Abstract
Purpose of review
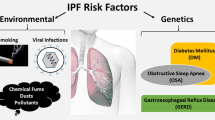
Systemic sclerosis–associated interstitial lung disease (SSc-ILD) and idiopathic pulmonary fibrosis (IPF) are fatal fibrotic lung disorders characterized by progressive fibrosis, immune dysregulation, vascular damage, fibroblast activation, and myofibroblast differentiation. In this review, we will briefly update all the above-mentioned mechanisms, cell-type involvement from single cell-RNA sequencing, and the differences with emerging common biomarkers and available treatment options.
Recent findings
In the IPF, tissue injury and lung fibrosis are thought to be initiated by injury of the alveolar epithelium and activation of alveolar epithelial cells (AECs) that release cytokines to activate the fibroblasts. By contrast, vascular damage is an early event in the pathogenesis of SSc-ILD and several diverse cells, such as myofibroblasts, fibroblasts, and endothelial cells, participate in inflammatory activation. Recent findings from single-cell RNA-seq suggested the presence of different subsets of innate and adaptive immune cells and differentiation of myofibroblasts from distinct sources, which complicates the understanding of the disease landscape. Fibroblast activation and myofibroblast accumulation are the final common pathways of lung fibrosis in both SSc-associated ILD and IPF.
Summary
Fibrosis in IPF appears to be related to aberrant repair following injury, but whether this also holds for SSc-ILD is less evident. Additionally, compared to IPF, immune dysregulation appears to contribute more to profibrotic responses in SSc-ILD. Nevertheless, persistent myofibroblast activity leads to progressive tissue fibrosis leading to organ failure and death. Few FDA-approved drugs (nintedanib, tocilizumab, and pirfenidone) are available for the treatment of fibrotic lung disease. Prospective high-throughput strategy-based approaches are required to understand the complexity of the diseases and develop specific therapeutic targets as part of precision medicine.

Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Herzog EL, Mathur A, Tager AM, Feghali-Bostwick C, Schneider F, Varga J. Review: Interstitial lung disease associated with systemic sclerosis and idiopathic pulmonary fibrosis: How similar and distinct? Arthritis Rheumatol. 2014;66(8):1967–78.
Mattoo H, Pillai S. Idiopathic pulmonary fibrosis and systemic sclerosis: pathogenic mechanisms and therapeutic interventions. Cell Mol Life Sci. 2021;78(14):5527–42.
Nihtyanova SI, Denton CP. Pathogenesis of systemic sclerosis associated interstitial lung disease. J Scleroderma Relat Disord. 2020;5(2_suppl):6–16.
Di Gregorio J, Robuffo I, Spalletta S, Giambuzzi G, De Iuliis V, Toniato E, et al. The epithelial-to-mesenchymal transition as a possible therapeutic target in fibrotic disorders. Front Cell Dev Biol. 2020;8:607483.
Kasper M, Barth K. Potential contribution of alveolar epithelial type I cells to pulmonary fibrosis. Biosci Rep. 2017;22:37(6).
Corvol H, Flamein F, Epaud R, Clement A, Guillot L. Lung alveolar epithelium and interstitial lung disease. Int J Biochem Cell Biol. 2009;41(8-9):1643–51.
Chen H, He A, Li H, Chen H, Xie H, Luo L, et al. TSSK4 upregulation in alveolar epithelial type-II cells facilitates pulmonary fibrosis through HSP90-AKT signaling restriction and AT-II apoptosis. Cell Death Dis. 2021;12(10):938.
•Valenzi E, Tabib T, Papazoglou A, Sembrat J, Trejo Bittar HE, Rojas M, et al. Disparate Interferon signaling and shared aberrant basaloid cells in single-cell profiling of idiopathic pulmonary fibrosis and systemic sclerosis-associated interstitial lung disease. Front Immunol. 2021;12:595811. An important study using single cell RNA sequencing technique for to generate comparative transcriptome profile of SSc-ILD and IPF lungs.
Depianto DJ, Vander HJA, Morshead KB, Sun KH, Modrusan Z, Teng G, et al. Molecular mapping of interstitial lung disease reveals a phenotypically distinct senescent basal epithelial cell population. 2021;6(8):e143626. https://doi.org/10.1172/jci.insight.143626.
Yamada Z, Nishio J, Motomura K, Mizutani S, Yamada S, Mikami T, et al. Senescence of alveolar epithelial cells impacts initiation and chronic phases of murine fibrosing interstitial lung disease. Front Immunol. 2022;18:13.
•Habermann AC, Gutierrez AJ, Bui LT, Yahn SL, Winters NI, Calvi CL, et al. Single-cell RNA sequencing reveals profibrotic roles of distinct epithelial and mesenchymal lineages in pulmonary fibrosis. Sci Adv. 2020;6(28):eaba1972. An important study identified novel ECM producing epithelial subset, which enriched in pulmonary fibrosis lung.
Shenderov K, Collins SL, Powell JD, Horton MR. Immune dysregulation as a driver of idiopathic pulmonary fibrosis. J Clin Invest. 2021;131(2):e143226.
•Fang D, Chen B, Lescoat A, Khanna D, Mu R. Immune cell dysregulation as a mediator of fibrosis in systemic sclerosis. Nat Rev Rheumatol. 2022;18(12):683–93. A relevant review described immune abnormalities are one of the major hallmarks of SSc.
Tourkina E, Bonner M, Oates J, Hofbauer A, Richard M, Znoyko S, et al. Altered monocyte and fibrocyte phenotype and function in scleroderma interstitial lung disease: Reversal by caveolin-1 scaffolding domain peptide. Fibrogenesis Tissue Repair. 2011;4(1):15.
Kreuter M, Lee JS, Tzouvelekis A, Oldham JM, Molyneaux PL, Weycker D, et al. Monocyte count as a prognostic biomarker in patients with idiopathic pulmonary fibrosis. Am J Respir Crit Care Med. 2021;204(1):74–81.
Mathai SK, Gulati M, Peng X, Russell TR, Shaw AC, Rubinowitz AN, et al. Circulating monocytes from systemic sclerosis patients with interstitial lung disease show an enhanced profibrotic phenotype. Lab Invest. 2010;90(6):812–23.
Trombetta AC, Soldano S, Contini P, Tomatis V, Ruaro B, Paolino S, et al. A circulating cell population showing both M1 and M2 monocyte/macrophage surface markers characterizes systemic sclerosis patients with lung involvement. Respir Res. 2018;19(1):186.
Rudnik M, Hukara A, Kocherova I, Jordan S, Schniering J, Milleret V, et al. Elevated fibronectin levels in profibrotic CD14+ monocytes and CD14+ macrophages in systemic sclerosis. Front Immunol. 2021;12:642891.
Yamashita M, Utsumi Y, Nagashima H, Nitanai H, Yamauchi K. S100A9/CD163 expression profiles in classical monocytes as biomarkers to discriminate idiopathic pulmonary fibrosis from idiopathic nonspecific interstitial pneumonia. Sci Rep. 2021;11(1):12135.
Scott MKD, Quinn K, Li Q, Carroll R, Warsinske H, Vallania F, et al. Increased monocyte count as a cellular biomarker for poor outcomes in fibrotic diseases: a retrospective, multicentre cohort study. Lancet Respir Med. 2019;7(6):497–508.
Bernardinello N, Grisostomi G, Cocconcelli E, Castelli G, Petrarulo S, Biondini D, et al. The clinical relevance of lymphocyte to monocyte ratio in patients with Idiopathic Pulmonary Fibrosis (IPF). Respir Med. 2022;191:106686.
Fraser E, Denney L, Antanaviciute A, Blirando K, Vuppusetty C, Zheng Y, et al. Multi-modal characterization of monocytes in idiopathic pulmonary fibrosis reveals a primed type I interferon immune phenotype. Front Immunol. 2021;12:623430.
Zhang L, Wang Y, Wu G, Xiong W, Gu W, Wang CY. Macrophages: friend or foe in idiopathic pulmonary fibrosis? Respir Res. 2018;19(1):170.
Manetti M. Deciphering the alternatively activated (M2) phenotype of macrophages in scleroderma. Exp Dermatol. 2015;24(8):576–8.
•Valenzi E, Bulik M, Tabib T, Morse C, Sembrat J, Trejo Bittar H, et al. Single-cell analysis reveals fibroblast heterogeneity and myofibroblasts in systemic sclerosis-associated interstitial lung disease. Ann Rheum Dis. 2019;78(10):1379–87. This study established fibroblast heterogeneity in SSc-ILD using single cell RNA technology.
Liossis SNC, Staveri C. The role of B cells in scleroderma lung disease pathogenesis. Front Med (Lausanne). 2022;9:936182.
Ali MF, Egan AM, Shaughnessy GF, Anderson DK, Kottom TJ, Dasari H, et al. Antifibrotics modify B-cell-induced fibroblast migration and activation in patients with idiopathic pulmonary fibrosis. Am J Respir Cell Mol Biol. 2021;64(6):722–33.
Truchetet ME, Brembilla NC, Montanari E, Allanore Y, Chizzolini C. Increased frequency of circulating Th22 in addition to Th17 and Th2 lymphocytes in systemic sclerosis: Association with interstitial lung disease. Arthritis Res Ther. 2011;13(5).
Bagnato G, Harari S. Cellular interactions in the pathogenesis of interstitial lung diseases. Eur Respir Rev. 2015;24(135):102–14.
Zhang M, Zhang S. T cells in fibrosis and fibrotic diseases. Front Immunol. 2020;11:1142.
Probst CK, Montesi SB, Medoff BD, Shea BS, Knipe RS. Vascular permeability in the fibrotic lung. Eur Resp J. 2020;56(1):1900100.
Ramadhiani R, Ikeda K, Hirata KI, Emoto N. Endothelial cell senescence exacerbates pulmonary fibrosis potentially through accelerated endothelial to mesenchymal transition. Kobe J Med Sci. 2021;67(3):E84–91.
Jia W, Wang Z, Gao C, Wu J, Wu Q. Trajectory modeling of endothelial-to-mesenchymal transition reveals galectin-3 as a mediator in pulmonary fibrosis. Cell Death Dis. 2021;12(4):327.
Pulito-Cueto V, Remuzgo-Martínez S, Genre F, Atienza-Mateo B, Mora-Cuesta VM, Iturbe-Fernández D, et al. Endothelial progenitor cells: Relevant players in the vasculopathy and lung fibrosis associated with the presence of interstitial lung disease in systemic sclerosis patients. Biomedicines. 2021;9(7):847.
Pulito-Cueto V, Remuzgo-Martínez S, Genre F, Mora-Cuesta VM, Iturbe-Fernández D, Fernández-Rozas S, et al. Endothelial progenitor cells as a potential biomarker in interstitial lung disease associated with rheumatoid arthritis. J Clin Med. 2020;9(12):4098.
Liu X, Qin X, Qin H, Jia C, Yuan Y, Sun T, et al. Characterization of the heterogeneity of endothelial cells in bleomycin-induced lung fibrosis using single-cell RNA sequencing. Angiogenesis. 2021;24(4):809–21.
Hung CF. Origin of myofibroblasts in lung fibrosis. Lung injury current tissue microenvironment reports. 2020;1:155–62. https://doi.org/10.1007/s43152-020-00022-9.
Hinz B, Phan SH, Thannickal VJ, Galli A, Bochaton-Piallat ML, Gabbiani G. The myofibroblast. Am J Pathol. 2007;170(6):1807–16.
Blaauboer ME, Boeijen FR, Emson CL, Turner SM, Zandieh-Doulabi B, Hanemaaijer R, et al. Extracellular matrix proteins: A positive feedback loop in lung fibrosis? Matrix Biology. Feb. 2014;34:170–8.
Fortier SM, Penke LR, King D, Pham TX, Ligresti G, Peters-Golden M. Myofibroblast dedifferentiation proceeds via distinct transcriptomic and phenotypic transitions. JCI Insight. 2021;6(6):e144799. https://doi.org/10.1172/jci.insight.144799.
Herrera J, Henke CA, Bitterman PB. Extracellular matrix as a driver of progressive fibrosis. J Clin Invest. 2018;128(1):45–53.
Jandl K, Kwapiszewska G. Stiffness of the extracellular matrix: A regulator of prostaglandins in pulmonary fibrosis? Am J Respir Cell Mol Biol. 2020;63(6):721–2.
Wu B, Tang L, Kapoor M. Fibroblasts and their responses to chronic injury in pulmonary fibrosis. Seminars in Arthritis and Rheumatism. W.B. Saunders; 2021 Feb;51(1):310-317.
Herrera J, Forster C, Pengo T, Montero A, Swift J, Schwartz MA, et al. Registration of the extracellular matrix components constituting the fibroblastic focus in idiopathic pulmonary fibrosis. JCI Insight. 2019;4(1):e125185.
Khedoe P, Marges E, Hiemstra P, Ninaber M, Geelhoed M. Interstitial lung disease in patients with systemic sclerosis: toward personalized-medicine-based prediction and drug screening models of Systemic Sclerosis-related Interstitial Lung Disease (SSc-ILD). Front Immunol. 2020;4:11.
Razdan N, Vasilopoulos T, Herbig U. Telomere dysfunction promotes transdifferentiation of human fibroblasts into myofibroblasts. Aging Cell. 2018;17(6):e12838.
Piñeiro-Hermida S, Martínez P, Bosso G, Flores JM, Saraswati S, Connor J, et al. Consequences of telomere dysfunction in fibroblasts, club and basal cells for lung fibrosis development. Nat Commun. 2022;13(1):5656.
Lakota K, Hanumanthu VS, Agrawal R, Carns M, Armanios M, Varga J. Short lymphocyte, but not granulocyte, telomere length in a subset of patients with systemic sclerosis. Ann Rheum Dis. 2019;78(8):1142–4.
Guo T, He C, Venado A, Zhou Y. Extracellular matrix stiffness in lung health and disease. Compr Physiol. 2022;12(3):3523–58.
Santos A, Lagares D. Matrix stiffness: the conductor of organ fibrosis. Curr Rheumatol Rep. 2018;20(1):2.
Nho RS, Ballinger MN, Rojas MM, Ghadiali SN, Horowitz JC. Biomechanical force and cellular stiffness in lung fibrosis. Am J Pathol. 2022;192(5):750–61.
Upagupta C, Shimbori C, Alsilmi R, Kolb M. Matrix abnormalities in pulmonary fibrosis. Eur Resp Rev. 2018;27(148):180033.
Lindahl GE, Stock CJW, Shi-Wen X, Leoni P, Sestini P, Howat SL, et al. Microarray profiling reveals suppressed interferon stimulated gene program in fibroblasts from scleroderma-associated interstitial lung disease. Respir Res. 2013;14(1):80.
Xie T, Wang Y, Deng N, Huang G, Taghavifar F, Geng Y, et al. Single-cell deconvolution of fibroblast heterogeneity in mouse pulmonary fibrosis. Cell Rep. 2018 Mar 27;22(13):3625–40.
••Travaglini KJ, Nabhan AN, Penland L, Sinha R, Gillich A, Sit RV, et al. A molecular cell atlas of the human lung from single-cell RNA sequencing. Nature. 2020;587(7835):619–25. An important study which created human lung atlas using single-cell RNA sequencing.
Tsukui T, Sun KH, Wetter JB, Wilson-Kanamori JR, Hazelwood LA, Henderson NC, et al. Collagen-producing lung cell atlas identifies multiple subsets with distinct localization and relevance to fibrosis. Nat Commun. 2020;11(1):1920. https://doi.org/10.1038/s41467-020-15647-5.
••Adams TS, Schupp JC, Poli S, Ayaub EA, Neumark N, Ahangari F, et al. Single-cell RNA-seq reveals ectopic and aberrant lung-resident cell populations in idiopathic pulmonary fibrosis. Sci Adv. 2020;6(28):eaba1983. Another important study using single cell RNA sequencing to generate single-cell atlas of the IPF lung.
Bonella F, Patuzzo G, Lunardi C. Biomarker discovery in systemic sclerosis: state of the art. Curr Biomark Find. 2015;5:47–68. https://doi.org/10.2147/CBF.S60446.
Thannickal VJ, Antony VB. Is personalized medicine a realistic goal in idiopathic pulmonary fibrosis? Exp Rev Resp Med. 2018;12(6):441–3.
Ebata S, Yoshizaki-Ogawa A, Sato S, Yoshizaki A. New era in systemic sclerosis treatment: recently approved therapeutics. J Clin Med. 2022;11(15):4631.
••Khanna D, Lescoat A, Roofeh D, Bernstein EJ, Kazerooni EA, Roth MD, et al. systemic sclerosis–associated interstitial lung disease: how to incorporate two food and drug administration–approved therapies in clinical practice. Arthritis and Rheumatol. 2022;74(1):13–27. A recent comprehensive review focused on the future pharmacologic and nonpharmacologic options for the treatment of SSc-ILD.
Kokosi MA, Margaritopoulos GA, Wells AU. Personalised medicine in interstitial lung diseases. Eur Resp Rev. 2018;30:27(148).
Martinez FJ, Collard HR, Pardo A, Raghu G, Richeldi L, Selman M, et al. Idiopathic pulmonary fibrosis. Nat Rev Dis Primers. 2017;3(1):17074.
Lederer DJ, Martinez FJ. Idiopathic Pulmonary Fibrosis. N Engl J Med. 2018;378(19):1811–23.
Seedat UF. Trial of a preferential phosphodiesterase 4B inhibitor for idiopathic pulmonary fibrosis. N Engl J Med. 386(23):2178–87.
Health NJ. Saracatinib in the Treatment of Idiopathic Pulmonary Fibrosis (STOP-IPF). 2020-2023:NCT04598919. https://classic.clinicaltrials.gov/ct2/show/NCT04598919.
Campochiaro C, Allanore Y. An update on targeted therapies in systemic sclerosis based on a systematic review from the last 3 years. Arthritis Res Ther. 2021 Dec 1;23(1):155.
Spierings J, Chiu YH, Voortman M, van Laar JM. Autologous stem-cell transplantation in systemic sclerosis-associated interstitial lung disease: early action in selected patients rather than escalation therapy for all. Ther Adv Musculoskelet Dis. 2021;13:1759720X2110351.
Cheng W, Zeng Y, Wang D. Stem cell-based therapy for pulmonary fibrosis. Stem Cell Res Ther. 2022;13(1):492.
Glass DS, Grossfeld D, Renna HA, Agarwala P, Spiegler P, DeLeon J, et al. Idiopathic pulmonary fibrosis: Current and future treatment. Clin Respir J. 2022 Feb 10;16(2):84–96.
Finnerty JP, Ponnuswamy A, Dutta P, Abdelaziz A, Kamil H. Efficacy of antifibrotic drugs, nintedanib and pirfenidone, in treatment of progressive pulmonary fibrosis in both idiopathic pulmonary fibrosis (IPF) and non-IPF: a systematic review and meta-analysis. BMC Pulm Med. 2021;21(1):411.
••Hinz B, Lagares D. Evasion of apoptosis by myofibroblasts: a hallmark of fibrotic diseases. Nat Rev Rheumatol. 2020;16(1):11–31. An important review described the mechanism of how myofibroblasts evade from apoptosis in the fibrotic microenvironment.
Bonhomme O, André B, Gester F, De Seny D, Moermans C, Struman I, et al. Biomarkers in systemic sclerosis-associated interstitial lung disease: Review of the literature. Rheumatology (Oxford). 2019;58(9):1534–46.
Drakopanagiotakis F, Wujak L, Wygrecka M, Markart P. Biomarkers in idiopathic pulmonary fibrosis. Matrix Biol. 2018;68-69:404–21.
Guiot J, Moermans C, Henket M, Corhay JL, Louis R. Blood biomarkers in idiopathic pulmonary fibrosis. Lung. 2017;195(3):273–80.
Ley B, Brown KK, Collard HR. Molecular biomarkers in idiopathic pulmonary fibrosis. Am J Physiol Lung Cell Mol Physiol. 2014;307(9):L681–91.
Elhai M, Avouac J, Allanore Y. Circulating lung biomarkers in idiopathic lung fibrosis and interstitial lung diseases associated with connective tissue diseases: Where do we stand? Semin Arthritis Rheum. 2020;50(3):480–91.
Ramírez-Aragón M, Hernández-Sánchez F, Rodríguez-Reyna TS, Buendía-Roldán I, Güitrón-Castillo G, Núñez-Alvarez CA, et al. The transcription factor scx is a potential serum biomarker of fibrotic diseases. Int J Mol Sci. 2020;21(14):1–20.
Lota HK, Renzoni EA. Circulating biomarkers of interstitial lung disease in systemic sclerosis. Int J Rheumatol. 2012;2012:121439.
Bagnato G, Roberts WN, Roman J, Gangemi S. A systematic review of overlapping microrna patterns in systemic sclerosis and idiopathic pulmonary fibrosis. Eur Respir Rev. 2017;26(144):160125.
Acknowledgements
We thank Kris Shah for editing.
Funding
This study was supported by grants from the National Institutes of Health, National Institute of Arthritis, and Musculoskeletal and Skin Diseases (NIAMS AR074997) and the National Scleroderma Foundation.
Author information
Authors and Affiliations
Contributions
PV and SB wrote the review; SBa and JV reviewed and edited.
Corresponding author
Ethics declarations
Conflict of Interest
Priyanka Verma declares that she has no conflict of interest. Swarna Bale declares that she has no conflict of interest. John Varga declares that he has no conflict of interest. Swati Bhattacharyya declares that she has no conflict of interest.
Human and animal rights and informed consent
The article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Verma, P., Bale, S., Varga, J. et al. Molecular Mechanisms Underlying Systemic Sclerosis–Associated Interstitial Lung Disease and Idiopathic Pulmonary Fibrosis: an Update. Curr Treat Options in Rheum 9, 221–235 (2023). https://doi.org/10.1007/s40674-023-00213-z
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40674-023-00213-z