Abstract
Ectopic pancreatic tissue is called pancreatic choristoma or heterotopia of pancreas. It is a rare entity. We present a case of advanced Ca ovary with omental pancreatic choristoma.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Pancreatic choristoma is a congenital anomaly. Herein, the pancreatic tissue without any anatomical or vascular connections to the main pancreas is found in ectopic location. It is relatively a rare entity, found at laparotomy with an incidence of 0.2% (Elpek 2007).
The pancreatic choristoma can be found in various anatomical sites such as the stomach, duodenum, jejunum, gallbladder, esophagus, common bile duct, spleen, mesentery, mediastinum, lungs and fallopian tubes. Stomach is the most common location (25 to 38%), with pancreatic rests most frequently found in the submucosa (75% of cases) (Elhence 2012).
Although ectopic pancreas is usually an incidental finding, they can present with nonspecific symptoms such as abdominal pain, abdominal fullness, nausea, vomiting, anorexia, weight loss, anemia, and melena. Abdominal pain is the most common symptomatic presentation and can be explained by the inflammation and irritation of surrounding tissues secondary to the secretion of pancreatic enzymes and hormones. Pain can also be explained as a result of hemorrhage in the lesion due to mucosal erosion and ulcer formation, especially when it occurs in the small intestine. Patients can also present with symptoms of gastric outlet obstruction especially those greater than 1.5 cm in size. Published literature reports have described rare instances of malignant transformation in the ectopic pancreatic tissue (Pendharkar 2019).
We present a case of pancreatic choristoma in the omentum, in a case of epithelial ovarian Ca.
Case
A 54-year-old lady presented to our OPD with abdominal distension, breathlessness, inability to eat for last 2 months, in the COVID-19 pandemic days, April, 2020. She also gave a longstanding history of dyspepsia, bloating and diarrhea on and off.
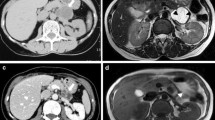
Clinical examination revealed a cachectic lady with a ECOG performance score 2, massive ascites and bilateral pedal edema. Her CA125 value was more than 2000 U/ml at first visit, serum albumin 3.6 g%. PET-CT done elsewhere showed multiple discrete coalescent peritoneal, omental and mesenteric soft tissue deposits with caking, massive ascites, prominent retrocaval, perigastric, intramammary, mediastinal nodes. Ascitic fluid tapping was done and sent for malignant cytology, cell block analysis. The report was positive for malignant cells, adenocarcinoma cells. A working diagnosis of advanced ovarian Ca was made and planned for neoadjuvant chemotherapy followed by interval debulking surgery.
Dose dense weekly Paclitaxel 80 mg/m2 and Carboplatin AUC 2 was administered for 9 weeks, starting from 6/5/2020. At the end of 9 weeks, there was partial clinical response. The massive ascites had become mild ascites but patient had not had much improvement in symptoms of loose motions and dyspepsia. Her CA 125 had decreased from more than 2000U/ml to 246 U/ml. A PET-CT was repeated to assess her response to treatment and revealed partial response to the therapy.
She underwent interval debulking surgery on 15/9/2020.
Laparotomy, TAH + BSO + pelvic peritonectomy and total omentectomy were performed. There was no gross residual disease left at the end of surgery. Her PCI score was 8/39. She had received prophylactic antibiotics, anticoagulants as per hospital protocol (Fig. 1).
During surgery total omentectomy, dissection was difficult near splenic flexure, as there was a residual tumor in the omentum near splenic hilum, of around 5 cm. There were dense adhesions between the tumor mass in omentum and the anterior surface of the pancreas. Complete debulking was done. The first 2 days post-op period was uneventful—with patient on normal diet and ambulating from post-op day 1. On post-op day 3, patient developed one episode of high-grade fever, persistent diarrhea and chest congestion symptoms. She was treated symptomatically for next 3 days. Fever had subsided in 24 h but diarrhea persisted. Covid RT-PCR was done twice during the 7 days post-op period. Both the Covid RT-PCR reports were negative. Her white blood counts were on higher side of range, 17,000–21,000/mm3, with neutrophilic leukocytosis all throughout the hospital stay. The inflammatory marker serum procalcitonin (PCT) increased steadily from 5 to 18 ng/ml, from post-op day 6 to 11, (normal value for serum procalcitonin- < 0.5 ng/ml, serum PCT > 2 ng/ml—sepsis, serum PCT values increase post laparotomy). Work up for possible source of sepsis was done, and reports were non-contributory. Patient was started on higher antibiotics for raised PCT. Clinically, patient was not looking as ill as her blood reports. There were no more episodes of fever during her hospital stay. She was discharged on 11th post-op day, ambulating, with symptoms of diarrhea partially subsiding.
The patient returned on POD 14 for suture removal. Wound had healed well. Histopathology showed HGSC ovary with pancreatic choristoma in omentum.
Based on Heinrich’s 1909* classification and the subsequent Gasper-Fuentes modification in 1973, there are four types of pancreatic heterotopia. They are
-
Type I—typical pancreatic tissue with acini, ducts, and islet cells similar to the normal pancreas.
-
Type II (canalicular variety)—pancreatic ducts only.
-
Type III (exocrine pancreas)—acinar tissue only.
-
Type IV (endocrine pancreas)—islet cells only.
Our patient belonged to first type with pancreatic tissue, acini, ducts and islet cells (Fig. 2).
She was advised to complete the adjuvant treatment as advised. She was lost to follow-up after completion of treatment.
Discussion
The clinical presentation of the ectopic pancreas and ovarian carcinoma has many similarities.
Our patient had irritable bowel syndrome for the last 10–12 years. In ovarian cancer, we do find the symptoms of constipation, loose motions, weight loss, bloating sensation, loss of appetite for a few months prior to diagnosis of Ca ovary. Hence, the GI symptomatology was thought to be of ovarian origin, but a bit exaggerated. But retrospectively, we found that watery diarrhea is a less common symptom for Ca ovary than constipation (Fig. 3).
During the postoperative period, patient continued to have diarrhea and pain abdomen in the left hypochondrium, which was attributed to the surgical procedure. The symptom of persistent diarrhea was thought to be due to covid, in the pandemic time. The persistent leukocytosis and elevated serum procalcitonin made us prescribe higher antibiotics during the 11-day hospital stay (Fig. 4).
Omental pancreatic choristoma is a rare occurrence, and the diagnosis was revealed after the patient got discharged!
This case helped us to know about pancreatic choristoma, and the clinical picture could then be correlated with laboratory reports. The raised serum PCT and leukocytosis could be due to inflammation due to choristoma and surgical dissection.
References
Elpek GO, Bozova S, Küpesiz GY, Oğüş M. An unusual cause of cholecystitis: heterotopic pancreatic tissue in the gallbladder. World J Gastroenterol. 2007;13(2):313–5. https://doi.org/10.3748/wjg.v13.i2.313. (PMID: 17226916; PMCID: PMC4065965).
Elhence P, Bansal R, Agrawal N. Heterotopic pancreas in gall bladder associated with chronic cholecystolithiasis. Int J Appl Basic Med Res. 2012;2(2):142–3. https://doi.org/10.4103/2229-516X.106360. (PMID: 23776830; PMCID: PMC3678697).
Pendharkar D, Khetrapal S, Jairajpuri ZS, Rana S, Jetley S. Pancreatic and gastric heterotopia in the gallbladder: a rare incidental finding. Int J Appl Basic Med Res. 2019;9(2):115–7. https://doi.org/10.4103/ijabmr.IJABMR_109_18. (PMID: 31041176; PMCID: PMC6477957).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Sharma, M., Annapurna, V., Sulakshana, M.S. et al. Pancreatic Choristoma in Omentum in Advanced CA Ovary: A Clinical Puzzle. Indian J Gynecol Oncolog 21, 32 (2023). https://doi.org/10.1007/s40944-023-00706-8
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1007/s40944-023-00706-8