Abstract
Purpose
Gender-affirming hormone treatment (GAHT) is one of the main demands of transgender and gender diverse (TGD) people, who are usually categorised as transgender assigned-male-at birth (AMAB) and assigned-female-at birth (AFAB). The aim of the study is to investigate the long-term therapeutic management of GAHT, considering hormonal targets, treatment adjustments and GAHT safety.
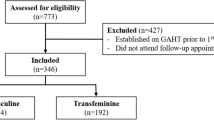
Methods
A retrospective, longitudinal, observational, multicentre clinical study was carried out. Transgender people, both AMAB and AFAB, were recruited from two Endocrinology Units in Italy (Turin and Modena) between 2005 and 2022. Each subject was managed with specific and personalized follow-up depending on the clinical practice of the Centre. All clinical data routinely collected were extracted, including anthropometric and biochemical parameters, lifestyle habits, GAHT regime, and cardiovascular events.
Results
Three-hundred and two transgender AFAB and 453 transgender AMAB were included. Similar follow-up duration (p = 0.974) and visits’ number (p = 0.384) were detected between groups. The transgender AFAB group reached therapeutic goals in less time (p = 0.002), fewer visits (p = 0.006) and fewer adjustments of GAHT scheme (p = 0.024). Accordingly, transgender AFAB showed a higher adherence to medical prescriptions compared to transgender AMAB people (p < 0.001). No significantly increased rate of cardiovascular events was detected in both groups.
Conclusion
Our real-world clinical study shows that transgender AFAB achieve hormone target earlier and more frequently in comparison to transgender AMAB individuals. Therefore, transgender AMAB people may require more frequent check-ups in order to tailor feminizing GAHT and increase therapeutic adherence.
Similar content being viewed by others
Data availability
Data are available after request directly to the author.
References
Fisher AD et al (2022) SIGIS-SIAMS-SIE position statement of gender affirming hormonal treatment in transgender and non-binary people, (in eng). J Endocrinol Invest 45(3):657–673. https://doi.org/10.1007/s40618-021-01694-2
Meyer-Bahlburg HF (2010) From mental disorder to iatrogenic hypogonadism: dilemmas in conceptualizing gender identity variants as psychiatric conditions, (in eng). Arch Sex Behav 39(2):461–476. https://doi.org/10.1007/s10508-009-9532-4
Coleman E et al (2022) Standards of care for the health of transgender and gender diverse people, version 8, (in eng). Int J Transgend Health 23(Suppl 1):S1-s259. https://doi.org/10.1080/26895269.2022.2100644
Goodman M, Adams N, Corneil T, Kreukels B, Motmans J, Coleman E (2019) Size and distribution of transgender and gender nonconforming populations: a narrative review, (in eng). Endocrinol Metab Clin North Am 48(2):303–321. https://doi.org/10.1016/j.ecl.2019.01.001
Winter S et al (2016) Transgender people: health at the margins of society, (in eng). Lancet (London, England) 388(10042):390–400. https://doi.org/10.1016/s0140-6736(16)00683-8
Wylie K, Knudson G, Khan SI, Bonierbale M, Watanyusakul S, Baral S (2016) Serving transgender people: clinical care considerations and service delivery models in transgender health, (in eng). Lancet (London, England) 388(10042):401–411. https://doi.org/10.1016/s0140-6736(16)00682-6
Expósito-Campos P, Gómez-Balaguer M, Hurtado-Murillo F, Morillas-Ariño C (2023) Evolution and trends in referrals to a specialist gender identity unit in Spain over 10 years (2012–2021), (in eng). J Sex Med 20(3):377–387. https://doi.org/10.1093/jsxmed/qdac034
Hembree WC et al (2017) Endocrine treatment of gender-dysphoric/gender-incongruent persons: an endocrine society clinical practice guideline, (in eng). Endocr Pract Off J Am Coll Endocrinol Am Assoc Clini Endocrinol 23(12):1437. https://doi.org/10.4158/1934-2403-23.12.1437
Cocchetti C, Ristori J, Romani A, Maggi M, Fisher AD (2020) Hormonal treatment strategies tailored to non-binary transgender individuals, (in eng). J Clin Med 9:6. https://doi.org/10.3390/jcm9061609
van Kesteren PJ, Asscheman H, Megens JA, Gooren LJ (1997) Mortality and morbidity in transsexual subjects treated with cross-sex hormones, (in eng). Clin Endocrinol 47(3):337–342. https://doi.org/10.1046/j.1365-2265.1997.2601068.x
Meyer G, Mayer M, Mondorf A, Flügel AK, Herrmann E, Bojunga J (2020) Safety and rapid efficacy of guideline-based gender-affirming hormone therapy: an analysis of 388 individuals diagnosed with gender dysphoria, (in eng). Eur J Endocrinol Eur Fed Endocr Soc 182(2):149–156. https://doi.org/10.1530/eje-19-0463
de Ronde W, ten Kulve J, Woerdeman J, Kaufman JM, de Jong FH (2009) Effects of oestradiol on gonadotrophin levels in normal and castrated men, (in eng). Clin Endocrinol 71(6):874–879. https://doi.org/10.1111/j.1365-2265.2009.03573.x
Mueller A, Kiesewetter F, Binder H, Beckmann MW, Dittrich R (2007) Long-term administration of testosterone undecanoate every 3 months for testosterone supplementation in female-to-male transsexuals, (in eng). J Clin Endocrinol Metab 92(9):3470–3475. https://doi.org/10.1210/jc.2007-0746
Irwig MS (2018) Cardiovascular health in transgender people, (in eng). Rev Endocr Metab Disord 19(3):243–251. https://doi.org/10.1007/s11154-018-9454-3
Maraka S et al (2017) Sex steroids and cardiovascular outcomes in transgender individuals: a systematic review and meta-analysis, (in eng). J Clin Endocrinol Metab 102(11):3914–3923. https://doi.org/10.1210/jc.2017-01643
Alzahrani T et al (2019) Cardiovascular disease risk factors and myocardial infarction in the transgender population, (in eng). Circ Cardiovasc Qual Outcomes 12(4):e005597. https://doi.org/10.1161/circoutcomes.119.005597
Kyinn M, Banks K, Leemaqz SY, Sarkodie E, Goldstein D, Irwig MS (2021) Weight gain and obesity rates in transgender and gender-diverse adults before and during hormone therapy, (in eng). Int J Obes (Lond) 45(12):2562–2569. https://doi.org/10.1038/s41366-021-00935-x
MacKnight C, Rockwood K (2001) Use of the chronic disease score to measure comorbidity in the Canadian study of health and aging, (in eng). Int Psychogeriatr 13(Supp 1):137–142. https://doi.org/10.1017/s1041610202008074
McGregor JC et al (2005) Utility of the chronic disease score and Charlson comorbidity index as comorbidity measures for use in epidemiologic studies of antibiotic-resistant organisms, (in eng). Am J Epidemiol 161(5):483–493. https://doi.org/10.1093/aje/kwi068
Von Korff M, Wagner EH, Saunders K (1992) A chronic disease score from automated pharmacy data, (in eng). J Clin Epidemiol 45(2):197–203. https://doi.org/10.1016/0895-4356(92)90016-g
Romeo M, Spaggiari G, Nuzzo F, Granata ARM, Simoni M, Santi D (2022) Follicle-stimulating hormone effectiveness in male idiopathic infertility: what happens in daily practice? (in eng). Andrology. https://doi.org/10.1111/andr.13353
Zhang PY, Yu Y (2019) Precise personalized medicine in gynecology cancer and infertility, (in eng). Front Cell Dev Biol 7:382. https://doi.org/10.3389/fcell.2019.00382
Broekmans FJ (2019) Individualization of FSH doses in assisted reproduction: facts and fiction, (in eng). Front Endocrinol 10:181. https://doi.org/10.3389/fendo.2019.00181
Rosenthal SM (2014) Approach to the patient: transgender youth: endocrine considerations, (in eng). J Clin Endocrinol Metab 99(12):4379–4389. https://doi.org/10.1210/jc.2014-1919
Gooren L (2005) Hormone treatment of the adult transsexual patient, (in eng). Horm Res 64(Suppl 2):31–36. https://doi.org/10.1159/000087751
Moore E, Wisniewski A, Dobs A (2003) Endocrine treatment of transsexual people: a review of treatment regimens, outcomes, and adverse effects, (in eng). J Clin Endocrinol Metab 88(8):3467–3473. https://doi.org/10.1210/jc.2002-021967
Gooren LJ, Giltay EJ, Bunck MC (2008) Long-term treatment of transsexuals with cross-sex hormones: extensive personal experience, (in eng). J Clin Endocrinol Metab 93(1):19–25. https://doi.org/10.1210/jc.2007-1809
Prior JC, Vigna YM, Watson D (1989) Spironolactone with physiological female steroids for presurgical therapy of male-to-female transsexualism, (in eng). Arch Sex Behav 18(1):49–57. https://doi.org/10.1007/bf01579291
Tangpricha V, Ducharme SH, Barber TW, Chipkin SR (2003) Endocrinologic treatment of gender identity disorders, (in eng). Endocr Pract Off J Am Coll Endocrinol Am Assoc Clini Endocrinol 9(1):12–21. https://doi.org/10.4158/ep.9.1.12
Jones BA, Haycraft E, Murjan S, Arcelus J (2016) Body dissatisfaction and disordered eating in trans people: a systematic review of the literature, (in eng). Int Rev Psychiatry 28(1):81–94. https://doi.org/10.3109/09540261.2015.1089217
Gómez-Gil E, Trilla A, Salamero M, Godás T, Valdés M (2009) Sociodemographic, clinical, and psychiatric characteristics of transsexuals from Spain, (in eng). Arch Sex Behav 38(3):378–392. https://doi.org/10.1007/s10508-007-9307-8
Fisher AD et al (2013) Sociodemographic and clinical features of gender identity disorder: an Italian multicentric evaluation, (in eng). J Sex Med 10(2):408–419. https://doi.org/10.1111/j.1743-6109.2012.03006.x
Santi D et al (2022) Qualitative and quantitative analysis of doctor-patient interactions during andrological consultations, (in eng). Andrology 10(7):1240–1249. https://doi.org/10.1111/andr.13225
Cocchetti C et al (2021) Does gender-affirming hormonal treatment affect 30-year cardiovascular risk in transgender persons? A two-year prospective European study (ENIGI), (in eng). J Sex Med 18(4):821–829. https://doi.org/10.1016/j.jsxm.2021.01.185
Quirós C et al (2015) Effect of cross-sex hormone treatment on cardiovascular risk factors in transsexual individuals. Experience in a specialized unit in Catalonia, (in eng). Endocrinologia Y Nutricion Organo De La Sociedad Espanola De Endocrinologia Y Nutricion 62(5):210–216. https://doi.org/10.1016/j.endonu.2015.02.001
Hilden M et al (2021) Gender incongruence in Denmark, a quantitative assessment, (in eng). Acta Obstet Gynecol Scand 100(10):1800–1805. https://doi.org/10.1111/aogs.14227
Bhasin S, Basaria S (2011) Diagnosis and treatment of hypogonadism in men, (in eng), best practice & research. Clin Endocrinol Metab 25(2):251–270. https://doi.org/10.1016/j.beem.2010.12.002
Bhasin S et al (2018) Testosterone therapy in men with hypogonadism: an endocrine society* clinical practice guideline. J Clin Endocrinol Metab 103(5):1715–1744. https://doi.org/10.1210/jc.2018-00229
Anderson GL et al (2004) Effects of conjugated equine estrogen in postmenopausal women with hysterectomy: the Women’s Health Initiative randomized controlled trial, (in eng). JAMA 291(14):1701–1712. https://doi.org/10.1001/jama.291.14.1701
Voutsadaki K, Matalliotakis M, Ladomenou F (2022) Hypogonadism in adolescent girls: treatment and long-term effects, (in eng). Acta Biomed 93(5):e2022317. https://doi.org/10.23750/abm.v93i5.13719
Boehm U et al (2015) Expert consensus document: European consensus statement on congenital hypogonadotropic hypogonadism–pathogenesis, diagnosis and treatment, (in eng). Nat Rev Endocrinol 11(9):547–564. https://doi.org/10.1038/nrendo.2015.112
Holm M et al (2019) Pattern of mortality after menopausal hormone therapy: long-term follow up in a population-based cohort, (in eng). BJOG An Int J Obstet Gynaecol 126(1):55–63. https://doi.org/10.1111/1471-0528.15433
Bhupathiraju SN et al (2017) Hormone therapy use and risk of chronic disease in the nurses’ health study: a comparative analysis with the women’s health initiative, (in eng). Am J Epidemiol 186(6):696–708. https://doi.org/10.1093/aje/kwx131
Martinez-Martin FJ et al (2022) Incidence of hypertension in young transgender people after a 5-year follow-up: association with gender-affirming hormonal therapy, (in eng). Hypertens Res. https://doi.org/10.1038/s41440-022-01067-z
Elamin MB, Garcia MZ, Murad MH, Erwin PJ, Montori VM (2010) Effect of sex steroid use on cardiovascular risk in transsexual individuals: a systematic review and meta-analyses, (in eng). Clin Endocrinol 72(1):1–10. https://doi.org/10.1111/j.1365-2265.2009.03632.x
Nota NM, Wiepjes CM, de Blok CJM, Gooren LJG, Kreukels BPC, den Heijer M (2019) Occurrence of acute cardiovascular events in transgender individuals receiving hormone therapy, (in eng). Circulation 139(11):1461–1462. https://doi.org/10.1161/circulationaha.118.038584
Aranda G et al (2021) Cardiovascular risk associated with gender affirming hormone therapy in transgender population, (in eng). Front Endocrinol 12:718200. https://doi.org/10.3389/fendo.2021.718200
Berra M et al (2006) Testosterone decreases adiponectin levels in female to male transsexuals, (in eng). Asian J Androl 8(6):725–729. https://doi.org/10.1111/j.1745-7262.2006.00204.x
Wierckx K et al (2014) Cross-sex hormone therapy in trans persons is safe and effective at short-time follow-up: results from the European network for the investigation of gender incongruence, (in eng). J Sex Med 11(8):1999–2011. https://doi.org/10.1111/jsm.12571
Pirtea P, Ayoubi JM, Desmedt S, T’Sjoen G (2021) Ovarian, breast, and metabolic changes induced by androgen treatment in transgender men, (in eng). Fertil Steril 116(4):936–942. https://doi.org/10.1016/j.fertnstert.2021.07.1206
Acknowledgements
Nothing to declare.
Funding
This research did not receive any specific grant from any funding agency in the public, commercial or not-for-profit sector.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
There is no conflict of interest that could be perceived as prejudicing the impartiality of the research reported.
Ethical approval
The study protocol was approved by the Ethics Committee of “Area Vasta Emilia Nord” (protocol number: AOU0024637/19 of 12/09/2019).
Informed consent
The informed consent has been provided by patients enrolled.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Santi, D., Spaggiari, G., Marinelli, L. et al. Gender-affirming hormone treatment: friend or foe? Long-term follow-up of 755 transgender people. J Endocrinol Invest 47, 1091–1100 (2024). https://doi.org/10.1007/s40618-023-02220-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40618-023-02220-2