Abstract
Background
Studies have found an increased risk of pyoderma gangrenosum associated with rituximab. The structural properties and pharmacological action of rituximab may affect the risk of pyoderma gangrenosum. Additionally, pyoderma gangrenosum is associated with autoimmune disorders for which rituximab is indicated.
Objective
We aimed to determine whether rituximab is disproportionally associated with pyoderma gangrenosum using a systems biology-informed approach.
Methods
Adverse event reports were extracted from the US Food and Drug Administration Adverse Event Reporting System (FAERS, 2013–20). The Bayesian Confidence Propagation Neural Network Information Component was used to test for disproportionality. Comparators used to determine potential causal pathways included all other medicines, all medicines with a similar structure (monoclonal antibodies), all medicines with the same pharmacological target (CD20 antagonists) and all medicines used for the same indication(s) as rituximab.
Results
Thirty-two pyoderma gangrenosum cases were identified, 62.5% were female, with a median age of 48 years. There was an increased association of pyoderma gangrenosum with rituximab compared with all other medicines (exponentiated Information Component 6.75, 95% confidence interval (CI) 4.66–9.23). No association was observed when the comparator was either monoclonal antibodies or CD20 antagonists. Conditions for which an association of pyoderma gangrenosum with rituximab was observed were multiple sclerosis (6.68, 95% CI 1.63–15.15), rheumatoid arthritis (2.67, 95% CI 1.14–4.80) and non-Hodgkin’s lymphoma (2.94, 95% CI 1.80–3.73).
Conclusions
Pyoderma gangrenosum was reported more frequently with rituximab compared with all other medicines. The varying results when restricting medicines for the same condition suggest the potential for confounding by indication. Post-market surveillance of biologic medicines in FAERS should consider a multi-faceted approach, particularly when the outcome of interest is associated with the underlying immune condition being treated by the medicine of interest.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
It is difficult to understand the plausibility of an adverse drug reaction if the medicine is confounded by indication. |
Biologic medicines have been associated with immune-mediated adverse drug reactions when used for autoimmune disorders. |
A systems biology-informed approach to estimate associations using spontaneous reports of adverse drug reactions may be useful in understanding the causal pathway for a potential increase in risk, adjusting for confounding and provide evidence of causal coherence. |
1 Introduction
Regulatory authorities rely on spontaneous reporting systems to monitor the post-market safety of medicines. Spontaneous reports are submitted by medicine sponsors, health practitioners and the public to regulatory agencies around the world [1]. Analyses of these data can be effective in alerting regulatory agencies to potential medicine-related harm for further investigation. However, there are limitations with this system because of under-reporting of adverse events. Further, it is often challenging to attribute causality and accurately inform regulatory processes owing to a lack of clinical information and baseline rates of disease [2]. It may be difficult to determine whether an adverse drug reaction (ADR) identified for a medicine is plausible if both the medicine and the indication are associated with or confounded by the indication for which the medicine is used. This is particularly the case for safety signals detected with biologic medicines and immune-mediated side effects.
Biologic medicines are increasingly used in the management of high-burden chronic autoimmune diseases and cancers, [3, 4]; however, knowledge regarding the safety of biologic medicines is limited, as pre-marketing studies often have small sample sizes and short follow-up periods [3, 5]. Additionally, their unique structural and pharmacological actions may affect the risk of ADRs.
Rituximab, first introduced in the late 1990s for the treatment of B-cell non-Hodgkin’s lymphoma [3, 4, 6] and subsequently for rheumatoid arthritis and B-cell chronic lymphocytic leukaemia [3], acts by targeting CD20, a specific B-cell antigen, which results in cellular destruction [7]. Common ADRs associated with rituximab include immune-mediated infusion reactions and infections [6, 7] while rare adverse reactions include Merkel cell carcinoma, Stevens–Johnson syndrome and toxic epidermal necrolysis [7,8,9]. In a recent study using spontaneous reports collected by the US Food and Drug Administration, a three-fold increase in the association of pyoderma gangrenosum (PG) was observed with the use of rituximab when compared with all other medicines [10]. Pyoderma gangrenosum is a rare inflammatory skin disease first described in 1916 with an estimated incidence of 1–5.8 per 100,000 per year [11, 12]. Pyoderma gangrenosum behaves in an unpredictable manner with eight variants of PG currently described in the literature [11]. These variants differ by site and type of ulceration, degree of progression of disease and response to therapy [11]. The pathology is thought to include both innate and adaptive immune responses together with a genetic component [12] and PG is more common among people with systemic autoimmune disorders such as inflammatory bowel disease (30%), rheumatoid arthritis (25%) and haematological malignancies (25%) [11, 13].
There is no gold standard treatment for PG and treatment regimes are currently based on expert opinion, case studies and small cohort studies [12]; however, wound care and analgesia are the cornerstone for the management of PG [14]. Several biologic medicines have also been shown to be effective in treating PG including infliximab and rituximab [10, 12, 13].
Given the place of rituximab in therapy, and the potential for an increased risk of PG in conditions for which rituximab is used, we aimed to investigate the suspected signal of PG associated with rituximab using the US Food and Drug Administration Adverse Event Reporting System (FAERS) database. To do this, we used a systems biology informed approach in which we aimed to determine whether rituximab is associated with an increased risk of PG when compared to all other medicines with the same structure as rituximab (monoclonal antibodies [mAbs]), the same pharmacological target (CD20 antagonists) and when restricted to medicines used for the same indication as rituximab (e.g., non-Hodgkin’s lymphoma). A systems biology approach uses a network of factors to determine the influence of interacting human and medicinal traits on the risk of an ADR [15]. In this study, we have leveraged the systems biology concepts that the chemical structure or pharmacological target of a medicine can influence the risk of an ADR. We have combined these concepts with an additional sub-population analysis to adjust for confounding by indication. This approach may be useful in understanding the causal pathway for a potential increase in the risk of an ADR from complex immunomodulating molecules used to treat chronic autoimmune disorders such as biologic medicines [16,17,18,19,20].
2 Objective
The objective of this study was to determine whether rituximab is disproportionally associated with PG using a systems biology approach.
3 Methods
3.1 Data Source and Preparation
Adverse drug reaction case reports were sourced from FAERS online quarterly extracts from 1 January, 2013 (shift from legacy Adverse Event Reporting System to FAERs files) to 30 September, 2020 (latest reporting period at time of study) [21]. FAERS is the US spontaneous reporting system for ADRs. To date, it contains over 24 million ADR reports from industry, clinicians and consumers [22]. Relevant demographic, exposure and outcome variables were extracted, where available (Table 1).
3.2 Identification of Outcome (PG) and Indications
In FAERS, the ADR terms and indication for each medicine are provided as Preferred Term level labels of the Medical Dictionary for Regulatory Activities (MedDRA) [23, 24]. Pyoderma gangrenosum was identified by a report of “Pyoderma Gangrenosum” (MedDRA Code = 10037635).
Comparator ADRs included all other ADRs excluding skin conditions [System Organ Class categorisation of skin and subcutaneous tissue disorders [23]]. This approach was employed to ensure competing or similar adverse events were removed from the baseline ADR counts to minimise misclassification. Adverse drug reactions were removed from the analysis if PG was the indication for any medicines taken by the patient prior to their report, as exposure should precede outcome.
3.3 Identification of Exposure (Rituximab and Comparator Medicines)
Unlike ADRs and indications, medicine names in FAERS are not standardised. Medicine names can be entered in many forms including generic names, brand names and medicine synonyms. Misspellings including superfluous text are common. To optimise capture (and to minimise misclassification) of all medicine entries, fuzzy string matching of medicine names was performed using a sequence of steps. First, the Observational Health Data Sciences and Informatics common data model vocabulary files were used to find drug synonyms [25]. Second, FAERS data were queried to find potential valid medicine representations. Potential matches were extracted from the database if they met any of the following criteria (a) within a soundex distance of two (b) the first three letters were contained anywhere in the potential match, or (c) the last three letters are contained anywhere in the potential match. This list of potential matches including false positives were then assessed using a classification boundary based on regular expressions and full Damerau–Levenshtein distance [26]. From this list of medicine matches, a manual review of the match status was undertaken to finalise the set of records for extraction from FAERS for analysis. Fuzzy matching was undertaken for ‘rituximab’, all ‘mAbs’ and all ‘CD20 antagonists’ (see Appendix A in the Electronic Supplementary Material [ESM] for a flow chart of fuzzy matching methodology).
Data were limited to medicines that were listed as “primary suspect” to the ADR. Records were also limited to the last case version of the report (case id) as is recommended by the Food and Drug Administration [27]. Patient demographics and indications for rituximab were linked via the primary id corresponding to the last case version for each case id. Each list of comparator medicines was validated, prior to analysis, by clinical pharmacists (Appendix B of the ESM).
3.4 Disproportionality Analysis
We employed the Bayesian Confidence Propagation Neural Network Information Component statistic, estimated using Markov Chain Monte Carlo simulation, as it is appropriate for small sample sizes [28,29,30,31]. We present an exponentiated Information Component, denoted ratio scale Information Component (RSIC), to report disproportionality estimates on the ratio scale as seen in common disproportionality statistics such as the reporting odds ratio and the proportional reporting ratio [28]. In our study, we considered all medicine-outcome pairs where there were at least three reports and a potential signal was identified when the RSIC estimate was >2 and the corresponding 95% confidence interval (CI) lower bound was > 1 (significant at the α = 0.05) [32,33,34]. As well as estimating an overall association with ADRs, we used a systems biology informed approach to choosing comparator groups to determine if the association varied according to chemical properties (mAbs vs all other medicines), pharmacological action (CD20 inhibitors vs all other medications) or clinical indication (autoimmune disease and all other indications) (Table 2).
4 Results
There were 1105 reports of PG in the FAERS database, of which rituximab was the primary suspect in 32 cases and PG was not the indication for treatment (Table 2). Median age for rituximab PG cases and all other medicines was 48 and 51 years, respectively. For reports where sex was recorded, 100% of rituximab PG cases and 61.5% of all other medicines PG cases were female. The PG cases were observed in every year of the study period.
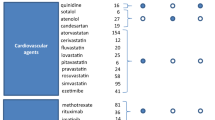
When compared with all other medicines, rituximab had a significantly disproportional number of PG reports with a RSIC estimate of 6.55, 95% CI 4.52–8.95. When compared to all other mAbs, the disproportionality estimate for rituximab was non-significant (RSIC 1.11, 95% CI 0.77–1.51). Compared with other CD20s the disproportionality estimate was 1.42 (95% CI 1.24–1.53), which does not meet the signal threshold. When analyses were limited to populations using medicines for rheumatoid arthritis, multiple sclerosis and non-Hodgkin’s lymphoma indications, there were significant measures of disproportionality estimated (Fig. 1 and Table 3); 3.57 (95% CI 1.78–5.95), 8.46 (95% CI 2.55–17.70), and 2.43 (95% CI 1.37–3.50), respectively.
Signal detection estimates (ratio scale information component [RSIC]) of rituximab vs other comparators for pyoderma gangrenosum. All all other medicines, BCPNN Bayesian Confidence Propagation Neural Network, CI confidence interval, mAbs monoclonal antibodies, MCMC Markov Chain Monte Carlo, MS multiple sclerosis, NHL non-Hodgkin’s lymphoma, RA rheumatoid arthritis
5 Discussion
This study used a systems biology-informed approach to assist with understanding of safety signals generated in spontaneous reports data. As found previously, there was a disproportional number of reports of PG associated with rituximab when compared with all other medicines, however, when restricted to medicines of similar structural or pharmacological properties, no association with PG was observed. When analyses were limited to the most common indications for the use of rituximab, rheumatoid arthritis, multiple sclerosis and non-Hodgkin’s lymphoma, an elevated risk profile was observed compared with the use of all other medicines for these indications. These results suggest that the apparent association between PG and rituximab may be due to the chemical properties or pharmacological actions of rituximab. When stratifying by the indication of the medicines, a signal was observed between PG and rituximab for multiple sclerosis; however, the association with rituximab and PG was lower in RA and non-Hodgkin’s lymphoma, suggesting that the underlying disease may modify the risk of PG. The wide CI for the multiple sclerosis analysis is due to a small sample size and should be interpreted with caution.
These results are useful for informing if there is an association between rituximab and PG and whether the potential signal requires further investigation using more robust pharmacoepidemiologic methods [17]. Small case studies and series have shown that in those who develop PG whilst receiving rituximab, cessation of rituximab has reversed the PG, whilst in contrast the initiation of rituximab has been demonstrated as a successful treatment for PG [10]. This clinical contradiction challenges the biological plausibility of an association.
A 2021 pharmacovigilance study used a similar approach with respect to adjusting for the baseline risk of the outcome by stratifying by the medication indication [19]. This study estimated the risk of acute pancreatitis with sodium glucose co-transporter 2 inhibitors in Vigibase, by restricting analyses to only medicines used for diabetes mellitus, as diabetes is a potential risk factor for pancreatitis. That study found that the majority of risk estimates were non-significant after restricting the analysis to diabetes only. The authors concluded that other mechanisms may be in play such as diabetic ketoacidosis-induced acute pancreatitis rather than the medicine.
The strengths of the current study include the use of fuzzy matching to maximize case capture and minimise the misclassification of medicines. We also used a disproportionality method, Bayesian Confidence Propagation Neural Network, which is appropriate for small sample sizes as it adjusts for small cell counts [28]. While our estimate of risk when compared with all medicines was higher than that reported by the earlier study of Aggarwal [10], both studies found a positive association with rituximab and PG, despite different methodologies; however, the attenuation of disproportionality when we employed our approach suggests that confounding by indication may account for some of the association observed.
Our study has the same limitations of similar studies using voluntary reporting systems including under-reporting and a lack of clinical details [19]. In this study, demographic details for age, sex, duration of treatment, comorbidities, re-challenge and de-challenge were missing for many cases and this may influence the outcomes of our study. In addition, the preferred terms for outcome used in this study may not have captured all cases.
In total, there were 155 reports missing the indication for treatment, which may have included PG. Of these, 97% were in the non-rituximab PG case cohort. If non-rituximab PG cases had a PG indication, then they would have been excluded from our analysis, as per inclusion criteria, and this would have resulted in a weaker signal.
A relatively large proportion of cases were reported from Australia. This may be because of international differences in clinical practices (e.g., diagnostics) or it may be owing to the fact that drug sponsors in Australia are mandated to report any ADR to the Therapeutic Goods Administration, potentially resulting in a higher reporting rate compared with other countries.
This study used spontaneous reporting data that may be influenced by the level of awareness of reporting ADRs amongst health professionals and in this case the level of skill in correctly diagnosing PG. Therefore, this study may have underestimated the overall numbers of PG occurring in the community.
6 Conclusions
This study identified an association between reports of PG associated with the use of rituximab; however, we have identified that there are plausible pathways that may explain this apparent association including the chemical structure or pharmacological action of the medicine. As rituximab is an effective treatment in life-threatening and chronic conditions of high morbidity and PG is a treatable condition of rare occurrence, these results do not change the risk/benefit profile of rituximab. Post-market surveillance of biologic medicines using spontaneous reports data should consider leveraging concepts from the systems biology approach to ADR detection to determine if more sophisticated studies are required to strengthen the signal plausibility, particularly when the outcome of interest is associated with the underlying immune condition being treated by the medicine of interest.
References
Alomar M, Tawfiq AM, Hassan N, Palaian S. Post marketing surveillance of suspected adverse drug reactions through spontaneous reporting: current status, challenges and the future. Ther Adv Drug Saf. 2020;11:2042098620938595.
Giezen TJ, Mantel-Teeuwisse AK, Leufkens HG. Pharmacovigilance of biopharmaceuticals: challenges remain. Drug Saf. 2009;32(10):811–7.
Castelli MS, McGonigle P, Hornby PJ. The pharmacology and therapeutic applications of monoclonal antibodies. Pharmacol Res Perspect. 2019;7(6): e00535.
Dotan E, Aggarwal C, Smith MR. Impact of rituximab (Rituxan) on the treatment of B-cell non-Hodgkin’s lymphoma. Pharm Ther. 2010;39(3):148–57.
Ingrasciotta Y, Cutroneo PM, Marcianò I, Giezen T, Atzeni F, Trifirò G. Safety of biologics, including biosimilars: perspectives on current status and future direction. Drug Saf. 2018;41(11):1013–22.
Randall KL. Rituximab in autoimmune diseases. Aust Prescr. 2016;39(4):131–4.
Selewski DT, Shah GV, Mody RJ, Rajdev PA, Mukherji SK. Rituximab (Rituxan). Am J Neuroradiol. 2010;31(7):1178–80.
Rafiee Zadeh A, Ghadimi K, Ataei A, Askari M, Sheikhinia N, Tavoosi N, et al. Mechanism and adverse effects of multiple sclerosis drugs: a review article. Part 2. Int J Physiol Pathophysiol Pharmacol. 2019;11(4):105–14.
Therapeutic Goods Administration. Database of adverse event notifications. Medicine Summary (Rituximab). Institution: Department of Health 2020; Canberra: Australian Government. 2020.
Aggarwal P. Pyoderma gangrenosum adverse event with rituximab use: a postmarketing pharmacovigilance analysis. Dermatol Ther. 2020;33(2): e13221.
Ruocco E, Sangiuliano S, Gravina AJ, Miranda A, Nicoletti G. Pyoderma gangrenosum: an updated review. J Eur Acad Dermatol Venereol. 2009;23(9):1008–17.
Fletcher J, Alhusayen R, Alavi A. Recent advances in managing and understanding pyoderma gangrenosum. F1000 Res. 2019;8:F1000 Faculty Rev-2092.
Brookly T, Dunnill G, Probert C. Diagnosis and treatment of pyoderma gangrenosum. BMJ. 2006;333(3655):181–4.
Isoherranen K, O’Brien JJ, Barker J, Dissemond J, Hafner J, Jemec GBE, et al. Atypical wounds: best clinical practices and challenges. An EWMA document. J Wound Care. 2019;28(6):S1-92.
Boland MR, Jacunski A, Lorberbaum T, Romano JD, Moskovitch R, Tatonetti NP. Systems biology approaches for identifying adverse drug reactions and elucidating their underlying biological mechanisms. Wiley Interdiscip Rev Syst Biol Med. 2016;8(2):104–22.
Cutroneo PM, Isgro V, Russo A, Ientile V, Sottosanti L, Pimpinella G, et al. Safety profile of biological medicines as compared with non-biologicals: an analysis of the Italian spontaneous reporting system database. Drug Saf. 2014;37(11):961–70.
Cox LA. Modernizing the Bradford Hill criteria for assessing causal relationships in observational data. Crit Rev Toxicol. 2018;48(8):682–712.
Duran-Frigola M, Aloy P. Analysis of chemical and biological features yields mechanistic insights into drug side effects. Chem Biol. 2013;20(4):594–603.
Frent I, Busca C, Leucuta D, Farcas A, Mogosan C. An investigation on the association between sodium glucose co-transporter 2 inhibitors use and acute pancreatitis: a VigiBase study. Pharmacoepidemiol Drug Saf. 2021;30(10):1428–40. https://doi.org/10.1002/pds.5313.
Lorberbaum T, Nasir M, Keiser MJ, Vilar S, Hripcsak G, Tatonetti NP. Systems pharmacology augments drug safety surveillance. Clin Pharmacol Ther. 2015;97(2):151–8.
US Food and Drug Administration. FDA Adverse Event Reporting System (FAERS) quarterly data extract files.
US Food and Drug Administration (FDA). FDA adverse event reporting system (FAERS) public dashboard. Silver Spring: Department of Health and Human Services; 2022.
Medical Dictionary for Regulatory Activities (MeDRA) 2020. https://www.meddra.org/browsers. Accessed 8 Jul 2022.
Ontology NCfB. Medical Dictionary for Regulatory Activities terminology (MedDRA). BioPortal: National Centres for Biomedical Computing; 2021. https://bioportal.bioontology.org/ontologies/MEDDRA?p=summary. Accessed 8 Jul 2022.
OHDSI. The book of OHDSI. Chapter 4: the common data model. https://ohdsi.github.io/TheBookOfOhdsi/CommonDataModel. Accessed 8 Jul 2022.
van der Loo M. The stringdist package for approximate string matching. R J. 2014;6:111–22.
Ibrahim H, Saad A, Abdo A, Sharaf EA. Mining association patterns of drug-interactions using post marketing FDA’s spontaneous reporting data. J Biomed Inform. 2016;60:294–308.
Gould AL. Practical pharmacovigilance analysis strategies. Pharmacoepidemiol Drug Saf. 2003;12(7):559–74.
Bate A, Lindquist M, Edwards IR, Olsson S, Orre R, Lansner A, et al. A Bayesian neural network method for adverse drug reaction signal generation. Eur J Clin Pharmacol. 1998;54(4):315–21.
Bate A, Lindquist M, Edwards IR, Orre R. A data mining approach for signal detection and analysis. Drug Saf. 2002;25(6):393–7.
Norén GN, Bate A, Orre R, Edwards IR. Extending the methods used to screen the WHO drug safety database towards analysis of complex associations and improved accuracy for rare events. Stat Med. 2006;25(21):3740–57.
Candore G, Juhlin K, Manlik K, Thakrar B, Quarcoo N, Seabroke S, et al. Comparison of statistical signal detection methods within and across spontaneous reporting databases. Drug Saf. 2015;38(6):577–87.
Evans SJW, Waller PC, Davis S. Use of proportional reporting ratios (PRRs) for signal generation from spontaneous adverse drug reaction reports. Pharmacoepidemiol Drug Saf. 2001;10(6):483–6.
Ji HH, Tang XW, Dong Z, Song L, Jia YT. Adverse event profiles of anti-CTLA-4 and anti-PD-1 monoclonal antibodies alone or in combination: analysis of spontaneous reports submitted to FAERS. Clin Drug Investig. 2019;39(3):319–30.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
This research was funded by the National Health and Medical Research Council (NHMRC) Project Grant GNT1157506 and GNT1196900. EE Roughead is funded under NHRMC GNT1110139.
Conflicts of interest/Competing interests
Jodie Belinda Hillen, Ty Stanford, Michael Ward, EE Roughead, Lisa Kalisch Ellett and Nicole Pratt have no conflicts of interest that are directly relevant to the content of this study.
Ethics approval
This research was approved by the University of South Australia Human Research Ethics Committee (Application ID: 201902).
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Availability of data and material
Data are available from the FAERS Public Dashboard.
Code availability
The code is available at https://github.com/tystan/ritux_pg.
Authors’ contributions
JBH and NP developed the study protocol, analysed the data and drafted the manuscript. TS extracted the FAERS data, conducted the risk analyses and drafted the manuscript. MW contributed to the study protocol and interpreting the data. EER and LKE contributed to the study protocol and drafting of the manuscript. All authors read and approved the final manuscript.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Hillen, J.B., Stanford, T., Ward, M. et al. Rituximab and Pyoderma Gangrenosum: An Investigation of Disproportionality Using a Systems Biology-Informed Approach in the FAERS Database. Drugs - Real World Outcomes 9, 639–647 (2022). https://doi.org/10.1007/s40801-022-00322-6
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40801-022-00322-6