Abstract
Background
Throughout the coronavirus (COVID-19) pandemic, research revealed people of color were more likely to be infected, have severe illness, and die due to the virus. However, some areas in the USA are now reporting a new shift; lower Black and Hispanic COVID-19 mortality rates compared to their White counterparts. Research indicates that this shift is the result of COVID-19’s impact on disparities by race. In this paper, we analyze death data to determine if the new shift has occurred locally. Specifically, we examined COVID-19 prevalence and related death data in Connecticut by comparing race/ethnicity through two periods of time: one before and one after the first case of the Omicron variant of COVID-19.
Methods
This cross-sectional epidemiological analysis to examine cases and deaths by racial/ethnic status utilizes Connecticut data from March 2020 to February 2022. The following assumption is applied: expected pre-Omicron cases and deaths from March 5, 2020 to November 27, 2021 are equal to the number of cases and deaths during Omicron cases and deaths from November 28, 2021 to February 17, 2022. Race/ethnicity are operationalized as non-Hispanic White, non-Hispanic Black, and Hispanic.
Results
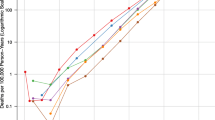
Pre-Omicron (March 5, 2020 to November 27, 2021) compared to the monthly aged adjusted COVID-19 case rate for Whites (394/10,000 populations), Blacks had a higher rate (501/10,000 populations), and Hispanics had the highest (585/10,000 populations). During the Omicron period (November 28 to February 17, 2022), significant changes in COVID-19 case rates were observed in all three ethnic groups, but the biggest changes were observed in Hispanics, followed by Blacks, and then Whites. The rate ratios further showed a remarkable reduction of 47% in case rates (from 1.0 pre-Omicron and from 1.47 during Omicron, p < 0.0001) for Hispanics, when compared to that of Whites. While Blacks showed a significant, smaller reduction of 5% in case rates (from 1.27 pre-Omicron and from 1.22 during the Omicron, p < 0.001) when compared to Whites. Regarding COVID-19-related mortality, the racial differences were similar.
Conclusions and Relevance
By examining Connecticut’s COVID-19 death and case data, this study identified the new shift that occurred locally. The current shift may be anchored in the evolution of the COVID-19 virus, public health guidelines/policies, and the degree to which populations have complied with public health recommendations.
Similar content being viewed by others
Data Availability
The data for this manuscript is publicly available, de-identified data from the Connecticut Department of Health. There is no code associated with this dataset. As the data is de-identified and publicly available, Ethics approval/participant consent was not required.
References
Laurencin CT, Walker JM. A pandemic on a pandemic: racism and COVID-19 in Blacks. Cell Syst. 2020;11(1):9–10. https://doi.org/10.1016/j.cels.2020.07.002.
Kim EJ, Marrast L, Conigliaro J. COVID-19: magnifying the effect of health disparities. J Gen Intern Med. 2020;35(8):2441–2. https://doi.org/10.1007/s11606-020-05881-4.
Podewils LJ, Burket TL, Mettenbrink C, et al. Disproportionate incidence of COVID-19 infection, hospitalizations, and deaths among persons identifying as Hispanic or Latino — Denver, Colorado March–October 2020. MMWR Morb Mortal Wkly Rep. 2020;69:1812–16. https://doi.org/10.15585/mmwr.mm6948a3external.
Laurencin CT, McClinton A. The COVID-19 pandemic: a call to action to identify and address racial and ethnic disparities. J Racial Ethn Health Disparities. 2020;7:398–402. https://doi.org/10.1007/s40615-020-00756-0.
Laurencin CT, Wu ZH, McClinton A, Grady JJ, Walker JM. Excess deaths among Blacks and Latinx compared to whites during Covid-19. J Racial Ethn Health Disparities. 2021;8(3):783–9. https://doi.org/10.1007/s40615-021-01010-x.
Anderson-Carpenter KD, Neal ZP. Racial disparities in COVID-19 impacts in Michigan, USA. J Racial Ethn Health Disparities. 2022;9(1):156–64. https://doi.org/10.1007/s40615-020-00939-9.
Laurencin CT, Wu ZH, Grady JJ, Wu R, Walker JM. Changes in COVID-19-associated deaths during a year among Blacks and Hispanics compared to Whites in the State of Connecticut. J Racial Ethn Health Disparities. 2022;9(5):2049–55. https://doi.org/10.1007/s40615-021-01143-z.
Glance LG, Thirukumaran CP, Dick AW. The unequal burden of COVID-19 deaths in counties with high proportions of Black and Hispanic residents. Med Care. 2021;59(6):470–6. https://doi.org/10.1097/MLR.0000000000001522.
Gupta R, Agrawal R, Bukhari Z, Jabbar A, Wang D, Diks J, Alshal M, Emechebe DY, Brunicardi FC, Lazar JM, Chamberlain R, Burza A, Haseeb MA. Higher comorbidities and early death in hospitalized African-American patients with Covid-19. BMC Infect Dis. 2021;21(1):78. https://doi.org/10.1186/s12879-021-05782-9.
Gauthorp E. The color of coronavirus: COVID-19 deaths by race and ethnicity in the U.S. APM Research Lab. 2023. Retrieved 10-9-2023 from https://www.apmresearchlab.org/covid/deaths-by-race
Koons C. Black, Hispanic New Yorkers are dying at high rates of COVID-19. 2020. Bloommberg. Retrieved 6-7-2023 from https://www.bloomberg.com/news/articles/2020-04-08/black-hispanic-new-yorkers-are-dying-at-high-rates-of-covid-19#xj4y7vzkg.
Laurencin CT, Valantine H, Yancy C, Jones CP, Bright C. The Covid-19 vaccine and the Black community: addressing the justified questions. J Racial Ethn Health Disparities. 2021;8:809–20. https://doi.org/10.1007/s40615-021-01082-9.
Johnson A, Keating D. Whites now more likely to die from COVID than Blacks: why the pandemic shifted. Washington Post. 2022. Retrieved 10-9-2023 from https://www.washingtonpost.com/health/2022/10/19/covid-deaths-us-race/.
Laurencin CT. Addressing justified vaccine hesitancy in the Black community. J Racial Ethn Health Disparities. 2021;8(3):543–6. https://doi.org/10.1007/s40615-021-01025-4.
Alobuia WM, Dalva-Baird NP, Forrester JD, Bendavid E, Bhattacharya J, Kebebew E. Racial disparities in knowledge, attitudes and practices related to COVID-19 in the USA. J Public Health (Oxf). 2020;42(3):470–8. https://doi.org/10.1093/pubmed/fdaa069.
Poteat T, Millett GA, Nelson LE, Beyrer C. Understanding COVID-19 risks and vulnerabilities among black communities in America: the lethal force of syndemics. Ann Epidemiol. 2020;47:1–3. https://doi.org/10.1016/j.annepidem.2020.05.004.
Centers for Disease Control and Prevention. COVID-19: People with certain medical conditions. 2023. Retrieved 10-9-2023 from https://www.cdc.gov/coronavirus/2019-ncov/need-extra-precautions/people-with-medical-conditions.html.
Kriss JL, Hung M, Srivastav A, et al. COVID-19 Vaccination coverage, by race and ethnicity — national immunization survey adult COVID module, United States, December 2020–November 2021. MMWR Morb Mortal Wkly Rep. 2022;71:757–63. https://doi.org/10.15585/mmwr.mm7123a2.
Pham O, Ndugga N, Hill L, Artiga S, Alam R, Parker N. Latest data on COVID-19 vaccinations race/ethnicity. Kaiser Family Foundation. 2022. Retrieved 01-20-2023 from https://www.kff.org/coronavirus-covid-19/issue-brief/latest-data-on-covid-19-vaccinations-race-ethnicity/.
LaVeist T, Benjamin G. 60 black health experts urge Black Americans to get vaccinated. The New York Times. 2021. Retrieved 10-9-2023 from https://www.nytimes.com/2021/02/07/opinion/covid-black-americans.html?auth=login-google1tap&login=google1tap.
Author information
Authors and Affiliations
Contributions
The manuscript was conceptualized and written through the contributions of all authors. All authors have approved the final version of the manuscript.
Corresponding author
Ethics declarations
Conflict of Interest
Dr. Cato T. Laurencin is the editor-in-chief of Racial and Ethnic Health Disparities. He does not have other relevant financial or non-financial interests to disclose. The remaining authors have no relevant financial or non-financial interests to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Laurencin, C.T., Wu, Z., Grady, J.J. et al. The Shift: COVID-19-Associated Deaths are Now Trending Lower Among Blacks and Hispanics Compared to Whites. J. Racial and Ethnic Health Disparities 10, 3188–3193 (2023). https://doi.org/10.1007/s40615-023-01823-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40615-023-01823-y