. However, if an abnormal postdose ECG finding was consistent with the abnormal predose ECG finding, the postdose reading was not reported as an adverse event.
Statistics
The statistical analysis was conducted using SAS version 9.2, Windows 10 (SAS Institute, Cary, NC). Descriptive statistics were calculated for the pharmacokinetic and safety data, and summarized by three pediatric age groups commonly used for dosing OTC pediatric products: 2–5 years, 6–11 years, and 12–17 years. The data included individual phenylephrine concentration–time data; plasma (phenylephrine) and urinary (phenylephrine, PE-S, PE-G, 3-HMA) pharmacokinetic parameters; screening and postdose clinical assessment parameters; serial measurements of blood pressure and pulse; and ECG parameters. The relationships of observed and scaled CL/F with age were assessed using linear regression analysis. Least-squares estimates of the intercept and slope and their associated standard errors and p values were obtained. An age-related change was concluded if the p value associated with the slope was < 0.05 for a two-sided test.
Fridericia-corrected QT interval values (QTcF), which were obtained by correcting machine-generated QTcB values using the Fridericia formulae, were tabulated along with changes from baseline (postdose minus predose). The number and percentages of children with QTcF values that fell within adult categories (0 to ≤ 450 ms, > 450 to ≤ 480 ms, > 480 to ≤ 500 ms, and > 500 ms) and with increases in QTcF values that fell within adult categories (≤ 30 ms, > 30 to ≤ 60 ms, and > 60 ms) were reported by the three age groups.
Results
Subject Disposition
This study was conducted at West Coast Clinical Trials (Cypress, CA) between September and November 2008. Forty-one children and adolescents with nasal symptoms due to respiratory allergies were enrolled. The subjects included 16 males and 25 females, of which the majority were either Black (65.9%) or Hispanic (22.0%). Consent was withdrawn for one female subject in the youngest age group after receiving the phenylephrine dose because she was not able to comply with the pharmacokinetic blood collections. Demographic information for subjects who completed the study is summarized in Table 2. Data from all subjects were included in the safety analysis.
Pharmacokinetic Analysis
Mean pharmacokinetic parameters of phenylephrine for the children’s age groups (2–5 years and 6–11 years) and adolescent age group (12–17 years) are summarized in Table 3. Mean Cmax and AUC∞ increased from the youngest to the oldest age group, whereas the dose-independent parameters of Tmax and t½,β were similar among the groups. Mean plasma phenylephrine concentration–time profiles shown in Fig. 1 are consistent with this trend.
The linear relationships of oral clearance (observed and scaled) and age are illustrated in Fig. 2. Observed oral clearance (CL/F,obs) increased with increasing age owing to larger body sizes. However, the opposite trend with age became apparent with allometric scaling of oral clearance for body size (CL/F,scaled), [8]. Volume of distribution was scaled for body size directly by multiplying by the ratio of the child’s weight to a 70 kg adult (Vd/F,scaled). No trends with increasing age or among age group means were observed (Table 3). However, mean values for the two youngest groups were more variable, having coefficients of variability of 39% and 49%, than the oldest group, which also had the lowest mean value after scaling.
On average, about 50% of the phenylephrine HCl dose was recovered from urine collected over 24 h. Mean percentages of phenylephrine and three metabolites per dose are summarized in Table 4 by age group. Urine excretion data were obtained from only two 5-year-old children in the youngest age group, so data for each subject are reported in the table without summary statistics.
Safety
Twelve treatment-emergent adverse events were experienced by nine children. Eight of the 12 adverse events were obtained from abnormal postdose ECG readings, and the remaining included two reports of somnolence and one report each of vasovagal syncope and nausea. Using standard regulatory terms to assess relatedness to study treatment, the clinical investigator deemed the two reports of somnolence as related to phenylephrine, whereas she deemed the remaining ten adverse events as doubtful or not related to treatment. Only one adverse event, somnolence, was reported for one child in the 2–5-year age group.
Mean systolic and diastolic blood pressure and pulse measured before and up to 4.5 h after the phenylephrine dose are shown by age group in Fig. 3. No clinically relevant changes in blood pressure, pulse, or physical examination findings were observed during the study. None of the automatic, pre- and postdose abnormal ECG readings was deemed clinically significant. From the postdose ECG data, eight observations for six subjects were reported as adverse events. In the 6–11-year age group, the events were sinus bradycardia, right ventricular hypertrophy, supraventricular extrasystoles, and ECG ST segment elevation. In the 12–17-year age group, the events were sinus bradycardia, supraventricular arrhythmia, ECG ST segment elevation, and abnormal QRS axis. The investigator classified these events as not clinically significant and assessed the causality as not related or doubtful relationship to phenylephrine. One subject had a repeat postdose ECG recording to confirm the investigator’s clinical interpretation; the latter ECG was normal.
QTcF values were calculated for this study, because a published study of 781 children aged 10–18 years indicates that QTcB overcorrects QT data in the pediatric age group, as systematic variations in the QTcB with both age and heart rate in normal children are observed [9]. One child had a pre- and postdose QTcB of 461 ms (QTcF of 475 ms); no other child had a pre- or postdose QTcB or QTcF value > 450 ms or an increase > 30 ms. Because there is no consensus on the upper limits of these categories for the pediatric population, these results should be considered within this context.
Discussion
Current pediatric doses of OTC cough and cold ingredients, including phenylephrine, are 1/4 and 1/2 fractions of the adult doses, which were intended to adjust for differences in body sizes among adults and children ages 2–5 years and 6–11 years, respectively. In this study, which is the first to characterize the pharmacokinetics of phenylephrine in children, three fractional doses were added to the pediatric dosing schedule (Table 1) to narrow the range of systemic drug exposure despite a large variation in body size. The adolescent age group received the 10-mg adult dose. Indeed, these phenylephrine HCl doses achieved mean total exposures (AUC∞) and maximum exposures (Cmax) that differed only about 1.5-fold across the pediatric age groups, even though they extended over a fourfold range (2.5–10 mg) provided by the modified dosing schedule. The dose-independent parameters, Tmax and t½,β, reflected rapid absorption and elimination of phenylephrine, respectively, and they were similar among groups.
Mean AUC∞ for children aged 6–11 years and adolescents were within the range of mean values (816–1916 pg h/mL) reported for the 10-mg therapeutic dose of phenylephrine HCl across adult studies; whereas AUC∞ for children aged 2–5 years fell below the range despite the higher dose added for older children in this age group [10,11,12]. All mean Cmax fell below the range of mean adult values (874–1600 pg/mL). The lower Cmax observed in children may be partially due to fewer blood samples collected after the dose compared with adults. The rapid absorption of phenylephrine, reaching maximum concentrations typically within 20 min, requires the collection of several samples within a short period to capture the maximum concentration more reliably. Also of note is the high degree of intersubject variability for both AUC∞ and Cmax in children and adults, which is characteristic of drugs, including phenylephrine, that undergo high first-pass metabolism and have relatively low bioavailability.
The observed oral clearance, CL/F,obs, of phenylephrine increased with age mainly owing to increasing body size. However, developmental differences in metabolic activities, especially in very young children, may contribute to age-related differences in oral clearance, whereas fluctuations in sex and growth hormones may affect metabolic activities in adolescents [13]. Scaling oral clearance using the allometric ¾-power model of body weight is often informative when comparing clearance data among pediatric age groups, because differences in metabolism, where they may exist, would become apparent [8]. For phenylephrine, allometric scaling of oral clearance showed an inverse relationship with age. CL/F,scaled was modestly higher for the youngest children, suggesting no maturation delays in phenylephrine metabolism or other clearance mechanism. Additionally, CL/F,scaled for adolescents was comparable to CL/F (154 ± 42 L/min) estimated in adults [12].
The modest decline in CL/F,scaled across the ages from 2 to 17 years may be related to differences in the doses administered and their susceptibility to high-first pass effects in the gastrointestinal tract. In adults, AUC∞ increased more than proportionally and oral clearance was lower with increasing phenylephrine doses from 10 to 30 mg [12]. For children aged 2–5 years who received the lowest doses (2.5–3.75 mg), more phenylephrine may be metabolized when passing through the intestinal wall, resulting in lower bioavailability and higher CL/F,scaled compared with children aged 6–11 years and adolescents who received higher doses (5–7.5 mg and 10 mg, respectively).
The principal routes of phenylephrine metabolism are sulfate conjugation (mainly in the intestinal wall) and oxidative deamination by both the A and B forms of monoamine oxidase [14, 15]. Glucuronidation has also been reported as a metabolic pathway. Overall, the urine metabolite pattern was similar for children aged 6–11 and 12–17 years. Mean percentages of the dose excreted as phenylephrine, PE (0.36% and 0.30%, respectively), were low and as the glucuronide, PE-G, were negligible for both groups. Mean percentages for the sulfate, PE-S (22.1% and 18.6%, respectively) were slightly lower than those for 3-HMA (27.6% and 22.3%, respectively). In an adult study, mean percentages of phenylephrine and its metabolites excreted in urine for the therapeutic 10-mg dose were 0.44%, PE; 0.033%, PE-G; 46.6% PE-S; and 25.3%, 3-HMA [12]. The percentages of dose excreted as PE, PE-G, and 3-HMA by children and adults were within the same range. However, only about 50% of the administered dose was recovered in 24 h because total collection of urine is more difficult to achieve in a pediatric population. The lower percentage of excreted dose compared with 72% in adults would account for some of the differences.
A single oral dose of phenylephrine HCl liquid was well tolerated with few treatment-related adverse events reported. Because the mechanism of action of phenylephrine involves vasoconstriction, subjects were comprehensively monitored for potential cardiovascular adverse events in this study. Overall, the cardiovascular assessments of pulse and blood pressure up to 4.5 h showed no clinically important changes following the dose. None of the abnormal ECG readings was deemed clinically significant or related to phenylephrine.
Evaluation of potential adverse events of phenylephrine associated with the central nervous system (i.e., headache, dizziness, and nervousness) relied on spontaneous reporting or responses to the nonleading question, “How do you feel?”. The lack of specific monitoring or assessment procedures for these adverse events is a limitation of this study. Given that children are often treated with multiple doses of cold medicines containing this ingredient over a few days, another limitation is that the safety of phenylephrine was evaluated after a single dose. Nevertheless, phenylephrine has a short elimination half-life such that it will not accumulate systemically with multiple dosing.
Conclusion
The modified weight–age dosing schedule for phenylephrine HCl evaluated in this study extended over a fourfold range of doses, providing AUC∞ and Cmax that increased only about 1.5-fold across pediatric age groups. More weight–age increments can decrease oscillations in AUC∞ and Cmax exposures across the three pediatric age groups, providing more consistent systemic concentrations as children age and receive the next higher dose. Oral clearance increased with age, but with allometric scaling for differences in body size, no developmental delays in the metabolism or other clearance mechanisms of phenylephrine were apparent. Adolescents had comparable systemic exposure, AUC∞, and oral clearance with adults following the 10-mg dose. The single doses of phenylephrine HCl were well tolerated in this study.
References
Johnson DA, Hricik JG. The pharmacology of α-adrenergic decongestants. Pharmacotherapy. 1993;12:110S-115S.
Hoffmann, Empey DW, Medder KT. Nasal decongestants. Drugs. 1981;21:438-43
Food and Drug Administration. Establishment of a monograph for OTC cold, cough, allergy, bronchodilator and antiasthmatic products. Fed Regist. 1976;41:38312–424.
Method P898. Quantitation of unconjugated phenylephrine in human plasma via HPLC with MS/MS detection, Issued Feb 2009. Middleton: PPD Bioanalytical Laboratory.
Method P956. Quantitation of phenylephrine and phenylephrine glucuronide in human urine via HPLC with MS/MS detection. Issued Feb 2009. Middleton: PPD Bioanalytical Laboratory.
Method P957. Quantitation of 3-hydroxymandelic acid in human urine via HPLC with MS/MS detection. Issued Feb 2009. Middleton: PPD Bioanalytical Laboratory.
Method P958. Quantitation of total phenylephrine in human urine via HPLC with MS/MS detection. Issued Feb 2009. Middleton: PPD Bioanalytical Laboratory.
Anderson BJ, Woolard GA, Holford NH. A model for size and age changes in the pharmacokinetics of paracetamol in neonates, infants, and children. Br J Clin Pharmacol. 2000;50:125–34.
Pearl W. Effects of gender, age, and heart rate on QT intervals in children. Pediatr Cardiol. 1996;17:135–6.
Ptacek P, Macek JK. Development and validation of a liquid chromatography–tandem mass spectrometry method for the determination of phenylephrine in human plasma and its application to a pharmacokinetic study. J Chromatogr B. 2007;858:263–8.
Atkinson HC, Stanescu I, Salem II, Potts AL, Anderson BJ. Increased bioavailability of phenylephrine by co-administration of acetaminophen: results of four open-label, crossover pharmacokinetic trials in healthy volunteers. Eur J Clin Pharmacol. 2015;71:151–8.
Gelotte CK, Zimmerman BA. Pharmacokinetics, safety, and cardiovascular tolerability of phenylephrine HCl 10, 20, and 30 mg after a single oral administration in healthy volunteers. Clin Drug Investig. 2015;35:547–58.
Kearns GL, van den Anker JN. Adolescents and drug development: commentary on a dawning paradigm shift. J Clin Pharmacol. 2021;61(6):740–3.
Ibrahim KF, Medgley JM, Crowley JR, Williams CM. The mammalian metabolism of R-(−)-m-synephrine. J Pharm Pharmacol. 1983;35:144–7.
Suzuki O, Matsumoto T, Oya M, Katsumata Y. Oxidation of synephrine by type A and type B monozmine oxidase. Experentia. 1979;35:1283–4.
Acknowledgements
Funding
This study was sponsored by McNeil Consumer Healthcare, a Division of Johnson & Johnson Consumer, Inc. (Fort Washington, PA, USA), which provided all research funding, including the journal’s Rapid Service Fee.
Editorial assistance
Kathleen Boyle, PhD, from KE Boyle Consultants, LLC (Exton, PA, USA) provided editorial assistance for this manuscript, and this support was funded by McNeil Consumer Healthcare.
Author contributions
The authors’ contributions are as follows: concept and study design (DAP, CKG), study conduct oversight (DAP), pharmacokinetic analysis (CKG), statistical analysis (BAZ), interpretation of results (CKG, DAP, BAZ), initial draft of manuscript (CKG), and revisions and approval of the final manuscript (CKG, DAP, BAZ).
Disclosures
Cathy Gelotte, Dolly Parasrampuria, and Brenda Zimmerman were employees at the time the study was conducted, and they all currently hold stock or stock options in Johnson & Johnson. Cathy Gelotte, a retired employee, continues to be a paid consultant to Johnson & Johnson Consumer, Inc.
Compliance with ethics guidelines
The study was conducted in accordance with guidelines of the International Conference on Harmonisation–Good Clinical Practice and applicable local regulatory requirements and laws on clinical research involving human subjects. The protocol and informed consent form were reviewed and approved by the Compass Institutional Review Board (Mesa, Arizona, USA). All subjects and their parents or legal guardian were informed of the nature and purpose of the study before any screening procedures. A parent or legal guardian provided written informed consent for a child to participate in the study, and written assent was obtained from children ≥ 6 years old.
Data availability
Supporting data for this Phase 1 study is not currently available for public access, and resides with the study sponsor.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Gelotte, C.K., Parasrampuria, D.A. & Zimmerman, B.A. Single-Dose Pharmacokinetics and Metabolism of the Oral Decongestant Phenylephrine HCl in Children and Adolescents. Pulm Ther 9, 139–150 (2023). https://doi.org/10.1007/s41030-022-00206-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s41030-022-00206-8