Abstract
Background
Serum lipid levels are associated with cancer risk. However, there still have uncertainties about the single and combined effects of low lipid levels on cancer risk.
Methods
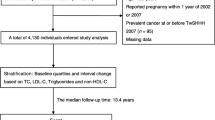
A prospective cohort study of 33,773 adults in Shanghai between 2016 and 2017 was conducted. Total cholesterol (TC), triglycerides (TG), low-density lipoprotein cholesterol (LDL-C), and high-density lipoprotein cholesterol (HDL-C) levels were measured. Cox proportional hazard models were used to assess the association of single and combined lipids with overall, lung, colon, rectal, thyroid gland, stomach, and female breast cancers. The effect of the combination of abnormal lipid score and lifestyle on cancer was also estimated.
Results
A total of 926 incident cancer cases were identified. In the RCS analysis, hazard ratios (HRs) of overall cancer for individuals with TC < 5.18 mmol/L or with LDL-C < 3.40 mmol/L were higher. Low TC was associated with higher colorectal cancer risk (HR [95% CI] = 1.76 [1.09–2.84]) and low HDL-C increased thyroid cancer risk by 90%. Abnormal lipid score was linearly and positively associated with cancer risk, and smokers with high abnormal lipid scores had a higher cancer risk, compared to non-smokers with low abnormal lipid scores (P < 0.05).
Conclusions
Low TC levels were associated with an increased risk of overall and colorectal cancer. More attention should be paid to participants with high abnormal lipid scores and unhealthy lifestyles who may have a higher risk of developing cancer. Determining the specific and comprehensive lipid combinations that affect tumorigenesis remains a valuable challenge.



Similar content being viewed by others
Data availability
Data for this study are available upon request, which clearly state the title and aim of the research.
References
Ferlay J, Colombet M, Soerjomataram I et al (2021) Cancer statistics for the year 2020: an overview. Int J Cancer 149:778–789. https://doi.org/10.1002/ijc.33588
Cao W, Chen H-D, Yu Y-W et al (2021) Changing profiles of cancer burden worldwide and in China: a secondary analysis of the global cancer statistics 2020. Chin Med J (Engl) 134:783–791. https://doi.org/10.1097/CM9.0000000000001474
Zheng R, Zhang S, Zeng H et al (2022) Cancer incidence and mortality in China, 2016. J Natl Cancer Center 2:1–9. https://doi.org/10.1016/j.jncc.2022.02.002
Sun D, Li H, Cao M et al (2020) Cancer burden in China: trends, risk factors and prevention. Cancer Biol Med 17:879–895. https://doi.org/10.20892/j.issn.2095-3941.2020.0387
Katzke VA, Sookthai D, Johnson T et al (2017) Blood lipids and lipoproteins in relation to incidence and mortality risks for CVD and cancer in the prospective EPIC–Heidelberg cohort. BMC Med 15:218. https://doi.org/10.1186/s12916-017-0976-4
Luo X, Cheng C, Tan Z et al (2017) Emerging roles of lipid metabolism in cancer metastasis. Mol Cancer 16:76. https://doi.org/10.1186/s12943-017-0646-3
Kuzu OF, Noory MA, Robertson GP (2016) The role of cholesterol in cancer. Cancer Res 76:2063–2070. https://doi.org/10.1158/0008-5472.CAN-15-2613
Bian X, Liu R, Meng Y et al (2021) Lipid metabolism and cancer. J Exp Med. https://doi.org/10.1084/jem.20201606
Butler LM, Perone Y, Dehairs J et al (2020) Lipids and cancer: emerging roles in pathogenesis, diagnosis and therapeutic intervention. Adv Drug Deliv Rev 159:245–293. https://doi.org/10.1016/j.addr.2020.07.013
Kitahara CM, Berrington de González A, Freedman ND et al (2011) Total cholesterol and cancer risk in a large prospective study in Korea. J Clin Oncol 29:1592–1598. https://doi.org/10.1200/JCO.2010.31.5200
Strohmaier S, Edlinger M, Manjer J et al (2013) Total serum cholesterol and cancer incidence in the metabolic syndrome and cancer project (Me-Can). PLoS ONE 8:e54242. https://doi.org/10.1371/journal.pone.0054242
Wu B, Teng L, He D et al (2019) Dose-response relation between serum total cholesterol levels and overall cancer risk: evidence from 12 prospective studies involving 1,926,275 participants. Int J Food Sci Nutr 70:432–441. https://doi.org/10.1080/09637486.2018.1529147
Kucharska-Newton AM, Rosamond WD, Mink PJ et al (2008) HDL-cholesterol and incidence of breast cancer in the ARIC cohort study. Ann Epidemiol 18:671–677. https://doi.org/10.1016/j.annepidem.2008.06.006
Furberg A-S, Veierød MB, Wilsgaard T et al (2004) Serum high density lipoprotein cholesterol, metabolic profile, and breast cancer risk. J Natl Cancer Inst 96:1152–1160. https://doi.org/10.1093/jnci/djh216
Beeghly-Fadiel A, Khankari NK, Delahanty RJ et al (2020) A Mendelian randomization analysis of circulating lipid traits and breast cancer risk. Int J Epidemiol 49:1117–1131. https://doi.org/10.1093/ije/dyz242
Ioannidou A, Watts EL, Perez-Cornago A et al (2022) The relationship between lipoprotein A and other lipids with prostate cancer risk: a multivariable Mendelian randomisation study. PLoS Med 19:e1003859. https://doi.org/10.1371/journal.pmed.1003859
Bull CJ, Bonilla C, Holly JMP et al (2016) Blood lipids and prostate cancer: a Mendelian randomization analysis. Cancer Med 5:1125–1136. https://doi.org/10.1002/cam4.695
Heir T, Falk RS, Robsahm TE et al (2016) Cholesterol and prostate cancer risk: a long-term prospective cohort study. BMC Cancer 16:643. https://doi.org/10.1186/s12885-016-2691-5
Zhao Q, Chen B, Wang R et al (2020) Cohort profile: protocol and baseline survey for the Shanghai Suburban Adult Cohort and Biobank (SSACB) study. BMJ Open 10:e035430. https://doi.org/10.1136/bmjopen-2019-035430
Zhu J, Zhang Y, Wu Y et al (2022) Obesity and dyslipidemia in Chinese adults: a cross-sectional study in Shanghai. China Nutr 14:2321. https://doi.org/10.3390/nu14112321
Tang M-H, Cui S-H, Yi K-Q et al (2022) Cross-sectional study on comorbidities in community patients with stroke in Songjiang District, Shanghai. Shanghai J Prev Med 34:888–894. https://doi.org/10.19428/j.cnki.sjpm.2022.21999
Pei J-F, Wang N, Zhao Q et al (2022) Association of physical activities in adults with diagnosis of type 2 diabetes in Songjiang District, Shanghai. Fudan Univ J Med Sci 49:852–861
Ren Z, Li Y, Li X et al (2021) Associations of body mass index, waist circumference and waist-to-height ratio with cognitive impairment among Chinese older adults: based on the CLHLS. J Affect Disord 295:463–470. https://doi.org/10.1016/j.jad.2021.08.093
WHO Expert Consultation (2004) Appropriate body-mass index for Asian populations and its implications for policy and intervention strategies. Lancet 363:157–163. https://doi.org/10.1016/S0140-6736(03)15268-3
The National Bureau of Statistics of China (2002) Tabulation on the 2000 population census of The Peoples Republic of China. China Statistic Press
Berberich AJ, Hegele RA (2022) A modern approach to dyslipidemia. Endocr Rev 43:611–653. https://doi.org/10.1210/endrev/bnab037
Kopin L, Lowenstein C (2017) Dyslipidemia. Ann Intern Med 167:IT81–IT96. https://doi.org/10.7326/AITC201712050
Ahn J, Lim U, Weinstein SJ et al (2009) Prediagnostic total and high-density lipoprotein cholesterol and risk of cancer. Cancer Epidemiol Biomarkers Prev 18:2814–2821. https://doi.org/10.1158/1055-9965.EPI-08-1248
Guan X-M, Wu S-L, Yang X-L et al (2018) Association of total cholesterol, low-density lipoprotein cholesterol, and non-high-density lipoprotein cholesterol with atherosclerotic cardiovascular disease and cancer in a Chinese male population. Int J Cancer 142:1209–1217. https://doi.org/10.1002/ijc.31149
Loosen SH, Kostev K, Luedde M et al (2022) Low blood levels of high-density lipoprotein (HDL) cholesterol are positively associated with cancer. J Cancer Res Clin Oncol 148:3039–3046. https://doi.org/10.1007/s00432-021-03867-1
His M, Zelek L, Deschasaux M et al (2014) Prospective associations between serum biomarkers of lipid metabolism and overall, breast and prostate cancer risk. Eur J Epidemiol 29:119–132. https://doi.org/10.1007/s10654-014-9884-5
Melvin JC, Holmberg L, Rohrmann S et al (2013) Serum lipid profiles and cancer risk in the context of obesity: four meta-analyses. J Cancer Epidemiol 2013:823849. https://doi.org/10.1155/2013/823849
Eichholzer M, Stähelin HB, Gutzwiller F et al (2000) Association of low plasma cholesterol with mortality for cancer at various sites in men: 17-y follow-up of the prospective Basel study. Am J Clin Nutr 71:569–574. https://doi.org/10.1093/ajcn/71.2.569
Kritchevsky SB, Kritchevsky D (1992) Serum cholesterol and cancer risk: an epidemiologic perspective. Annu Rev Nutr 12:391–416. https://doi.org/10.1146/annurev.nu.12.070192.002135
Patel KK, Kashfi K (2022) Lipoproteins and cancer: the role of HDL-C, LDL-C, and cholesterol-lowering drugs. Biochem Pharmacol 196:114654. https://doi.org/10.1016/j.bcp.2021.114654
Murai T (2012) The role of lipid rafts in cancer cell adhesion and migration. Int J Cell Biol 2012:763283. https://doi.org/10.1155/2012/763283
Murai T (2015) Cholesterol lowering: role in cancer prevention and treatment. Biol Chem 396:1–11. https://doi.org/10.1515/hsz-2014-0194
Murai T, Maruyama Y, Mio K et al (2011) Low cholesterol triggers membrane microdomain-dependent CD44 shedding and suppresses tumor cell migration. J Biol Chem 286:1999–2007. https://doi.org/10.1074/jbc.M110.184010
King RJ, Singh PK, Mehla K (2022) The cholesterol pathway: impact on immunity and cancer. Trends Immunol 43:78–92. https://doi.org/10.1016/j.it.2021.11.007
Huang B, Song B-L, Xu C (2020) Cholesterol metabolism in cancer: mechanisms and therapeutic opportunities. Nat Metab 2:132–141. https://doi.org/10.1038/s42255-020-0174-0
Mullen PJ, Yu R, Longo J et al (2016) The interplay between cell signalling and the mevalonate pathway in cancer. Nat Rev Cancer 16:718–731. https://doi.org/10.1038/nrc.2016.76
Park J-H, Choi M, Kim J-H et al (2020) Metabolic syndrome and the risk of thyroid cancer: a nationwide population-based cohort study. Thyroid 30:1496–1504. https://doi.org/10.1089/thy.2019.0699
Touvier M, Fassier P, His M et al (2015) Cholesterol and breast cancer risk: a systematic review and meta-analysis of prospective studies. Br J Nutr 114:347–357. https://doi.org/10.1017/S000711451500183X
Johnson KE, Siewert KM, Klarin D et al (2020) The relationship between circulating lipids and breast cancer risk: a Mendelian randomization study. PLoS Med 17:e1003302. https://doi.org/10.1371/journal.pmed.1003302
Nowak C, Ärnlöv J (2018) A Mendelian randomization study of the effects of blood lipids on breast cancer risk. Nat Commun 9:3957. https://doi.org/10.1038/s41467-018-06467-9
Yager JD, Davidson NE (2006) Estrogen carcinogenesis in breast cancer. N Engl J Med 354:270–282. https://doi.org/10.1056/NEJMra050776
Jung KY, Ahn HY, Han SK et al (2017) Association between thyroid function and lipid profiles, apolipoproteins, and high-density lipoprotein function. J Clin Lipidol 11:1347–1353. https://doi.org/10.1016/j.jacl.2017.08.015
Borena W, Stocks T, Jonsson H et al (2011) Serum triglycerides and cancer risk in the metabolic syndrome and cancer (Me-Can) collaborative study. Cancer Causes Control 22:291–299. https://doi.org/10.1007/s10552-010-9697-0
Fang Z, He M, Song M (2021) Serum lipid profiles and risk of colorectal cancer: a prospective cohort study in the UK Biobank. Br J Cancer 124:663–670. https://doi.org/10.1038/s41416-020-01143-6
Chandler PD, Song Y, Lin J et al (2016) Lipid biomarkers and long-term risk of cancer in the Women’s Health Study. Am J Clin Nutr 103:1397–1407. https://doi.org/10.3945/ajcn.115.124321
Ulmer H, Borena W, Rapp K et al (2009) Serum triglyceride concentrations and cancer risk in a large cohort study in Austria. Br J Cancer 101:1202–1206. https://doi.org/10.1038/sj.bjc.6605264
Borgquist S, Butt T, Almgren P et al (2016) Apolipoproteins, lipids and risk of cancer. Int J Cancer 138:2648–2656. https://doi.org/10.1002/ijc.30013
Lin X, Lu L, Liu L et al (2017) Blood lipids profile and lung cancer risk in a meta-analysis of prospective cohort studies. J Clin Lipidol 11:1073–1081. https://doi.org/10.1016/j.jacl.2017.05.004
Balaban S, Lee LS, Schreuder M, Hoy AJ (2015) Obesity and cancer progression: is there a role of fatty acid metabolism? Biomed Res Int 2015:274585. https://doi.org/10.1155/2015/274585
Novosyadlyy R, Lann DE, Vijayakumar A et al (2010) Insulin-mediated acceleration of breast cancer development and progression in a nonobese model of type 2 diabetes. Cancer Res 70:741–751. https://doi.org/10.1158/0008-5472.CAN-09-2141
Rehm J, Shield KD, Weiderpass E (2020) Alcohol consumption. A leading risk factor for cancer. Chem Biol Interact 331:109280. https://doi.org/10.1016/j.cbi.2020.109280
Luo J, Yang H, Song B-L (2020) Mechanisms and regulation of cholesterol homeostasis. Nat Rev Mol Cell Biol 21:225–245. https://doi.org/10.1038/s41580-019-0190-7
Martin-Perez M, Urdiroz-Urricelqui U, Bigas C et al (2022) The role of lipids in cancer progression and metastasis. Cell Metab 34:1675–1699. https://doi.org/10.1016/j.cmet.2022.09.023
Wu Q, Huang Y, Kong X et al (2023) DBLiPro: a database for lipids and proteins in human lipid metabolism. Phenomics. https://doi.org/10.1007/s43657-023-00099-w
Acknowledgements
This work was supported by the National Key Research and Development Program of China (2019YFC1315804, 2017YFC0907000), an Innovation Grant from Science and Technology Commission of Shanghai Municipality, China (20ZR1405600), the National Natural Science Foundation of China (82073637, 82122060), the Three-Year Action Plan for Strengthening Public Health System in Shanghai (GWV-10.2-YQ32), the Discipline Promotion Program of Shanghai Fourth People’s Hospital (SY-XKZT-2020-1002), and the Local High-Level Discipline Construction Project of Shanghai. The authors would like to acknowledge that Yanfeng Jiang, Xingdong Chen, and Chen Suo have contributed equally to the correspondence work. The authors would also like to thank all the study participants in this study and all workgroup staff of the Community Health Centers from Zhongshan, Xinqiao, Sheshan, and Maogang in the Songjiang district for their contribution to data collection in the field.
Author information
Authors and Affiliations
Contributions
YJX: conceptualization, formal analysis, and writing—original draft. YGJ: resources and data curation. YLW and XYS: investigation. DLZ, PPG, HBY, JRW, KLX, and TJZ: methodology. YX and QZ: data curation. QHM: resources and funding acquisition. XDC: supervision and funding acquisition. GMZ: supervision and resources. YFJ: supervision and writing—review and editing. CS: conceptualization, supervision, funding acquisition, and writing—review and editing. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflicts of interest.
Ethics approval
The ethics approval was exempted by Fudan University Institution Review Board (IRB#2016-04-0586).
Research involving human participants and/or animals
The present study complies with the guidelines for human studies.
Informed consent
Informed consent was obtained from all participants.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Xie, Y., Jiang, Y., Wu, Y. et al. Association of serum lipids and abnormal lipid score with cancer risk: a population-based prospective study. J Endocrinol Invest 47, 367–376 (2024). https://doi.org/10.1007/s40618-023-02153-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40618-023-02153-w