Abstract
Purpose
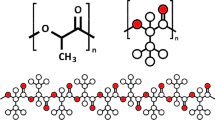
Key natural polymers, known as hydrogels, are an important group of materials in the design of tissue-engineered constructs that can provide a suitable habitat for cell attachment and proliferation. However, in comparison to tissues within the body, these hydrogels display poor mechanical properties. Such properties cause challenges in 3D printing of hydrogel scaffolds as well as their surgical handling after fabrication. For this reason, the purpose of this study is to critically review the 3D printing processes of hydrogels and their characteristics for tissue engineering application.
Methods
A search of Google Scholar and PubMed has been performed from 2003 to February 2022 using a combination of keywords. A review of the types of 3D printing is presented. Additionally, different types of hydrogels and nano-biocomposite materials for 3D printing application are critically reviewed. The rheological properties and crosslinking mechanisms for the hydrogels are assessed.
Results
Extrusion-based 3D printing is the most common practice for constructing hydrogel-based scaffolds, and it allows for the use of varying types of polymers to enhance the properties and printability of the hydrogel-based scaffolds. Rheology has been found to be exceedingly important in the 3D printing process; however, shear-thinning and thixotropic characteristics should also be present in the hydrogel. Despite these features of extrusion-based 3D printing, there are limitations to its printing resolution and scale.
Conclusion
Combining natural and synthetic polymers and a variety of nanomaterials, such as metal, metal oxide, non-metal, and polymeric, can enhance the properties of hydrogel and provide additional functionality to their 3D-printed constructs.
Lay Summary
Essential natural materials, known as hydrogels, are important for the design of tissue-engineered constructs that allow for cells to attach and grow while receiving the nutrients necessary for growth as well. However, in comparison to the cells in the body, the hydrogels have poor functional properties. Because of this, the purpose of this study is to assess the 3D printing processes of the hydrogels, and the appropriate characteristics of the hydrogels that allow this material to be useful in tissue engineering processes. A review of the types of 3D printing is presented, and the different types of materials used for 3D printing are also assessed. Lastly, the properties of hydrogels that make them ideal for 3D printing are reviewed. The most common type of 3D printing is extrusion-based 3D printing. It allows for the use of different types of natural materials to enhance the properties and printing ability for the hydrogel-based cellular environment. The flow of a material is found to be important in 3D printing as well as the consistency and capability of a material. However, there are challenges to the 3D printing quality and size for extrusion-based 3D printing. Overall, different 3D printing techniques should be created to enhance the construction capabilities of 3D printing to meet the most favorable environment for cellular growth and attachment.










Similar content being viewed by others
References
Tahmasbi Rad A, et al. Conducting scaffolds for liver tissue engineering. J Biomed Mater Res, Part A. 2014;102(11):4169–81.
Shabafrooz V, et al. The effect of hyaluronic acid on biofunctionality of gelatin–collagen intestine tissue engineering scaffolds. J Biomed Mater Res, Part A. 2014;102(9):3130–9.
Yazdimamaghani M, et al. Biomineralization and biocompatibility studies of bone conductive scaffolds containing poly (3, 4-ethylenedioxythiophene): poly (4-styrene sulfonate)(PEDOT: PSS). J Mater Sci - Mater Med. 2015;26(12):1–11.
Velasco-Hogan A, Jun X, Meyers MA. Additive manufacturing as a method to design and optimize bioinspired structures. Adv Mater. 2018;30(52):1800940.
Tayebi L, Masaeli R, Zandsalimi K. 3D printing in oral & maxillofacial surgery: Springer International Publishing; 2021
Wang X, et al. 3D printing of polymer matrix composites: a review and prospective. Compos Part B. 2017;110:442–58.
Chen Z, et al. 3D printing of ceramics: a review. J Eur Ceram Soc. 2019;39(4):661–87.
DebRoy T, et al. Additive manufacturing of metallic components–process, structure and properties. Prog Mater Sci. 2018;92:112–224.
Higuchi A, et al. External stimulus-responsive biomaterials designed for the culture and differentiation of ES, iPS, and adult stem cells. Prog Polym Sci. 2014;39(9):1585–613.
Sun W, et al. 3D printing hydrogel-based soft and biohybrid actuators: a mini-review on fabrication techniques, applications, and challenges. Front Robot AI. 2021;8:120.
Liu C, et al. Hydrogel prepared by 3D printing technology and its applications in the medical field. Colloid Interface Sci Commun. 2021;44: 100498.
Entezar-Almahdi E, et al. Integrin receptor mediated pH-responsive nano-hydrogel based on histidine-modified poly (aminoethyl methacrylamide) as targeted cisplatin delivery system. Journal of Drug Delivery Science and Technology. 2021;62: 102402.
Farzanfar J, et al. Assessment of pH responsive delivery of methotrexate based on PHEMA-st-PEG-DA nanohydrogels. Macromol Res. 2021;29(1):54–61.
Luo Y, Zhang T, Lin X. 3D printed hydrogel scaffolds with macro pores and interconnected microchannel networks for tissue engineering vascularization. Chem Eng J. 2022;430: 132926.
Yang HS, Wolcott MP, Kim HS, Kim S, Kim HJ. Effect of different compatibilizing agents on the mechanical properties of lignocellulosic material filled polyethylene bio-composites. Compos Struct. 2007;79(3):369–75.
Tayebi L. Structured membranes for biomedical and tissue engineering applications. Diss: University of Oxford; 2019.
Tabatabaei FS, Torres R, Tayebi L. “Biomedical materials in dentistry.” applications of biomedical engineering. Dentistry. 2020;3-20:22–5.
Wang X, et al. Generation of three-dimensional hepatocyte/gelatin structures with rapid prototyping system. Tissue Eng. 2006;12(1):83–90.
Tayebi L, et al. 3D-printed thick structured gelatin membrane for engineering of heterogeneous tissues. Mater Lett. 2018;217:39–43.
Dehghani S, et al. 3D-Printed membrane as an alternative to amniotic membrane for ocular surface/conjunctival defect reconstruction: an in vitro & in vivo study. Biomaterials. 2018;174:95–112.
Tayebi L, et al. 3D-printed membrane for guided tissue regeneration. Mater Sci Eng, C. 2018;84:148–58.
Kodama H. Automatic method for fabricating a three-dimensional plastic model with photo-hardening polymer. Rev Sci Instrum. 1981;52(11):1770–3.
Jungst T, Smolan W, Schacht K, Scheibel T, Groll J. Strategies and molecular design criteria for 3D printable hydrogels. Chem Rev. 2016;116(3):1496–539.
Tayebi L, Moharamzadeh K, editors. Biomaterials for oral and dental tissue engineering: Woodhead Publishing; 2017.
Jang TS, Jung HD, Pan HM, Han WT, Chen S, Song J. 3D printing of hydrogel composite systems: recent advances in technology for tissue engineering. Int J Bioprinting. 2018;4(1):27–46.
Nikpour P, et al. Dextran hydrogels incorporated with bioactive glass-ceramic: nanocomposite scaffolds for bone tissue engineering. Carbohyd Polym. 2018;190:281–94.
Donato RK, Mija A. Keratin associations with synthetic, biosynthetic and natural polymers: an extensive review. Polymers. 2019;12(1):32.
Pederson AW, Ruberti JW, Messersmith PB. Thermal assembly of a biomimetic mineral/collagen composite. Biomaterials. 2003;24(26):4881–90.
Yang X, et al. Collagen-alginate as bioink for three-dimensional (3D) cell printing based cartilage tissue engineering. 2018;83:195–201.
Kim YB, Lee H, Kim GH. Strategy to achieve highly porous/biocompatible macroscale cell blocks, using a collagen/genipin-bioink and an optimal 3D printing process. ACS Appl Mater Interfaces. 2016;8(47):32230–40.
Kosaraju SL, Puvanenthiran A, Lillford P. Naturally crosslinked gelatin gels with modified material properties. Food Res Int. 2010;43(10):2385–9.
Zheng H. Interaction mechanism in sol-gel transition of alginate solutions by addition of divalent cations. Carbohydr Res. 1997;302(1–2):97–101.
Draget KI, Skjåk-Bræk G, Smidsrød O. Alginate based new materials. Int J Biol Macromol. 1997;21(1–2):47–55.
Jia J, Richards DJ, Pollard S, Tan Y, Rodriguez J, Visconti RP, Trusk TC, et al. Engineering alginate as bioink for bioprinting. Acta Biomater. 2014;10(10):4323–31.
Gao Q, He Y, Jianzhong F, Liu A, Ma L. Coaxial nozzle-assisted 3D bioprinting with built-in microchannels for nutrients delivery. Biomaterials. 2015;61:203–15.
Schexnailder P, Schmidt G. Nanocomposite polymer hydrogels. Colloid Polym Sci. 2009;287(1):1–11.
Dvir T, Timko BP, Brigham MD, Naik SR, Karajanagi SS, Levy O, Jin H, Parker KK, Langer R, Kohane DS. Nanowired three-dimensional cardiac patches. Nat Nanotechnol. 2011;6(11):720–5.
Skardal A, Zhang J, McCoard L, Oottamasathien S, Prestwich GD. Dynamically crosslinked gold nanoparticle–hyaluronan hydrogels. Adv Mater. 2010;22(42):4736–40.
Xing R, Liu K, Jiao T, Zhang N, Ma K, Zhang R, Zou Q, Ma G, Yan X. An injectable self-assembling collagen–gold hybrid hydrogel for combinatorial antitumor photothermal/photodynamic therapy. Adv Mater. 2016;28(19):3669–76.
Zhu K, Shin SR, van Kempen T, Li Y-C, Ponraj V, Nasajpour A, Mandla S, et al. Gold nanocomposite bioink for printing 3D cardiac constructs. Adv Funct Mater. 2017;27(12):1605352.
Tognato R, Armiento AR, Bonfrate V, Levato R, Malda J, Alini M, Eglin D, Giancane G, Serra T. A stimuli-responsive nanocomposite for 3D anisotropic cell-guidance and magnetic soft robotics. Adv Funct Mater. 2019;29(9):1804647.
Tognato R, Armiento AR, Bonfrate V, Levato R, Malda J, Alini M, Eglin D, Giancane G, Serra T. A stimuli-responsive nanocomposite for 3D anisotropic cell-guidance and magnetic soft robotics. Adv Funct Mater. 2019;29(9):1804647.
Chen Q, Zhu L, Chen H, Yan H, Huang L, Yang J, Zheng J. A novel design strategy for fully physically linked double network hydrogels with tough, fatigue resistant, and self-healing properties. Adv Funct Mater. 2015;25(10):1598–607.
Liu S, Li L. Ultrastretchable and self-healing double-network hydrogel for 3D printing and strain sensor. ACS Appl Mater Interfaces. 2017;9(31):26429–37.
Yang F, Tadepalli V, Wiley BJ. 3D printing of a double network hydrogel with a compression strength and elastic modulus greater than those of cartilage. ACS Biomater Sci Eng. 2017;3(5):863–9.
Wu D, Yue Y, Tan J, Huang L, Binghong Luo LL, Zhou C. 3D bioprinting of gellan gum and poly (ethylene glycol) diacrylate based hydrogels to produce human-scale constructs with high-fidelity. Mater Des. 2018;160:486–95.
Naghieh S, et al. Printability of 3D printed hydrogel scaffolds: influence of hydrogel composition and printing parameters. Appl Sci. 2019;10(1):292.
He Y, et al. Research on the printability of hydrogels in 3D bioprinting. Sci Rep. 2016;6(1):1–13.
Wu D, Yue Y, Tan J, Huang L, Binghong Luo LL, Zhou C. 3D bioprinting of gellan gum and poly (ethylene glycol) diacrylate based hydrogels to produce human-scale constructs with high-fidelity. Mater Des. 2018;160:486–95.
Peak CW, Stein J, Gold KA, Gaharwar AK. Nanoengineered colloidal inks for 3D bioprinting. Langmuir. 2018;34(3):917–25.
Murphy SV, Atala A. 3D bioprinting of tissues and organs. Nat Biotechnol. 2014;32(8):773–85.
Blaeser A, Campos DFD, Puster U, Richtering W, Stevens MM, Fischer H. Controlling shear stress in 3D bioprinting is a key factor to balance printing resolution and stem cell integrity. Adv Healthc Mat. 2016;5(3):326–33.
Ouyang L, Rui Yao Y, Zhao, and Wei Sun. Effect of bioink properties on printability and cell viability for 3D bioplotting of embryonic stem cells. Biofabrication. 2016;8(3):035020.
Law N, Doney B, Glover H, Qin Y, Aman ZM, Sercombe TB, Liew LJ, Dilley RJ, Doyle BJ. Characterisation of hyaluronic acid methylcellulose hydrogels for 3D bioprinting. J Mech Behav Biomed Mater. 2018;77:389–99.
Müller M, Becher J, Schnabelrauch M, Zenobi-Wong M. Printing thermoresponsive reverse molds for the creation of patterned two-component hydrogels for 3D cell culture. JoVE (Journal of Visualized Experiments). 2013;77:e50632.
Sankaran S, Kalim Deshmukh M, Ahamed B, Khadheer Pasha SK. Electrospun polymeric nanofibers:fundamental aspects of electrospinning processes, optimization of electrospinning parameters, properties, and applications. In: Polymer nanocomposites in biomedical engineering. Cham: Springer; 2019. p. 375–409.
Ahmad J, Deshmukh K, Habib M, Hägg MB. Influence of TiO2 nanoparticles on the morphological, thermal and solution properties of PVA/TiO2 nanocomposite membranes. Arab J Sci Eng. 2014;39(10):6805–14.
Pasha K, SK KD, Ahamed MB, Chidambaram K, Mohanapriya MK, Arunai Nambi Raj N. Investigation of microstructure, morphology, mechanical, and dielectric properties of PVA/PbO nanocomposites. Adv Polym Technol. 2017;36(3):352–61.
Sadasivuni KK, Rattan S, Deshmukh K, Muzaffar A, Ahamed MB, Pasha SKK, Mazumdar P, Waseem S, Grohens Y, Kumar B. Hybrid nano-filler for value added rubber compounds for recycling. In: Rubber recycling; 2018. p. 310–29.
Thangamani J, Gounder KD, Sadasivuni KK, Chidambaram K, Ahamed MB, Ponnamma D, AlMaadeed MA-A, Pasha SKK. Recent advances in electrochemical biosensor and gas sensors based on graphene and carbon nanotubes (CNT)-a review. Adv Mater Lett. 2017;8(3):196–205.
Hong S, Sycks D, Chan HF, Lin S, Lopez GP, Guilak F, Leong KW, Zhao X. 3D printing of highly stretchable and tough hydrogels into complex, cellularized structures. Adv Mater. 2015;27(27):4035–40.
Sultan S, Mathew AP. 3D printed scaffolds with gradient porosity based on a cellulose nanocrystal hydrogel. Nanoscale. 2018;10(9):4421–31.
Liu S, Bastola AK, Li L. A 3D printable and mechanically robust hydrogel based on alginate and graphene oxide. ACS Appl Mater Interfaces. 2017;9(47):41473–81.
Wilson SA, Cross LM, Peak CW, Gaharwar AK. Shear-thinning and thermo-reversible nanoengineered inks for 3D bioprinting. ACS Appl Mater Interfaces. 2017;9(50):43449–58.
Roopavath UK, Soni R, Mahanta U, Deshpande AS, Rath SN. 3D printable SiO 2 nanoparticle ink for patient specific bone regeneration. RSC Adv. 2019;9(41):23832–42.
Nadgorny M, Ameli A. Functional polymers and nanocomposites for 3D printing of smart structures and devices. ACS Appl Mater Interfaces. 2018;10(21):17489–507.
Bair SS. High pressure rheology for quantitative elastohydrodynamics: Elsevier; 2019.
Van Vliet T, Van Dijk HJM, Zoon P, Walstra P. Relation between syneresis and rheological properties of particle gels. Colloid Polym Sci. 1991;269(6):620–7.
Jatav S, Joshi YM. Rheological signatures of gelation and effect of shear melting on aging colloidal suspension. J Rheol. 2014;58(5):1535–54.
Paxton N, Smolan W, Böck T, Melchels F, Groll J, Jungst T. Proposal to assess printability of bioinks for extrusion-based bioprinting and evaluation of rheological properties governing bioprintability. Biofabrication. 2017;9(4):044107.
Acknowledgements
Part of the research reported in this paper was supported by National Institute of Dental & Craniofacial Research of the National Institutes of Health under award number R15DE027533, R56DE029191, and 3R15DE027533-01A1W1.
The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Tajik, S., Garcia, C.N., Gillooley, S. et al. 3D Printing of Hybrid-Hydrogel Materials for Tissue Engineering: a Critical Review. Regen. Eng. Transl. Med. 9, 29–41 (2023). https://doi.org/10.1007/s40883-022-00267-w
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40883-022-00267-w