Abstract
Background
End-stage kidney disease (ESKD) incidence has been increasing over time, contributing significantly to morbidity and mortality. However, there is limited data examining the psychosocial factors affecting people with ESKD and how the social worker fits within the multidisciplinary CKD care. This integrative systematic review aims to summarise the existing evidence on psychosocial determinants of outcomes in ESKD and the role of the social worker in nephrology care.
Method
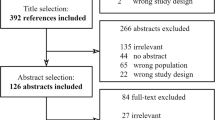
The literature search was conducted using PubMed and MEDLINE, targeting articles published from database inception until May 2021. This systematic review was performed in compliance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement. The Joanna Briggs Institute tools were employed to assess the quality of included studies.
Results
Of the 397 citations, 13 studies applicable to 1465 patients met the inclusion criteria. The studies were of cross-sectional, experimental, and exploratory qualitative design in nature. The findings of the studies were summarised into three major themes—psychosocial factors, role of the renal social worker, and impact of the renal social worker. The studies demonstrated that concerns related to adjustment, death and dying, family and social functioning, and loss were common amongst participants of the included studies indicating the need for a social worker. Three studies explored the impact of social workers in ESKD, revealing that people who received support from social workers had an improved quality of life, lower depression scores, and reduced hospitalisations and emergency room visits.
Conclusion
This review summarizes the multitude of physical and psychological stressors that patients with ESRD face, and highlights the positive role social workers can play in improving the psychosocial stressors in this patient group, and the need for large-scale randomised trials to understand the role of social workers as part of a multidisciplinary nephrology care.
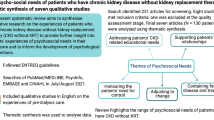
Graphic abstract


Similar content being viewed by others
References
Jha V, Garcia-Garcia G, Iseki K, Li Z, Naicker S, Plattner B, Saran R, Wang AY, Yang CW (2013) Chronic kidney disease: global dimension and perspectives. Lancet 382(9888):260–272. https://doi.org/10.1016/s0140-6736(13)60687-x
Bale C, Douglas A, Jegatheesan D, Pham L, Huynh S, Mulay A, Ranganathan D (2016) Psychosocial factors in end-stage kidney disease patients at a tertiary hospital in Australia. Int J Nephrol 2016. https://doi.org/10.1155/2016/2051586
Beder J (2000) Evaluation research on the effectiveness of social work intervention on dialysis patients: the first three months. Soc Work Health Care 30(1):15–30
Finnegan-John J, Thomas VJ (2013) The psychosocial experience of patients with end-stage renal disease and its impact on quality of life: findings from a needs assessment to shape a service. International Scholarly Research Notices 2013
Furr LA (1998) Psycho-social aspects of serious renal disease and dialysis: a review of the literature. Soc Work Health Care 27(3):97–118
Giles S (2005) Struggles between the body and machine: the paradox of living with a home haemodialysis machine. Soc Work Health Care 41(2):19–35
Jankowska-Polańska B, Uchmanowicz I, Wysocka A, Uchmanowicz B, Lomper K, Fal AM (2017) Factors affecting the quality of life of chronic dialysis patients. Eur J Pub Health 27(2):262–267
Low J, Smith G, Burns A, Jones L (2008) The impact of end-stage kidney disease (ESKD) on close persons: a literature review. Oxford University Press
Sheridan MS (1977) Renal disease and the social worker: a review. Health Soc Work 2(2):122–157
Taylor F, Taylor C, Baharani J, Nicholas J, Combes G (2016) Integrating emotional and psychological support into the end-stage renal disease pathway: a protocol for mixed methods research to identify patients’ lower-level support needs and how these can most effectively be addressed. BMC Nephrol 17(1):111
Van Der Borg WE, Schipper K, Abma TA (2016) Protocol of a mixed method, randomized controlled study to assess the efficacy of a psychosocial intervention to reduce fatigue in patients with End-Stage Renal Disease (ESRD). BMC Nephrol 17(1):73
Carlson LE, Bultz BD (2003) Benefits of psychosocial oncology care: Improved quality of life and medical cost offset. Health Qual Life Outcomes 1(1):8
Reiss M, Sandborn WJ (2015) The role of psychosocial care in adapting to health care reform. Clin Gastroenterol Hepatol 13(13):2219–2224
Abdel-Kader K, Unruh ML, Weisbord SD (2009) Symptom burden, depression, and quality of life in chronic and end-stage kidney disease. Clin J Am Soc Nephrol 4(6):1057–1064
Beder J (2008) Evaluation research on social work interventions: a study on the impact of social worker staffing. Soc Work Health Care 47(1):1–13
Callahan MB (2007) Begin with the end in mind: the value of outcome-driven nephrology social work. Adv Chronic Kidney Dis 14(4):409–414
Dobrof J, Dolinko A, Lichtiger E, Uribarri J, Epstein I (2002) Dialysis patient characteristics and outcomes: the complexity of social work practice with the end stage renal disease population. Soc Work Health Care 33(3–4):105–128
Callahan MB (2011) The role of the nephrology social worker in optimizing treatment outcomes for end-stage renal disease patients. Dial Transplant 40(10):444–450
Moher D, Liberati A, Tetzlaff J, Altman DG (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Ann Intern Med 151(4):264–269
Whittemore R, Knafl K (2005) The integrative review: updated methodology. J Adv Nurs 52(5):546–553
Fineout-Overholt E, Melnyk BM, Stillwell SB, Williamson KM (2010) Evidence-based practice, step by step: critical appraisal of the evidence part III. AJN The Am J Nur 110(11):43–51
Lockwood C, Munn Z, Porritt K (2015) Qualitative research synthesis: methodological guidance for systematic reviewers utilizing meta-aggregation. Int J Evid Based Healthc 13(3):179–187
Tufanaru C, Munn Z, Aromataris E, Campbell J, Hopp L (2017) Chapter 3: systematic reviews of effectiveness. Joanna Briggs Institute Reviewer’s Manual The Joanna Briggs Institute
Moola S, Munn Z, Tufanaru C, Aromataris E, Sears K, Sfetcu R, Currie M, Qureshi R, Mattis P, Lisy K (2017) Chapter 7: systematic reviews of etiology and risk. Joanna Briggs Institute Reviewer’s Manual The Joanna Briggs Institute (2019–2005)
Frank A, Auslander GK, Weissgarten J (2004) Quality of life of patients with end-stage renal disease at various stages of the illness. Soc Work Health Care 38(2):1–27
Karolich RL, Ford JP (2010) Meaning, comprehension, and manageability of end-stage renal disease in older adults living with long-term hemodialysis. Soc Work Health Care 49(1):19–37
Tijerina MS (2006) Psychosocial factors influencing Mexican-American women’s adherence with hemodialysis treatment. Soc Work Health Care 43(1):57–74
Tijerina MS (2009) Mexican American women’s adherence to hemodialysis treatment: a social constructivist perspective. Soc Work 54(3):232–242
Giles S (2004) Transformations: a phenomenological investigation into the life-world of home haemodialysis. Soc Work Health Care 38(2):29–50
Alleyne SI, Vassall-Hurd SA, Morgan AG (1982) End-stage renal disease in Jamaica: how patients cope in a developing society. Health Soc Work 7(2):130–133
Raiz L, Davies EA, Ferguson RM (2003) Sexual functioning following renal transplantation. Health Soc Work 28(4):264–272
Raiz L, Monroe J (2007) Employment post-transplant: a biopsychosocial analysis. Soc Work Health Care 45(3):19–37
Reid WJ, Hanrahan P (1982) Recent evaluations of social work: grounds for optimism. Soc Work 27(4):328–340
Winterbottom A, Bekker HL, Conner M, Mooney A (2014) Choosing dialysis modality: decision making in a chronic illness context. Health Expect 17(5):710–723
Di Wei X-YL, Chen Y-Y, Zhou X, Hu H-P (2016) Effectiveness of physical, psychological, social, and spiritual intervention in breast cancer survivors: an integrative review. Asia-Pacific J Oncol Nurs 3(3):226
Lilliehorn S, Isaksson J, Salander P (2019) What does an oncology social worker deal with in patient consultations?—an empirical study. Soc Work Health Care 58(5):494–508
Zilberfein F, Hutson C, Snyder S, Epstein I (2002) Social work practice with pre-and post-liver transplant patients: a retrospective self study. Soc Work Health Care 33(3–4):91–104
Pockett R, Dzidowska M, Hobbs K (2015) Social work intervention research with adult cancer patients: a literature review and reflection on knowledge-building for practice. Soc Work Health Care 54(7):582–614
Pockett R, Peate M, Hobbs K, Dzidowska M, Bell ML, Baylock B, Epstein I (2016) The characteristics of oncology social work in Australia: implications for workforce planning in integrated cancer care. Asia-Pacific J Clin Oncol 12(4):444–452
Klang B, Björvell H, Berglund J, Sundstedt C, Clyne N (1998) Predialysis patient education: effects on functioning and well-being in uraemic patients. J Adv Nurs 28(1):36–44
Sesso R, Yoshihiro M (1997) Time of diagnosis of chronic renal failure and assessment of quality of life in haemodialysis patients. Nephrol, Dial, Transplant: Offl Publ Eur Dial Transplant Assoc-Eur Ren Assoc 12(10):2111–2116
Germain MJ, Cohen L (2001) Supportive care for patients with renal disease: time for action. Am J Kidney Dis 38(4):884–886
Davison SN, Jassal SV (2016) Supportive care: integration of patient-centered kidney care to manage symptoms and geriatric syndromes. Clin J Am Soc Nephrol 11(10):1882–1891
O’Halloran P, Noble H, Norwood K, Maxwell P, Shields J, Fogarty D, Murtagh F, Morton R, Brazil K (2018) Advance care planning with patients who have end-stage kidney disease: a systematic realist review. J Pain Symptom Manag 56(5):795–807 (e718)
Murtagh FE, Burns A, Moranne O, Morton RL, Naicker S (2016) Supportive care: comprehensive conservative care in end-stage kidney disease. Clin J Am Soc Nephrol 11(10):1909–1914
Cukor D, Cohen SD, Peterson RA, Kimmel PL (2007) Psychosocial aspects of chronic disease: ESRD as a paradigmatic illness. J Am Soc Nephrol 18(12):3042–3055
Funding
The authors declare that they have no relevant financial interest.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
This type of study does not require ethical approval.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Appendix A: Appraisal of selected studies
Appendix A: Appraisal of selected studies
JBI critical appraisal checklist for analytical cross-sectional studies (Moola et al.) [24]
Criteria
-
1.
Were the criteria for inclusion in the sample clearly defined?
-
2.
Were the study subjects and the setting described in detail?
-
3.
Was the exposure measured in a valid and reliable way?
-
4.
Were objective, standard criteria used for measurement of the condition?
-
5.
Were confounding factors identified?
-
6.
Were strategies to deal with confounding factors stated?
-
7.
Were the outcomes measured in a valid and reliable way?
-
8.
Was appropriate statistical analysis used?
Authors, year | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | Overall |
|---|---|---|---|---|---|---|---|---|---|
Alleyne et al. [30] | N | Y | N | Y | N | N | N | N | Low |
Bale et al. [2] | Y | Y | Y | Y | N | N | Y | Y | Average |
Doborf et al. [17] | Y | Y | Y | Y | N | N | Y | Y | Average |
Frank et al. [25] | Y | Y | N | Y | N | N | Y | Y | Average |
Karolich et al. [26] | Y | Y | N | Y | Y | N | Y | Y | Average |
Raiz et al. [31] | N | N | N | Y | Y | N | N | N | Low |
Raiz et al. [32] | N | N | N | Y | N | N | N | Y | Low |
Tijerina et al. [27] | Y | Y | N | Y | N | N | Y | Y | Average |
Tijerina et al. [28] | Y | Y | N | Y | N | N | Y | Y | Average |
JBI critical appraisal checklist for randomized controlled trials (Tufanaru et al.) [23]
Criteria
-
1.
Was true randomization used for assignment of participants to treatment groups?
-
2.
Was allocation to treatment groups concealed?
-
3.
Were treatment groups similar at the baseline?
-
4.
Were participants blind to treatment assignment?
-
5.
Were those delivering treatment blind to treatment assignment?
-
6.
Were outcomes assessors blind to treatment assignment?
-
7.
Were treatment groups treated identically other than the intervention of interest?
-
8.
Was follow up complete and if not, were differences between groups in terms of their follow up adequately described and analyzed?
-
9.
Were participants analyzed in the groups to which they were randomized?
-
10.
Were outcomes measured in the same way for treatment groups?
-
11.
Were outcomes measured in a reliable way?
-
12.
Was appropriate statistical analysis used?
-
13.
Was the trial design appropriate, and any deviations from the standard RCT design (individual randomization, parallel groups) accounted for in the conduct and analysis of the trial?
JBI critical appraisal checklist for qualitative research (Lockwood et al.) [22]
Criteria
-
1.
Is there congruity between the stated philosophical perspective and the research methodology?
-
2.
Is there congruity between the research methodology and the research question or objectives?
-
3.
Is there congruity between the research methodology and the methods used to collect data?
-
4.
Is there congruity between the research methodology and the representation and analysis of data?
-
5.
Is there congruity between the research methodology and the interpretation of results?
-
6.
Is there a statement locating the researcher culturally or theoretically?
-
7.
Is the influence of the researcher on the research, and vice- versa, addressed?
-
8.
Are participants, and their voices, adequately represented?
-
9.
Is the research ethical according to current criteria or, for recent studies, and is there evidence of ethical approval by an appropriate body?
-
10.
Do the conclusions drawn in the research report flow from the analysis, or interpretation, of the data?
Rights and permissions
About this article
Cite this article
Hansen, M.S., Tesfaye, W., Sewlal, B. et al. Psychosocial factors affecting patients with end-stage kidney disease and the impact of the social worker. J Nephrol 35, 43–58 (2022). https://doi.org/10.1007/s40620-021-01098-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40620-021-01098-8