Abstract
Background
Acromegaly is a rare, debilitating condition for which data on the associated treatment patterns and economic burden are limited.
Objective
Our objective was to examine patient characteristics, treatment patterns, and healthcare resource utilization (HRU)/costs for individuals with acromegaly treated with surgical and/or medical therapy in the USA.
Methods
Using a large US claims database, adults with new episodes of acromegaly between 1 July 2007 and 31 December 2010 were identified (the first observed diagnosis being the index date). Patients had 6-month pre-index and 12-month post-index continuous enrollment and surgical and/or medical treatment during the 12-month post-index period. Descriptive analysis was performed to observe demographic/clinical characteristics, treatment patterns, HRU, and monthly healthcare costs between two mutually exclusive surgically and medically treated cohorts.
Results
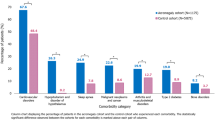
This study included 228 acromegalic individuals treated with surgical therapy and 169 treated with medical therapy. During the 12-month follow-up, compared with the medical cohort, the surgical cohort were more likely to have hypertension (50.4 vs. 32.0 %), sleep apnea (31.6 vs. 15.8 %), cardiac dysrhythmia (16.7 vs. 7.0 %), hospitalizations (98.3 vs. 13.6 %), and emergency room visits (29.8 vs. 20.7 %), and had more outpatient visits (10.2 vs. 5.2) and physician office visits (21.2 vs. 15.0) (all differences, p < 0.05). The surgical cohort had lower monthly healthcare costs during the 6-month pre-index period ($US1963.5 vs. 2818.4) but higher costs in the 12-month post-index period ($US5202.6 vs. 3076.5) than the medical cohort.
Conclusions
Our findings suggest the treatment pathway observed in this patient population has a non-negligible association with the clinical and economic burden.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
To address known data gaps, this study analyzed patients in a large US administrative claims database who had received surgical therapy and/or medical therapy for newly recognized episodes of acromegaly, in order to assess the prevalence of comorbid conditions, treatment patterns, health resource utilization, and costs. |
Compared with patients given medical therapy, those treated with surgical therapy had lower monthly healthcare costs during the 6-month pre-index period, and a higher prevalence of hypertension, sleep apnea, cardiac rhythm problems, and abnormal glucose, and higher costs in the 12-month post-index period. |
Future research is needed to assess the incremental economic burden associated with acromegaly and the cost-effectiveness of treatment options that cure the disease or decelerate its progression. |
1 Introduction
Acromegaly is a debilitating disorder characterized by overgrowth of tissues throughout the body. It is caused by chronic growth hormone (GH) excess, typically due to a benign pituitary adenoma [1] that develops gradually [2]. The condition is rare, with a prevalence of 58–130 cases per million [3, 4]. Even so, the clinical and quality-of-life burden posed by acromegaly is considerable. This is partly because patients often present with chronic comorbid conditions such as diabetes, hypertension, or valvular heart disease [5] or may require lifelong treatment. Also, evidence suggests that over half of patients with acromegaly are not treated effectively with respect to achieving disease control and minimizing adverse events such as nausea, vomiting, and headache [5, 6]. Furthermore, overall standardized mortality rates for those with disease are approximately twice those in the general population [7].
Such factors emphasize the importance of early diagnosis and optimal treatment, which can mitigate the increased mortality risk [8]. In this context, recent treatment guidelines recommend that first-line treatment for acromegaly in most cases is tumor excision surgery where the pituitary adenoma is resectable and the patient is a suitable surgical candidate [5]. Crucially, such treatment is potentially curative, and has an initial remission rate of over 85 % for microadenomas and 40–50 % for macroadenomas when performed by experienced surgeons [9, 10]. However, repeat operations may be needed for patients with residual intrasellar disease following initial surgery [9, 10].
By comparison, the guidelines recommend medical therapy as a first-line intervention only when surgery is not recommended, for example, where it is contraindicated or the tumor is unresectable. Medical therapy is also advocated as second-line treatment where disease persists following surgery, cavernous sinus invasion is extensive, there is no chiasmal compression, or the tumor recurs [5]. Also, many patients initially treated with medical therapy will eventually need surgery. While medical therapy aims primarily to control symptoms, it is commonly accompanied by tumor shrinkage within 3 months of starting the treatment [9, 10]. Drug therapy for acromegaly may also have beneficial effects on comorbidities. Treatment guidelines recommend radiotherapy as a possible treatment when there is a residual tumor mass following surgery and if medical therapy is unavailable or not tolerated [9, 10]. Radiotherapy is generally used as a third-line therapy, and, when used alone or with surgery or medical therapy, is likely to effect disease control [5, 6]. However, it is a more risky option, which may lead to hypopituitarism, visual defects, secondary tumors, and cerebrovascular events [5, 6]. Ultimately, surgical and medical therapies are the two mainstay treatments for acromegaly, with a multimodal approach often being needed.
While such treatment pathways for acromegaly are well-established, there is much less clarity about real-world treatment patterns for the disease and the related economic burden. One of the few recently published studies on this topic assessed data from 2003 to 2009 and found that total healthcare costs associated with treating acromegalic patients in the US were $US24,284 per patient-year, with 70 % from medical costs and 30 % from pharmacy costs [11]. One recent study examined real-world clinical characteristics and treatment patterns of individuals with acromegaly in the US [5], and another study explored treatment patterns, complications, and healthcare resource utilization (HRU) associated with acromegaly [12]. Notably, both of these studies focused on prevalent cases.
Against this background, the objective of the current study was to assess patients presenting with a new (and possibly) first episode of acromegaly and treated initially with either surgical excision or medical therapy, specifically to compare clinical characteristics, treatment patterns, HRU, and costs between these treatment groups. Accordingly, we applied a study design that specifically aimed to capture evidence on such patients and to allow evaluation of the initial treatment and add-on/switch therapies.
2 Methods
2.1 Data Source
Data for this retrospective study were obtained from the Truven MarketScan® Commercial Claims Databases (Truven Health Analytics™, Ann Arbor, MI, USA). These databases contain data (1995–present) for over 150 million patients residing in all US census regions, representing the healthcare experience of employees and dependents [13]. The MarketScan Research databases provide information on patient demographics and health plan enrollment, and capture person-specific HRU and costs across hospital inpatient and outpatient services, physician office visits, home health, hospice, and prescription medications. The commercial databases include large employers, health plans, government organizations, and public organizations, and cover approximately 100 payers and more than 500 million claims records. The databases link paid claims and encounter data to detailed patient information across healthcare settings and types of providers over time. Patient and provider information contained in these databases are de-identified, thus maintaining full compliance with the privacy regulations of the Health Insurance Portability and Accountability Act of 1996. Data records examined for this study spanned the time period from 1 January 2007 through 31 December 2011.
2.2 Patient Selection Criteria
Individuals aged 18 years or older, with two or more medical claims at least 30 days apart between 1 July 2007 and 31 December 2010 (the date range), with a diagnosis of acromegaly (primary or secondary International Classification of Diseases, Ninth Revision, Clinical Modification [ICD-9-CM] diagnosis code of 253.0) were selected. The data records covered 1 January 2007 through 31 December 2011 (the data records range), so the 1 July 2007 through 31 December 2010 date range was chosen to ensure that all included individuals would have at least a 6-month pre-selection period and a 12-month post-selection period for (1) an assessment of continuous health plan enrollment and (2) an assessment of baseline comorbid conditions, HRU, and costs. The first observed diagnosis was denoted as the index date. In order to identify those with a new episode of acromegaly, individuals with a medical claim with a diagnosis of acromegaly in the 6-month pre-index period were excluded. For example, if an individual with acromegaly had an index date of 15 July 2007 using claims in the date range, but also had a claim with a diagnosis of acromegaly on 14 March 2007 (in the data records range but out of the date range), this individual was excluded from the final sample size after applying this selection criterion. Individuals were required to have either surgical or medical therapy during the 12-month post-index period.
2.3 Study Populations and Identification of Treatment Cohorts
Patients were assigned into cohorts based only on whether they received surgery or medical therapy. Specifically, each individual with acromegaly was categorized into two mutually exclusive cohorts based on whether they received (1) tumor resection surgery (see Sect. 6 for procedure codes) with/without medical therapy (surgical therapy cohort) or (2) medical therapy without surgery (medical therapy cohort). Medical therapy included somatostatin analog treatment (i.e., lanreotide depot, octreotide, octreotide long-acting release [LAR], growth hormone receptor antagonists [i.e., pegvisomant], and dopamine agonists [bromocriptine and cabergoline]).
2.4 Study Measures
Study measures included demographic characteristics comprising age, sex, plan type, and US geographic region (northeast, midwest, south, and west) assessed as of the index date. The prevalence of acromegaly-related comorbidities in the baseline and post-index periods was derived using claims dated during 6 months prior to and 12 months after the index date, respectively. The comorbidities of interest included visual-field defects, hypopituitarism, osteoarthritis, arthropathy/arthralgia/synovitis, kyphosis and scoliosis, vertebral fracture, carpal tunnel syndrome, myopathy/myalgia, hypertension, cardiomyopathy, cardiac hypertrophy, heart failure, valvular heart disease, cardiac dysrhythmia/arrhythmia, nasal polyps, sleep apnea, diabetes, galactorrhea, menstrual abnormality, impaired libido/impotence, colon polyp, and hyperhidrosis.
Treatment patterns during the 12 months following the index date were also assessed. Measures of interest included tumor resection surgery, stereotactic radiotherapy, and medical therapy. Treatment sequence in terms of first-line and second-line treatments in the 12-month post-index period was assessed. First-line treatment patterns included tumor resection surgery and medical therapy. For individuals who received tumor resection surgery as the first-line treatment, subsequent treatment patterns were examined, including both medical therapy and no further treatment. For patients who received medical therapy as the first-line treatment, subsequent treatment patterns were examined, including no second-line therapy (i.e., patients who either continued to use the initial drug or completely discontinued its use throughout the 12-month post-index period), add-on, switching, and tumor resection surgery. Add-on was defined as adding another drug to the initial drug, and switching referred to discontinuing the initial drug and starting another drug.
HRU measures included inpatient hospitalization, emergency room (ER) visits, outpatient visits, physician office visits, and the use of specialty care (i.e., endocrinologist, neurosurgeon, or oncologist visits). These measures were assessed for both the 6-month pre-index and 12-month post-index periods. Monthly total healthcare costs were assessed during the 6-month pre-index and 12-month post-index periods. The cost categories included inpatient, outpatient, and pharmacy costs. All-cause and acromegaly-associated healthcare costs were estimated. Since the index date was set as the date of the initial diagnosis of the new episode of acromegaly, the acromegaly-associated healthcare costs could be captured only during the post-index period. Acromegaly-associated healthcare costs were defined as costs recorded on medical claims with at least one ICD-9-CM diagnosis code suggesting acromegaly (253.0), or costs reported on pharmacy claims with acromegaly-associated medical therapy including somatostatin analogs, growth hormone receptor antagonists, and dopamine agonists. As individuals entered and exited the study during different years, cost measures were standardized to $US, year 2011 values, using inflationary factors [14]. A total cost perspective, which included both healthcare payments plus any patient copayments/deductibles, was used for this analysis. To standardize cost comparisons, since the duration of pre-index and post-index periods differed, we reported healthcare costs on a monthly, rather than annual, basis.
2.5 Data Analyses
Descriptive analyses were conducted, and means and standard deviations (SDs) were reported for continuous variables in demographic characteristics and HRU. Percentages were reported for categorical variables in demographics, clinical characteristics, and HRU. Frequency distributions with percentages were reported for treatment sequences.
All-cause monthly total healthcare costs and cost by settings were compared between study cohorts. The non-parametric Wilcoxon test was used to detect differences for cost variables. Proportions of acromegaly-associated monthly healthcare costs, out of all-cause costs, were presented overall and separately for inpatient costs, outpatient costs, and pharmacy costs in the 12-month post-index period.
An additional subgroup analysis was conducted on a subset of individuals with at least 2 years of post-index data. All-cause monthly total healthcare costs and cost by settings for the 6-month pre-index period, and the first-year and second-year post-index periods were presented for this sub-sample. The percentages of acromegaly-associated monthly total healthcare costs and cost by settings were reported for the first-year and second-year post-index periods.
3 Results
3.1 Sample Selection
The study identified a total of 2492 commercially insured individuals with acromegaly and at least two claims for the disease between 1 July 2007 and 31 December 2010. After applying all the inclusion/exclusion criteria, the final study sample included 397 commercially insured individuals, of whom 228 (57.4 %) received surgical therapy with or without medical therapy and 169 (42.6 %) received medical therapy without surgery during the study (Fig. 1).
Sample selection of commercially insured acromegalic individuals who received surgical and/or medical therapy. * represents the medical therapy cohort included individuals with acromegaly who received medical therapy without surgery during the 12-month post-index period; † represents the surgical therapy cohort included individuals with acromegaly who received surgical therapy with/without medical therapies during the 12-month post-index period
3.2 Baseline Demographic Characteristics
Baseline patient demographic characteristics of acromegalic individuals by type of treatment are displayed in Table 1. The mean (SD) age among individuals in the medical therapy cohort (47.9 % female) and surgical therapy cohort (49.6 % female) was 47.2 (10.5) and 46.4 (10.2) years, respectively. Preferred provider organization (PPO) health plans insured over half of the individuals in the medical therapy cohort, with smaller proportions being insured by health maintenance organization (HMO) plans (18.9 %) and point of service (POS) plans (10.7 %). Over four-tenths of the patients resided in the south region. In the surgical therapy cohort, close to two-thirds of the individuals had a PPO plan type, followed by 17.1 % with an HMO plan and 8.8 % with a POS plan; over one-third resided in the south region. Baseline demographic characteristics were fairly well balanced between the two study cohorts.
3.3 Six-Month Pre-Index and 12-Month Post-Index Clinical Characteristics
Acromegalic individuals, whether in the surgical or the medical therapy cohort, had similar baseline clinical characteristics except for sleep apnea (14.2 vs. 7.1 %, respectively, p = 0.009) (Table 2). During the 12-month post-index period, compared with the medical therapy cohort, individuals in the surgical therapy cohort had a higher prevalence of hypertension (50.4 vs. 32.0 %), sleep apnea (31.6 vs. 15.8 %), cardiac dysrhythmia/arrhythmia (16.7 vs. 7.0 %), and abnormal glucose (11.0 vs. 5.3 %) (all differences, p < 0.05).
3.4 Treatment Patterns and Healthcare Resource Utilization
In the surgical therapy cohort, 31.6 % (72 of 228) of the individuals also received medical therapy during the 12-month post-index period (Table 3). Regarding the prescription medication used for treating acromegaly in the medical therapy cohort, 37.9 % of individuals were prescribed octreotide LAR, 37.3 % cabergoline, 16 % pegvisomant, 11.8 % bromocriptine, and 10.7 % lanreotide depot.
During the 6-month pre-index period, the overall pattern of HRU was similar between the two study cohorts, except that, compared with the medical therapy cohort, the surgical therapy cohort had more hospital outpatient visits (2.9 vs. 2.2) and physician office visits (8.8 vs. 6.3), and a higher proportion of patients in this cohort had neurosurgeon visits (15.8 vs. 7.7 %) (all differences, p < 0.05). In the 12-month post-index period, these two cohorts showed significant differences in the pattern of resource use. Compared with the medical therapy cohort, the surgical therapy cohort had a higher proportion of inpatient hospitalizations (98.3 vs. 13.6 %), ER visits (29.8 vs. 20.7 %), and specialist office visits (68.0 vs. 54.4 %), and more hospital outpatient visits (10.2 vs. 5.2) and physician office visits (21.2 vs. 15.0) (all differences, p < 0.05).
3.5 Treatment Sequence
Tumor resection surgery was used as the first-line treatment in 50.9 % of individuals with new episodes of acromegaly, of whom 77.2 % received no further treatment and 22.8 % received medical therapy as the second-line treatment. Medical therapy was used as the first-line treatment in 49.1 % of individuals with acromegaly, of whom 72.3 % did not receive second-line therapy, 12.3 % received second-line surgical therapy, 7.7 % had add-ons to the initial drug, and 7.7 % switched to another medication (Fig. 2).
Treatment sequence of commercially insured acromegalic individuals who received surgical and/or medical therapy during the 12-month post-index period. * represents the surgical therapy cohort (N = 228) included individuals with acromegaly who received surgical therapy as the first-line treatment (N = 202), as the second-line treatment (N = 24), or as the third-line treatment (N = 2); these two patients received surgery as the third-line treatment after they switched from one drug (first-line) to another drug (second-line); data not shown on this figure; † indicates that another drug was added to the initial drug; ‡ indicates that octreotide and octreotide long-acting release (LAR) were considered as one drug, and switching between octreotide and octreotide LAR was not considered as a switch of drug; $ indicates that the initial drug was discontinuded and another drug started
3.6 All-Cause Costs and Acromegaly-Associated Costs
During the 6-month pre-index period, individuals in the medical therapy cohort had higher monthly total healthcare costs ($US2818.4 vs. 1963.5) and pharmacy costs ($US1041.5 vs. 175.3) but lower monthly outpatient costs ($US929.6 vs. 1038.1) than the surgical therapy cohort (all p < 0.01). In the 12-month post-index period, individuals in the medical therapy cohort had lower monthly total healthcare costs ($US3076.5 vs. 5202.6), inpatient costs ($US347.7 vs. 2807.7), and outpatient costs ($US1366.6 vs. 1938.1) but higher pharmacy costs ($US1362.3 vs. 456.9) than did the surgical therapy cohort (all differences, p < 0.01) (Table 4).
Among the medical therapy cohort, the following proportions of various costs were associated with acromegaly: 56.0 % of monthly total healthcare costs, 25.8 % of inpatient costs, 33.3 % of outpatient costs, and 86.6 % of pharmacy costs. By comparison, in the surgical therapy cohort, the proportions were 52.5 % of the monthly total healthcare costs, 72.5 % of inpatient costs, 21.8 % of outpatient costs, and 59.3 % of pharmacy costs.
3.7 Subgroup Analysis in Patients with at Least 2 Years of Follow-Up
There were 240 acromegalic individuals with at least 2 years of post-index data. In the medical therapy cohort (N = 117), monthly total healthcare costs, outpatient costs, and pharmacy costs were slightly greater during the second-year post-index period followed by costs during the first-year post-index period (Table 5). In the surgical therapy cohort (N = 123), monthly total healthcare costs, inpatient costs, and outpatient costs were highest during the first-year post-index period, and monthly pharmacy costs were highest during the second-year post-index period. During the first-year post-index period, the surgical therapy cohort had much higher monthly total healthcare costs ($US5204.4 vs. 2807.6), inpatient costs ($US2706.0 vs. 268.0), outpatient costs ($US2031.4 vs. 1071.6), and lower pharmacy costs ($US467.1 vs. 1468.1) than did the medical therapy cohort (all differences, p < 0.01). However, this trend was reversed to some extent in the second-year post-index period, in that the surgical therapy cohort had lower monthly total healthcare costs ($US2158.5 vs. 2919.1) and outpatient costs ($US1082.2 vs. 1135.0) than the medical therapy cohort (both differences, p < 0.05).
4 Discussion
This study analyzed a large administrative claims database to assess the cross-sectional prevalence of comorbid conditions, treatment patterns/sequence, HRU, and costs among commercially insured individuals with newly recognized episodes of acromegaly who received surgical therapy and/or medical therapy in the USA. Consistent with the study by Burton et al. [5], we found that the prevalence of several major comorbidities was higher among the acromegalic individuals who received surgical and/or medical therapy during the post-index period. Of note, Broder et al. [12] concluded that complications associated with acromegaly, especially cardiovascular and musculoskeletal abnormalities, hypopituitarism, and sleep apnea, were commonly seen in individuals with acromegaly and increased utilization and costs in acromegaly patients; similarly, our study indicated that the clinical burden is substantial in this population. In addition, we observed that acromegalic individuals treated with surgical therapy had a higher prevalence of hypertension, sleep apnea, cardiac dysrhythmia/arrhythmia, and abnormal glucose than those treated with medical therapy during the post-index period. The impact of these complications was reflected in the higher healthcare costs.
During the 6-month pre-index period, healthcare resource use was comparable between the two study cohorts; however, individuals in the surgical therapy cohort utilized much greater resources in all healthcare settings than did those in the medical therapy cohort during the 12-month post-index period, suggesting a considerable economic burden associated with resection surgery and post-operative follow-up. The trend from cost analyses further validated this finding and showed that the surgical therapy cohort actually incurred lower costs during the pre-index period but had much higher costs in the 12-month post-index period compared with the medical therapy cohort. In our study, the surgery cohort comprised 228 patients, including 156 and 72 individuals with and without medical therapy, respectively. It is therefore possible that the costs could be higher in the surgical cohort at least partly due to this inclusion of patients with combination therapy, and that the costs associated with surgical treatment alone might be considerably lower. This notion is potentially supported by the fact that the overall proportion of patients treated with surgery for new episodes of acromegaly is somewhat lower than would be expected for a truly incident population. This fact suggests that our sample would have included some patients who were in fact presenting with disease recurrence, so accounting for the low proportion that went on to have surgery as first-line treatment (compared with a typical rate for a truly incident group) and the considerable number of such individuals who also needed second-line medical treatment.
Interestingly, our analysis of individuals with at least 2 years of post-index data is in line with the idea that, in the longer term, surgery may ultimately be associated with lower costs. Specifically, subgroup analysis showed that monthly total healthcare costs, inpatient costs, and outpatient costs were higher during the first-year post-index period and lower during the second-year post-index period in the surgical therapy cohort. This might have reflected favorable longer-term outcomes among individuals treated with surgery early after the initial acromegaly diagnosis. Of relevance, a study by Wilson et al. [15] on the economic burden among 53 Canadian patients with acromegaly who received a surgical procedure only (n = 27) or along with medical therapy (n = 26) observed that the mean annual surgical costs when averaged over 4 years was $US2400 less than the cost of medications. We also observed a positive relationship between drug costs and time, suggesting that, despite receiving costly surgical procedures, some individuals had persistent disease requiring subsequent pharmacologic treatments. This again may reflect that some patients in our surgical cohort could have had recurrent episodes of acromegaly, and were consequently less likely than incident patients to be cured with surgery alone. In the medical therapy cohort in our study, total healthcare costs were slightly higher during the second-year post-index period, primarily owing to the rising costs in the outpatient and pharmacy settings. Inpatient costs were the lowest during the second-year post-index period, perhaps suggesting that pharmacologic treatments were effective in preventing patients from experiencing acute and severe complications that necessitated hospitalization.
Future research should (1) explore patient characteristics associated with individuals who could not achieve surgically induced remission, (2) investigate other cost-effective treatment options for these individuals, and (3) use a longer follow-up period to accurately capture treatment patterns over time. It is important to understand the projection of lifetime costs of surgical versus medical therapy for acromegaly in future studies to establish whether the overall costs of medical treatment will rapidly overtake the upfront high surgical cost, and whether or how this differs for patients with newly diagnosed and recurrent disease.
4.1 Limitations
This study was subject to the following limitations common to most retrospective database analyses. The economic analysis was conducted from a total cost perspective, which included healthcare payments and any patient copayments/deductibles. Other costs such as indirect costs related to lost wages or lowered productivity were not considered. Healthcare claims used in this analysis were primarily used for administrative purposes in obtaining reimbursement for services provided to health plan members; hence, potential diagnostic and procedural coding inaccuracies might have occurred, causing the misclassification of certain diagnoses, events, or procedures of interest. It is possible that comorbidities might be underestimated, since coding for potential comorbidities may be poorly done, and, due to the nature of claims data, no clinical records were available in the database to evaluate acromegaly-associated comorbidities. Other limitations included the potential for bias in treatment cohort comparisons due to unmeasured confounders (e.g., disease severity, as the size and invasiveness of tumors were not available in the database). In addition, we used only a 6-month pre-index period for excluding patients with a diagnosis of acromegaly to identify newly recognized episodes of the condition and only required that individuals with acromegaly have at least 6 months of continuous health plan enrollment prior to the index date, to help ensure there were sufficient patients for analysis in our study sample. Acromegaly is challenging to diagnose and is often recognized late. Also, due to the nature of the claims database, it was not possible to know the disease history of the patient outside the current study period. Therefore, it is important to note that our study sample should not be regarded as a truly incident population, owing to the short pre-index period. More likely, it represents a mixture of patients, some of whom would be newly diagnosed, with others presenting with episodes of recurrent disease. We observed treatment patterns only during the 12-month post-index period, which may not have been a long enough period to capture the comprehensive and longitudinal picture necessary to fully understand patients’ treatment profiles. An important treatment goal for patients with acromegaly is to achieve biochemical control in terms of GH and insulin-like growth factor (IGF)-1 level; however, GH and IGF-1 data were not available in the current dataset. Another factor to consider here is the that the surgery cohort included patients with and without medical therapy, which—as mentioned above—we cannot be sure how our results might compare with an analysis that distinguished between cases that had surgery alone, surgery with medical therapy, and medical therapy alone in terms of economic burden, complications, and hospital admissions—an important potential focus for future research. Finally, given the dynamic pattern of care for patients with acromegaly in the clinical community, results derived from this study using data from 2007 to 2011 may not accurately reflect the current treatment patterns or economic burden of acromegaly.
5 Conclusions
Acromegaly poses a significant economic burden on individual patients and society as a whole. There is a paucity of published data with respect to the economic burden associated with the condition stratified by type of treatment that the patient initially receives. By comparing patient characteristics, treatment patterns/sequence, and economic outcomes associated with the type of acromegaly treatment, our findings may provide insights to the healthcare community and contribute to the literature. Future research is needed to assess the incremental economic burden associated with acromegaly and to conduct cost-effective analysis on treatment options to cure or decelerate the progression of the disease course.
References
Melmed S. Medical progress: acromegaly. N Engl J Med. 2006;355:2558–73.
Cook DM, Ezzat S, Katznelson L, et al. AACE medical guidelines for clinical practice for the diagnosis and treatment of acromegaly. Endocr Pract. 2004;10:213–25.
Holdaway IM, Rajasoorya C. Epidemiology of acromegaly. Pituitary. 1999;2:29–41.
Reddy R, Hope S, Wass J. Acromegaly. BMJ. 2010;341:c4189.
Burton T, Le Nestour E, Bancroft T, et al. Real-world comorbidities and treatment patterns of patients with acromegaly in two large US health plan databases. Pituitary. 2013;16:354–62.
Ben-Shlomo A, Sheppard MC, Stephens JM, et al. Clinical, quality of life, and economic value of acromegaly disease control. Pituitary. 2011;14:284–94.
Ayuk J, Sheppard MC. Does acromegaly enhance mortality? Rev Endocr Metab Disord. 2008;9:33–9.
Holdaway IM, Bolland MJ, Gamble GD. A meta-analysis of the effect of lowering serum levels of GH and IGF-I on mortality in acromegaly. Eur J Endocrinol. 2008;159:89–95.
Giustina A, Chanson P, Kleinberg D, et al. Expert consensus document: a consensus on the medical treatment of acromegaly. Nat Rev Endocrinol. 2014;10:243–8.
Katznelson L, Laws ER Jr, Melmed S, et al. Acromegaly: an endocrine society clinical practice guideline. J Clin Endocrinol Metab. 2014;99:3933–51.
Broder M, Neary M, Chang E, et al. Healthcare utilization and costs in acromegaly patients in the United States. June 24, 2012 Presentation Number: SUN-323 at The Endocrine Society’s 94th Annual Meeting and Expo, June 23–26, 2012, Houston. Endocr Rev. 2012;33.
Broder MS, Neary MP, Chang E, et al. Treatments, complications, and healthcare utilization associated with acromegaly: a study in two large United States databases. Pituitary. 2014;17:333–41.
Truven Health Analytics. Data, Databases and Online Tools. MarketScan Research Databases. 2013. http://www.truvenhealth.com/your_healthcare_focus/pharmaceutical_and_medical_device/data_databases_and_online_tools.aspx. Accessed 8 Oct 2013.
Bureau of Labor Statistics. Consumer price index inflation calculator (2011 dollars). Washington, DC: US Bureau of Labor Statistics 2013. http://www.bls.gov/cpi/data.htm. Accessed 10 Oct 2013.
Wilson LS, Shin JL, Ezzat S. Longitudinal assessment of economic burden and clinical outcomes in acromegaly. Endocr Pract. 2001;7:170–80.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
This study was sponsored by Ipsen Pharma SAS.
Conflicts of interest
Jerome Dinet, Siham Brulais, and Sylvie Gabriel are full-time employees of Ipsen Pharma SAS. Sharvari Bhurke is, and Chien-Chia Chuang and Shih-Yin Chen were, employees of Evidera, which provides consulting and other research services to pharmaceutical, device, government, and non-government organizations. In their salaried positions, they work/ed with a variety of companies and organizations and are/were precluded from receiving payment or honoraria directly from these organizations for services rendered. Evidera received funding from Ipsen Pharma SAS for the work performed by Evidera employees.
Ethical approval
This was a retrospective observational study using de-identified data from a commercial claims database that represented the healthcare experiences of over 150 million individuals across the USA. Therefore, our study had no effect on the treatment decisions of patients or healthcare providers. Because this study used only de-identified patient records and did not involve the collection, use, or transmittal of individually identifiable data, it did not require Institutional Review Board approval.
Appendix
Appendix
Tumor resection surgery for acromegaly and associated current procedural terminology (CPT) codes and International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) procedure codes
Procedure type | Code | Code description | Code type |
|---|---|---|---|
Excision of pituitary gland | 61546 | Craniotomy for hypophysectomy or excision of pituitary tumor, intracranial approach | CPT |
61548 | Hypophysectomy or excision of pituitary tumor, transnasal or transseptal approach, nonstereotactic | CPT | |
62165 | Neuroendoscopy, intracranial; with excision of pituitary tumor, transnasal or trans-sphenoidal approach | CPT | |
07.61 | Partial excision of pituitary gland, transfrontal approach | ICD-9-CM | |
07.62 | Partial excision of pituitary gland, transsphenoidal approach | ICD-9-CM | |
07.63 | Partial excision of pituitary gland, unspecified approach | ICD-9-CM | |
07.64 | Total excision of pituitary gland, transfrontal approach | ICD-9-CM | |
07.65 | Total excision of pituitary gland, transsphenoidal approach | ICD-9-CM | |
07.68 | Total excision of pituitary gland, other specified approach | ICD-9-CM | |
07.69 | Total excision of pituitary gland, unspecified approach | ICD-9-CM |
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (http://creativecommons.org/licenses/by-nc/4.0/), which permits any noncommercial use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Chuang, CC., Bhurke, S., Chen, SY. et al. Treatment Patterns and Economic Burden in Patients Treated for Acromegaly in the USA. Drugs - Real World Outcomes 2, 299–309 (2015). https://doi.org/10.1007/s40801-015-0039-0
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40801-015-0039-0