Abstract
Purpose of Review
Sleep deprivation is a global health issue, and the resultant cognitive deficits can be debilitating. A series of studies reported success with individually neuronavigated transcranial magnetic stimulation (TMS), coupled with online task performance, in substantially reducing performance deficits in working memory in healthy adults caused by 2 days of total sleep depression. This paradigm of coupling TMS with online task performance has been referred to as Cognitive Paired Associative Stimulation (C-PAS). This review describes those studies and the research since using various TMS paradigms to remediate working memory deficits in sleep deprivation.
Recent Findings
Three such studies were found, but none replicated the earlier findings. However, in each case, there were differences in study design that might explain the negative findings and inform future methodological choices and to underline the need to combine TMS with brain imaging guidance.
Summary
Online task performance during TMS, as done in the C-PAS paradigm, appears to be essential to demonstrating lasting remediation of working memory deficits induced by sleep deprivation. This observation highlights the importance of state-dependency in determining the effects of TMS. Further work needs to be done to clarify the potential role of C-PAS in alleviating the effects of sleep deprivation and studying cognitive processes affected by sleep.
Similar content being viewed by others
Introduction
Sleep plays a prominent role in the maintenance of memory processes in the brain, for example in the consolidation of declarative memories [1, 2]. This can be observed most readily by examining the consequences of sleep deprivation, which can lead to decreases in the synaptic plasticity needed to establish long-term memories [2, 3], as well as disruption of brain networks underlying working memory [4], neural effects opposite to the beneficial processes that occur in normal sleep. Recently developed brain stimulation techniques have provided tools to modulate the sleep-deprived brain and study the effects of sleep deprivation on memory. To demonstrate such an approach, the present review will specifically look at transcranial magnetic stimulation (TMS) and examine its use in the remediation of performance deficits in working memory caused by sleep deprivation.
TMS and Its Use in Studying Sleep Deprivation
TMS is a noninvasive form of brain stimulation that uses magnetic induction to modulate brain function both acutely and in long-lasting ways. TMS has been FDA-cleared as a therapy for treatment-resistant depression as well as for obsessive compulsive disorder (OCD), migraine, and smoking cessation, and studies suggest that it shows potential for the treatment of other psychiatric and neurological illnesses. TMS can also be used to investigate cognitive function by disrupting or facilitating ongoing performance of cognitive tasks. With repeated application, TMS can modulate cognitive function in more long-lasting ways: for example, it has shown promise in the remediation of memory and executive function deficits in sham-controlled clinical trials with patients with Alzheimer’s disease (e.g. [5,6,7]).
TMS has been shown to be useful in sleep research as well, for instance as a means to study the balance of neural excitation and inhibition in cerebral cortex during sleep [8] or to modulate ongoing sleep EEG oscillations [9]. Moreover, a growing body of research indicates that TMS may be a valuable tool in diagnosing and treating sleep disorders, such as chronic insomnia, obstructive sleep apnea syndrome, and restless leg syndrome [10, 11]. In the area of sleep deprivation, TMS was initially used to explore physiological changes in cortical activity that such deprivation causes. In one of the earliest of these studies, paired-pulse TMS was applied to the motor cortex of healthy adults before and after 24 h of total sleep deprivation [12]. Using paired-pulse stimulation, motor responses evoked by the stimuli can reflect excitatory or inhibitory activity depending on the time intervals between the pulses. Compared to baseline, subjects in Civardi et al. showed a flattening of responses in both excitatory and inhibitory time interval regions, suggesting a general hypoactivity in motor cortex caused by sleep deprivation [12]. Following this finding, later TMS studies of healthy adults and depressed patients have shown changes in measures of cortical excitability, excitatory-inhibitory balance, and plasticity in cortex due to sleep deprivation [13,14,15].
Initial Studies Reporting Cognitive Paired Associative Stimulation (C-PAS) Remediation of Working Memory Deficits in Sleep Deprivation
As TMS has been reported to have the capacity to enhance cognitive functions (e.g., [16]), and as sleep deprivation causes pronounced deficits in those functions, it is reasonable to ask whether TMS could be used to remediate cognitive performance deficits caused by sleep deprivation. The first attempt to use TMS in this way was reported in 2008 [17••], and it was based on the combination of two novel techniques for enhancing functional network engagement using TMS. The first technique involved using functional magnetic resonance imaging (fMRI) acquired during the performance of a cognitive task to highlight nodes of brain networks involved with the task to use for targeting TMS on an individual basis. This technique was later shown to be the most effective means of targeting TMS to date [18]. The second method was based on the growing number of observations in the brain stimulation field that controlling brain state plays a key role in yielding effective stimulation [19, 20]. Further, controlling brain state during cumulative TMS could lead to long-lasting functional changes. This was first seen using the paired associative stimulation (PAS) paradigm, where it was shown that synaptic efficacy within the cortico-spinal tract could be enhanced by pairing TMS stimulation of sensorimotor cortex with electrical stimulation of the median nerve [21]. The generalization of this multi-modal pairing of functional activation with individualized fMRI targeted TMS to enhance the action of a functional brain network is termed Cognitive Paired Associative Stimulation, or C-PAS [22]. Over a series of experiments [17••, 23•, 24••], we posited the C-PAS approach could be used to enhance the resilience of a working memory network affected by sleep deprivation, remediating performance deficits it caused.
In our initial proof-of-concept study, we investigated which specific parameters of online TMS might produce performance enhancement in a working memory task [23•]. The task used was called a delayed match-to-sample (DMS) task. In this task, one to six letters appeared for 3 s, followed by a 7-s delay period, and then a 3-s test period in which a probe letter appeared, during which subjects were to respond with a right or left finger press as fast as possible based on whether or not the probe letter had also appeared in the initial set of letters. In a first experiment with 15 healthy adult volunteers, we applied active and sham rTMS to left dorsolateral prefrontal and midline parietal cortex at 1, 5, and 20 Hz, applied in trains at an intensity of 100% motor threshold during the delay period of the task, and found that only 5 Hz stimulation to parietal cortex produced significant speeding of reaction time. In a new group of 22 participants, we stimulated the midline parietal cortex at 5 Hz during the delay and test phases of the DMS task and found only delay phase stimulation produced reaction time speeding.
After demonstrating that we could enhance working memory performance with a specific set of online parameters, we proceeded to apply the C-PAS paradigm in the context of sleep deprivation. Fifteen healthy adults were practiced on the DMS task [17••]. After an fMRI session during which the DMS task was performed, the subjects went through 2 days of total sleep deprivation in a sleep lab with continuous EEG monitoring, followed by a second fMRI session and a TMS session. During the online TMS session, the subjects performed the DMS task while receiving trains of 5 Hz rTMS during the delay period at an intensity of 100% motor threshold. Active and sham TMS were applied at three different cortical locations. Two were at nodes in left lateral occipital complex and in midline parietal cortex of a brain network found in a previous fMRI study to be both activated by the DMS task and sensitive to sleep deprivation [25]. The third targeted site was 1 cm posterior to the left lateral occipital complex node, just outside the network. Reaction time (RT) was sped up relative to sham with TMS to the sites within the network, significantly so for the lateral occipital site, while TMS to the target 1 cm posterior to lateral occipital site led to slower RT performance no different from sham. Accuracy was not affected by TMS. It was concluded that the TMS applied to the targeted working memory network remediated the slowing in performance caused by sleep deprivation. Importantly, there was a significant correlation between the degree the TMS sped RT and the drop in fMRI activation in the network pre- and post-sleep deprivation, with TMS most significantly aiding those with the biggest drop in network activation, demonstrating a direct brain-behavior relationship in the sleep deprivation-related TMS effect.
The remediation by TMS of a sleep deprivation-caused working memory deficit in Luber et al. [17••] was an acute effect. This could be demonstrated as rTMS was applied only every other DMS trial, and there was no performance enhancement seen in the non-TMS trials, leading to the conclusion that the effect wore off quickly, before the succeeding trial. Thus, we followed up with an attempt to generate a long-lasting effect [24••]. We followed a similar design, with 2 days of total sleep deprivation book-ended by MRI sessions, but this time instead of having a single TMS session at the end of the sleep deprivation period, we ran four 60-min TMS sessions during the sleep deprivation period, two on the first day and two on the second. We continued our online approach of applying 5 Hz rTMS during the delay period of the DMS task, again targeting the left lateral occipital complex, where the largest acute effect had been found. We expected that the repeated TMS sessions would build up a cumulative effect of resilience against sleep deprivation in the targeted network. We ran 55 healthy adults, divided into four groups: half of the participants received active TMS, the other half sham, and half were sleep deprived while the other half were not. DMS performance was measured at baseline and then after the 2-day sleep deprivation period—this time without concurrent TMS, and at least 18 h since the last TMS session. We found that while the sleep-deprived group that received sham TMS showed the typical performance deficits seen in the DMS task—frequent lapsing (non-response in task trials) and significant RT slowing—the sleep-deprived group that received active TMS did not display any RT slowing and had minimal lapsing—in short, they were indistinguishable in their DMS performance from the two groups who did not receive sleep deprivation. The multiple sessions of active TMS during the sleep deprivation period had apparently served to protect that group from the cognitive deficits normally caused by sleep deprivation in a manner that lasted at least 18 h after the last TMS session. Interestingly, the only significant pre-post fMRI difference between the two sleep deprivation groups was that there was a significant activation during DMS performance of the left lateral occipital cortex in the active TMS group but not in the sham group, suggesting that the TMS caused a change in the targeted region that may have been related to the resilience they developed to sleep deprivation in the DMS task.
More Recent Studies Using TMS to Affect Working Memory in Sleep Deprivation
Other groups have also used TMS to enhance working memory performance in the face of deficits caused by sleep deprivation. In one study, a design similar to Luber et al. [17••] was used, with MRI sessions book-ending a period of total sleep deprivation and a TMS session occurring at the end of the sleep deprivation, using trains of 5 Hz rTMS at 100% motor threshold [26•]. There were a number of design differences too: the sleep deprivation period was 24 h rather than 48 h, the working memory task used was the n-back (0, 1, and 2) rather than a DMS, the TMS was applied offline (i.e., this was not C-PAS, which requires online TMS), and the design was between group, with three groups randomized by TMS targeting condition, using active TMS to medial prefrontal or medial occipital cortical sites, or sham TMS. The authors found that in sleep-deprived subjects, for the high load case (i.e., 2-back) of the n-back, accuracy after TMS to medial occipital cortex was higher and RT was unchanged from baseline, while performance was worse after sleep deprivation for 0- and 1-back cases. However, it was not clear how any meaningful statistical analysis could be performed: the report was labeled a pilot study, with only six subjects to distribute to the three groups. No follow-up on the study has been published to date by any of the authors.
In another study, 17 healthy adults were given 24 h of total sleep deprivation and performed two DMS tasks (one using 1–6 letters, the other 1–6 numbers) before and after the sleep deprivation period, and then again after an immediately following a session of TMS, in which twenty 10-s trains of 5 Hz rTMS were applied offline to left dorsolateral prefrontal cortex (DLPFC) [27•]. Both group mean accuracy and RT performance in the DMS worsened with sleep deprivation, then improved back to baseline levels after the TMS; however, these changes were not significant. There was a claim that post hoc testing showed a significant increase in performance accuracy in one of the two working memory tasks with TMS in sleep-deprived subjects, but this should be discounted both because the ANOVA the post hoc tests were following up had no significant effects and because there were no corrections for multiple comparisons in the post hoc analysis, which would have left the result nonsignificant. In addition, TMS targeting of DLPFC in this study suffered from the use of the 5-cm rule, which has been shown to be an imprecise method of locating DLPFC for TMS [28]. Further, subjects received no practice on the task, so any performance improvements could have been attributable to a practice effect, especially as there were no active or sham controls for the TMS condition. Finally, the offline design again was not C-PAS, further supporting the importance of brain state during stimulation.
In a more recent study which showed some similarities to Luber et al. [24••], 66 healthy adults were randomized to active and sham groups and received 24 h of total sleep deprivation [29•]. Similar to the earlier study, an attempt was made to generate a cumulative effect with multiple TMS sessions given during the sleep deprivation period. Forty 5-s trains of 10 Hz rTMS were applied to left DLPFC at 80% of motor threshold in each of two sessions, one performed 9 h into the 24 h sleep deprivation period, and the other 21 h in. Two tasks, the n-back and Stroop color-word task, were given at times 0, 6, 12, 18, and 24 h into the 24 h sleep deprivation period. There were no significant differences in task performance between active and sham groups across the five test times. However, this negative result may have been due to problematic decisions regarding TMS targeting and parameters: notably, TMS was targeted using the 5-cm rule, which is a non-optimal means of locating DLPFC. Moreover, at 80% of motor threshold, the TMS intensity used was much lower than that used previously in cases when differences in cognitive performance were seen between active and sham TMS conditions (e.g., [17••, 24••]). Most importantly, the C-PAS paradigm was not used, again demonstrating that the offline design is ineffective.
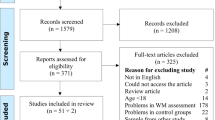
Lessons Learned in the Three Follow-Up Studies
In summary, the three follow-up studies did not demonstrate strong support for the two original reports that found both acute [17••] and longer-lasting [24••] improvements to sleep deprivation–related working memory deficits. However, there were design and technical problems in each of those three studies. Most notably, the replication attempts failed to replicate the C-PAS paradigm, i.e., TMS was not given during task performance, nor was targeting guided by fMRI. Other limitations include the very small sample size in Martinez-Cancino et al. [26•], the lack of control condition and confound with task practice in Guo et al. [27•], the very low TMS dose used in Li et al. [29•], and the use of the 5-cm rule for targeting DLPFC in both Guo et al. [27•] and Li et al. [29•] (see Table 1). These experimental issues weaken conclusions that can be drawn from the three later studies. On the other hand, looked at in a different light, contrasting these studies with the earlier work may represent a positive contribution towards a paradigm to reduce working memory deficits in sleep deprivation. All three studies used a 24-h total sleep deprivation period, while Luber et al. used a 48-h period [17••, 24••]. This suggests that an effect of TMS on task performance might be more clearly seen at longer deprivation durations, where the cognitive deficits are more profound. The three studies all used offline TMS, that is, TMS was applied separately from when task performance was assessed. There is reason to believe that a functional targeting approach using online TMS (i.e., TMS applied in combination with the task) might enhance the capacity of the stimulation to modulate the targeted function [22, 30], as the results of doing so in Luber et al. [17••, 24••] support. In line with this approach, preliminary pilot work to optimize TMS parameters relative to the working memory task such as stimulation frequency and placement of the stimulus train relative to the phase of the task, such as was done by Luber et al. [23•], seems recommended. Also important is the targeting approach. Guo et al. [27•] and Li et al. [29•] used the 5-cm rule of locating and stimulating DLPFC. Using such a scalp-based method has been shown to be far less efficacious in generating a cognitive TMS effect than imaging methods, especially through the use of individualized fMRI-guided targeting [18]. But more essentially, in contrast with the two earlier studies, the three later studies did not perform the step of identifying a brain network both involved with their working memory tasks and sensitive to sleep deprivation that they could then proceed to engage with TMS. By not doing so, these studies help make the case that TMS can most effectively be used within an experimental context of brain imaging.
Convergent Evidence Suggesting the Effectiveness of TMS in Sleep Deprivation
Beyond the TMS studies of working memory just discussed, there has also been convergent evidence from other areas of sleep research involving noninvasive magnetic and electric brain stimulation techniques that encourage further work in using TMS to remediate sleep deprivation–caused cognitive deficits. For example, in animal research, experiments using low-amplitude magnetic stimulation in rodents after sleep deprivation and employing learning and memory tasks involving maze learning and object recognition found that the stimulation fully remedied performance deficits caused by lack of sleep [31]. Neuromodulation using noninvasive electrical stimulation with sleep deprivation has also resulted in cognitive performance enhancements. In two sham-controlled studies in which healthy adult humans received 30 min of anodal 2 mA transcranial direct current stimulation (tDCS) over the left DLPFC during 36 h of total sleep deprivation, subjects receiving active stimulation showed improved performance on vigilance tasks, although not so on a DMS task [32, 33]. In a more recent sham-controlled pilot study in which healthy volunteers received anodal 2 mA tDCS to left DLPFC during 30 h of total sleep deprivation, subjects receiving active stimulation showed improved performance on vigilance and working memory tasks [34]. In another recent report, sleep deprivation in healthy adults prevented the LTP-like effects of anodal tDCS from occurring while reversing the LDP-like effects of cathodal tDCS, both of which can impact cognitive performance [35]. Using TMS in a clinical setting with sleep-deprived patients has also resulted in cognitive improvements: in a group of 42 patients suffering from obstructive sleep apnea, a session of a form of TMS known as intermittent theta burst stimulation resulted in significant improvements in performance in working memory, sustained attention, and visual memory tasks [36]. Overall, when added to the initial results of significant working memory performance enhancements [17••, 24••], these other findings from noninvasive magnetic and electric brain stimulation techniques reinforce the promise of TMS as a means of remediating the deficits in cognition, especially in working memory, caused by sleep deprivation. Further, it should also be pointed out that in all of the TMS studies using sleep deprivation cited here, as well as others (e.g., [37]), no severe side effects, including seizures, were reported. This indicates that TMS can be used safely when employing sleep deprivation, although some caution should be exercised as there is evidence from epilepsy research and from other brain stimulation studies that sleep deprivation can lower seizure threshold [38].
Potential Uses for TMS-Based Sleep Deprivation Research
The development of brain stimulation techniques to moderate cognitive deficits caused by sleep deprivation could impact research in two ways. First and most directly, they could be used to study the brain mechanisms underlying these deficits in the hopes of developing remediation techniques. Sleep deprivation is a global health problem, and while some people suffering its effects can be helped via lifestyle changes (e.g., adolescents losing sleep due to excessive use of the Internet), many suffer from illnesses that include chronic sleep deprivation or are members of professions (e.g., warfighters, transport operators) where sleep deprivation is unavoidable [39]. Cognitive effects of sleep loss include deficits in attention, in executive function and decision-making, in working memory and in long-term declarative memory [3, 40]. The neural causes for these deficits likely occur on multiple spatial and temporal scales in brain systems. For example, at the cellular level, sleep deprivation interferes with synaptic mechanisms of long-term potentiation (LTP) and plasticity needed for the formation of long-term memories, while at the network level, it interferes with oscillatory activity in medial temporal memory networks needed for memory consolidation [2]. To affect processes at the cellular level, use of multiple weeks of TMS sessions, as used for instance in treating depression, might cause epigenetic synaptic changes that could affect plasticity involved with long-term memory. In the latter case, the fMRI-TMS targeting approach used by Luber et al. [24••] to generate resilience to the effects of sleep deprivation on working memory might also work if networks supporting long-term memory were targeted. In this regard, Romanella et al. [41] provide a framework for using noninvasive brain stimulation in the context of age-related brain network changes associated with sleep and sleep loss and memory and cognition.
In a second area of possible impact, brain stimulation combined with sleep deprivation can be used as a means of studying the neural bases of cognitive deficits caused by psychiatric and neurological diseases, with the goal of developing memory remediation paradigms. In healthy adults, sleep deprivation provides a means to generate a reversible cognitive deficit whose neural mechanisms can then be explored using brain stimulation. For example, as described above, a series of experiments was performed utilizing both sleep-deprived and non-sleep-deprived volunteers in which an fMRI-guided rTMS paradigm was developed that remediated the working memory deficits caused by sleep deprivation [17••, 23•, 24••, 25]. The knowledge and techniques learned from those studies suggested an analogy with the deficits in working memory associated with aging, and the paradigm was then successfully adapted in a study of working memory in older adults [42]. Using a more difficult DMS task in which participants had to not just remember but alphabetize random letter strings, individualized fMRI-guided 5 Hz rTMS applied online to a group of older adults increased the accuracy of their memory performance. This result, based on sleep deprivation research, represents a first step towards studying the remediation of the working memory deficits that occur with normal aging.
Conclusion
Sleep deprivation is a global health issue and, in many cases, resistant to easy treatment. As reviewed here, in the last few decades, noninvasive brain stimulation, notably TMS, has been used to investigate cortical processing related to cognitive deficits caused by sleep deprivation, primarily using working memory as a representative cognitive process. There has been accumulating evidence for the effects of brain stimulation on cognitive performance in sleep deprivation: the initial successes in developing the C-PAS paradigm for long-lasting TMS remediation of working memory, the lessons learned from more recent attempts following up that success, and convergent positive results from other brain stimulation studies of cognition and sleep deprivation in animals, healthy volunteers, and patients. Thus, there appears to be great merit in the idea of continued work using C-PAS in the development of therapeutic approaches to alleviating the effects of sleep deprivation, of studying cognitive processes affected by sleep, and as a laboratory for exploring functional resilience in cortical networks.
Data Availability
Not applicable.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Raven F, Van der Zee EA, Meerlo P, Havekes R. The role of sleep in regulating structural plasticity and synaptic strength: implications for memory and cognitive function. Sleep Med Rev. 2018;39:3. https://doi.org/10.1016/j.smrv.2017.05.002.
Abel T, Havekes R, Saletin JM, Walker MP. Sleep, plasticity and memory from molecules to whole-brain networks. Curr Biol. 2013;23(17):R774–88. https://doi.org/10.1016/j.cub.2013.07.025.
Cousins JN, Fernandez G. The impact of sleep deprivation on declarative memory. Prog Brain Res. 2019;246:27–53. https://doi.org/10.1016/bs.pbr.2019.01.007.
Krause AJ, Simon EB, Mander BA, Greer SM, Saletin JM, Goldstein-Piekarski AN, et al. The sleep-deprived human brain. Nat Rev Neurosci. 2017;18(7):404–18. https://doi.org/10.1038/nrn.2017.55.
Zhao J, Li Z, Cong Y, Zhang J, Tan M, Zhang H, et al. Repetitive transcranial magnetic stimulation improves cognitive function of Alzheimer’s disease patients. Oncotarget. 2017;8(20):33864–71. https://doi.org/10.18632/oncotarget.13060.
Koch G, Bonni S, Pellicciari MC, Casula EP, Mancini M, Esposito R, et al. Transcranial magnetic stimulation of the precuneus enhances memory and neural activity in prodromal Alzheimer’s disease. Neuroimage. 2018;169:302–11. https://doi.org/10.1016/j.neuroimage.2017.12.048.
Sabbagh M, Sadowsky C, Tousi B, Agronin ME, Alva G, Armon C, et al. Effects of a combined transcranial magnetic stimulation (TMS) and cognitive training intervention in patients with Alzheimer’s disease. Alzheimers Dement. 2020;16(4):641–50. https://doi.org/10.1016/j.jalz.2019.08.197.
Avesani M, Formaggio E, Fuggetta G, Fiaschi A, Manganotti P. Corticospinal excitability in human subjects during nonrapid eye movement sleep: single and paired-pulse transcranial magnetic stimulation study. Exp Brain Res. 2008;187(1):17–23. https://doi.org/10.1007/s00221-008-1274-3.
Manganotti P, Formaggio E, Del Felice A, Storti SF, Zamboni A, Bertoldo A, et al. Time-frequency analysis of short-lasting modulation of EEG induced by TMS during wake, sleep deprivation and sleep. Front Hum Neurosci. 2013;7:767. https://doi.org/10.3389/fnhum.2013.00767.
Lanza G, Fisicaro F, Cantone M, Pennisi M, Cosentino FII, Lanuzza B, et al. Repetitive transcranial magnetic stimulation in primary sleep disorders. Sleep Med Rev. 2023;67:101735. https://doi.org/10.1016/j.smrv.2022.101735.
Nardone R, Sebastianelli L, Versace V, Brigo F, Golaszewski S, Pucks-Faes E, et al. Effects of repetitive transcranial magnetic stimulation in subjects with sleep disorders. Sleep Med. 2020;71:113–21. https://doi.org/10.1016/j.sleep.2020.01.028.
Civardi C, Boccagni C, Vicentini R, Bolamperti L, Tarletti R, Varrasi C, et al. Cortical excitability and sleep deprivation: a transcranial magnetic stimulation study. J Neurol Neurosurg Psychiatry. 2001;71(6):809–12. https://doi.org/10.1136/jnnp.71.6.809.
Kreuzer P, Langguth B, Popp R, Raster R, Busch V, Frank E, et al. Reduced intra-cortical inhibition after sleep deprivation: a transcranial magnetic stimulation study. Neurosci Lett. 2011;493(3):63–6. https://doi.org/10.1016/j.neulet.2011.02.044.
Kuhn M, Maier JG, Wolf E, Mainberger F, Feige B, Maywald S, et al. Indices of cortical plasticity after therapeutic sleep deprivation in patients with major depressive disorder. J Affect Disord. 2020;277:425–35. https://doi.org/10.1016/j.jad.2020.08.052.
Kuhn M, Wolf E, Maier JG, Mainberger F, Feige B, Schmid H, et al. Sleep recalibrates homeostatic and associative synaptic plasticity in the human cortex. Nat Commun. 2016;7:12455. https://doi.org/10.1038/ncomms12455.
Luber B, Lisanby SH. Enhancement of human cognitive performance using transcranial magnetic stimulation (TMS). Neuroimage. 2014;85(Pt 3(0 3)):961–70. https://doi.org/10.1016/j.neuroimage.2013.06.007.
•• Luber B, Stanford AD, Bulow P, Nguyen T, Rakitin BC, Habeck C, et al. Remediation of sleep-deprivation-induced working memory impairment with fMRI-guided transcranial magnetic stimulation. Cereb Cortex. 2008;18(9):2077–85. https://doi.org/10.1093/cercor/bhm231. The first report of the successful use of C-PAS to acutely remediate working memory deficits due to sleep deprivation.
Sack AT, Cohen Kadosh R, Schuhmann T, Moerel M, Walsh V, Goebel R. Optimizing functional accuracy of TMS in cognitive studies: a comparison of methods. J Cogn Neurosci. 2009;21(2):207–21. https://doi.org/10.1162/jocn.2009.21126.
Romei V, Thut G, Silvanto J. Information-based approaches of noninvasive transcranial brain stimulation. Trends Neurosci. 2016;39(11):782–95. https://doi.org/10.1016/j.tins.2016.09.001.
Silvanto J, Pascual-Leone A. State-dependency of transcranial magnetic stimulation. Brain Topogr. 2008;21(1):1–10. https://doi.org/10.1007/s10548-008-0067-0.
Stefan K, Kunesch E, Cohen LG, Benecke R, Classen J. Induction of plasticity in the human motor cortex by paired associative stimulation. Brain. 2000;123(Pt 3):572–84. https://doi.org/10.1093/brain/123.3.572.
Sathappan AV, Luber BM, Lisanby SH. The dynamic duo: combining noninvasive brain stimulation with cognitive interventions. Prog Neuropsychopharmacol Biol Psychiatry. 2019;89:347–60. https://doi.org/10.1016/j.pnpbp.2018.10.006.
• Luber B, Kinnunen LH, Rakitin BC, Ellsasser R, Stern Y, Lisanby SH. Facilitation of performance in a working memory task with rTMS stimulation of the precuneus: frequency- and time-dependent effects. Brain Res. 2007;1128(1):120–9. https://doi.org/10.1016/j.brainres.2006.10.011. First report of the use of C-PAS to improve working memory in healthy adult volunteers.
•• Luber B, Steffener J, Tucker A, Habeck C, Peterchev AV, Deng ZD, et al. Extended remediation of sleep deprived-induced working memory deficits using fMRI-guided transcranial magnetic stimulation. Sleep. 2013;36(6):857–71. https://doi.org/10.5665/sleep.2712. Demonstration of long-lasting remediation of working memory deficits in sleep-deprived adults using repeated sessions of C-PAS.
Habeck C, Rakitin BC, Moeller J, Scarmeas N, Zarahn E, Brown T, et al. An event-related fMRI study of the neurobehavioral impact of sleep deprivation on performance of a delayed-match-to-sample task. Brain Res Cogn Brain Res. 2004;18(3):306–21. https://doi.org/10.1016/j.cogbrainres.2003.10.019.
• Martinez-Cancino MDP, Azpiroz-Leehan J, Jimenez-Angeles L, Garcia-Quintanar A, Santana-Miranda R. Effects of high frequency rTMS on sleep. deprivation: a pilot study. Annu Int Conf IEEE Eng Med Biol Soc. 2016;2016:5937–40. https://doi.org/10.1109/EMBC.2016.7592080. First report of attempted use of offline rTMS to alleviate the effects of sleep deprivation on working memory.
• Guo Z, Jiang Z, Jiang B, McClure MA, Mu Q. High-frequency repetitive transcranial magnetic stimulation could improve impaired working memory induced by sleep deprivation. Neural Plast. 2019;2019:7030286. https://doi.org/10.1155/2019/7030286. An attempt to acutely enhance working memoryperformance in sleep deprived subjects using offline rTMS.
Fitzgerald PB, Maller JJ, Hoy KE, Thomson R, Daskalakis ZJ. Exploring the optimal site for the localization of dorsolateral prefrontal cortex in brain stimulation experiments. Brain Stimul. 2009;2(4):234–7. https://doi.org/10.1016/j.brs.2009.03.002.
• Li S, Zhou H, Yu Y, Lyu H, Mou T, Shi G, et al. Effect of repetitive transcranial magnetic stimulation on the cognitive impairment induced by sleep deprivation: a randomized trial. Sleep Med. 2021;77:270–8. https://doi.org/10.1016/j.sleep.2020.06.019. A recent attempt touse offline rTMS in cumulative sessions during sleep deprivation to generate longer-lasting remediation of working memory deficits.
Bikson M, Name A, Rahman A. Origins of specificity during tDCS: anatomical, activity-selective, and input-bias mechanisms. Front Hum Neurosci. 2013;7:688. https://doi.org/10.3389/fnhum.2013.00688.
Estrada C, Fernandez-Gomez FJ, Lopez D, Gonzalez-Cuello A, Tunez I, Toledo F, et al. Transcranial magnetic stimulation and aging: effects on spatial learning and memory after sleep deprivation in Octodon degus. Neurobiol Learn Mem. 2015;125:274–81. https://doi.org/10.1016/j.nlm.2015.09.011.
McIntire LK, McKinley RA, Goodyear C, Nelson J. A comparison of the effects of transcranial direct current stimulation and caffeine on vigilance and cognitive performance during extended wakefulness. Brain Stimul. 2014;7(4):499–507. https://doi.org/10.1016/j.brs.2014.04.008.
McIntire LK, McKinley RA, Nelson JM, Goodyear C. Transcranial direct current stimulation versus caffeine as a fatigue countermeasure. Brain Stimul. 2017;10(6):1070–8. https://doi.org/10.1016/j.brs.2017.08.005.
Cheng JX, Zhao X, Qiu J, Jiang Y, Ren J, Sun S, et al. Effects of transcranial direct current stimulation on performance and recovery sleep during acute sleep deprivation: a pilot study. Sleep Med. 2021;79:124–33. https://doi.org/10.1016/j.sleep.2021.01.014.
Salehinejad MA, Ghanavati E, Reinders J, Hengstler JG, Kuo MF, Nitsche MA. Sleep-dependent upscaled excitability, saturated neuroplasticity, and modulated cognition in the human brain. Elife. 2022;11:e69308. https://doi.org/10.7554/eLife.69308.
Han X, Cai S, Gui H, Chen R. Transcranial magnetic stimulation cortical oscillations and improve cognition in obstructive sleep apnea patients. Brain Behav. 2023;13(4):e2958. https://doi.org/10.1002/brb3.2958.
Anderson B, Mishory A, Nahas Z, Borckardt JJ, Yamanaka K, Rastogi K, et al. Tolerability and safety of high daily doses of repetitive transcranial magnetic stimulation in healthy young men. J ECT. 2006;22(1):49–53. https://doi.org/10.1097/00124509-200603000-00011.
Stultz DJ, Osburn S, Burns T, Pawlowska-Wajswol S, Walton R. Transcranial magnetic stimulation (TMS) safety with respect to seizures: a literature review. Neuropsychiatr Dis Treat. 2020;16:2989–3000. https://doi.org/10.2147/NDT.S276635.
Chattu VK, Manzar MD, Kumary S, Burman D, Spence DW, Pandi-Perumal SR. The global problem of insufficient sleep and its serious public health implications. Healthcare (Basel). 2018;7:1. https://doi.org/10.3390/healthcare7010001.
Lanza G. Repetitive TMS for the “cognitive tsunami” of sleep deprivation. Sleep Med. 2021;77:279–80. https://doi.org/10.1016/j.sleep.2020.11.010.
Romanella SM, Roe D, Paciorek R, Cappon D, Ruffini G, Menardi A, et al. Sleep, noninvasive brain stimulation, and the aging brain: challenges and opportunities. Aging Res Rev. 2020;61:101067. https://doi.org/10.1016/j.arr.2020.101067.
Beynel L, Davis SW, Crowell CA, Hilbig SA, Lim W, Nguyen D, et al. Online repetitive transcranial magnetic stimulation during working memory in younger and older adults: a randomized within-subject comparison. PLoS ONE. 2019;14(3):e0213707. https://doi.org/10.1371/journal.pone.0213707.
Funding
B. Luber, E. Ekpo, and S. H. Lisanby are supported by the NIMH Intramural Research Program (ZIAMH002955). S. H. Lisanby is inventor on patents and patent applications on electrical and magnetic brain stimulation therapy systems held by the NIH and Columbia University.
Author information
Authors and Affiliations
Contributions
B.L., E.E., and S.H.L. wrote the main manuscript text, and E.E. and B.L. prepared the table. All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Conflict of Interest
The authors have no competing interests as defined by Springer, or other interests that might be perceived to influence the results and/or discussion reported in this paper.
Human and Animal Rights and Informed Consent
All reported studies/experiments with human or animal subjects performed by the authors have been previously published and complied with all applicable ethical standards (including the Helsinki Declaration and its amendments, institutional/national research committee standards, and international/national/institutional guidelines).
Disclaimer
The opinions expressed in this article are the authors’ own and do not reflect the views of the NIH, the Department of Health and Human Services, or the United States government.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Luber, B., Ekpo, E.C. & Lisanby, S.H. The Use of Cognitive Paired Associative Stimulation (C-PAS) in Investigating and Remediating the Effects of Sleep Deprivation on Working Memory in Humans: The Importance of State-Dependency. Curr Sleep Medicine Rep (2024). https://doi.org/10.1007/s40675-024-00290-z
Accepted:
Published:
DOI: https://doi.org/10.1007/s40675-024-00290-z