Abstract
Contingency management is an intervention for substance use disorders based on operant principles. The evidence base in support of contingency management is massive. It is effective in treating substance use disorder in general and opioid use disorder in particular. Dissemination has remained slow despite the urgency created by the opioid epidemic. Key barriers include a lack of expertise, time, and money. Implementing contingency management with smartphones eliminates the need for special training. It also solves logistical issues and requires little time on the part of clinicians. Thus, remaining barriers relate to cost. Federal anti-kickback regulations complicate solutions to the cost barrier. Other important regulatory challenges related to cost include the lack of billing codes and the difficulty of obtaining FDA approval for digital therapeutics. Even after the cost barrier is overcome, provider adoption is not guaranteed. Incentivizing providers for collaborative care may increase adoption and generate referrals. Recently proposed legislation and governmental policy statements provide optimism regarding the near-term large-scale adoption of contingency management in the treatment of opioid use disorder.
Similar content being viewed by others
Notes
Dallery et al. (2015) and Andrade and DeFulio (2017) offer chapter-length coverage of CM including descriptions of procedural differences across variants. For a book-length treatment, see Higgins et al. (2007). For instructions regarding CM design and implementation considerations see Meredith et al. (2014), and for a book-length treatment of this topic, see Petry (2011).
In addition to adoption by Medi-Cal, positive signs of broad support for CM include adoption of Prescription Digital Therapeutics that include CM by MassHealth (Massachusetts’ Medicaid program), and ongoing Medicaid pilot programs in other states such as Vermont, as well as State Bill S7543 under consideration in the New York State Senate’s 2021–2022 session. Review of press releases posted to the websites of companies that provide CM services (e.g., Affect Therapeutics, DynamiCare Health, Pear Therapeutics) illustrates that these companies have been increasingly successful in securing direct service contracts from payers such as Blue Cross Blue Shield and Aetna, among others. This recent increase in support adds to prior key dissemination victories such as inclusion of CM in NIDA Clinical Trials Network studies (e.g., Peirce et al., 2006) and nationwide adoption of CM by the U.S. Department of Veterans Affairs (Petry et al., 2014).
References
Abraham, A. J., Knudsen, H. K., Rothrauff, T. C., & Roman, P. M. (2010). The adoption of alcohol pharmacotherapies in the Clinical Trials Network: The influence of research network participation. Journal of Substance Abuse Treatment, 38(3), 275–283.
Ainscough, T. S., McNeill, A., Strang, J., Calder, R., & Brose, L. S. (2017). Contingency management interventions for non-prescribed drug use during treatment for opiate addiction: A systematic review and meta-analysis. Drug & Alcohol Dependence, 178, 318–339.
Alford, D. P., LaBelle, C. T., & Kretsch, N. (2011). Collaborative care of opioid-addicted patients in primary care using buprenorphine. Health Care Reform, 171(5), 425–431.
Andrade, L. F., & DeFulio, A. (2017). Contingency management treatments for drug use. In J. C. Todorov (Ed.), Trends in behavior analysis (Vol. 2, pp. 4–37). Mauricio Galinkin/Technopolitik.
Asch, D. A., Troxel, A. B., Stewart, W. F., Sequist, T. D., Jones, J. B., Hirsch, A. G., Hoffer, K., Zhu, J., Wang, W., Hodlofski, A., Frasch, A. B., Weiner, M. G., Finnerty, D. D., Rosenthal, M. B., Gangemi, K., & Volpp, K. G. (2015). Effect of financial incentives to physicians, patients, or both on lipid levels. Journal of the American Medical Association, 314(18), 1926–1935.
Baer, D. M., Wolf, M. M., & Risley, T. R. (1987). Some still-current dimensions of applied behavior analysis. Journal of Applied Behavior Analysis, 20(4), 313–327.
Benishek, L. A., Kirby, K. C., Dugosh, K. L., & Padovano, A. (2010). Beliefs about the empirical support of drug abuse treatment interventions: A survey of outpatient treatment providers. Drug & Alcohol Dependence, 107(2–3), 202–208.
Benishek, L. A., Dugosh, K. L., Kirby, K. C., Matejkowski, Clements, N. T., Seymour, B. L., & Festinger, D. S. (2014). Prize-based contingency management for the treatment of substance abusers: A meta-analysis. Addiction, 109(9), 1426–1436.
Bickel, W. K., & Marsch, L. A. (2001). Toward a behavioral economic understanding of drug dependence: Delay discounting processes. Addiction, 96(1), 73–86.
Bickel, W. K., Johnson, M. W., Koffarnus, M. N., MacKillop, J., & Murphy, J. G. (2014). The behavioral economics of substance use disorders: Reinforcement pathologies and their repair. Annual Review of Clinical Psychology, 10, 641–677.
Bigelow, G. E. (2001). An operant behavioral perspective on alcohol abuse and dependence. In N. Heather, T. J. Peters, & T. Stockwell (Eds.), International handbook of alcohol dependence and problems (pp. 299–315). John Wiley & Sons.
Bond, L., Davie, G., Carlin, J. B., Lester, R., & Nolan, T. (2002). Increases in vaccination coverage for children in child care, 1997 to 2000: An evaluation of the impact of government incentives and initiatives. Australian & New Zealand Journal of Public Health, 26(1), 58–64.
Bride, B. E., Abraham, A. J., & Roman, P. M. (2010). Diffusion of contingency management and attitudes regarding its effectiveness and acceptability. Substance Abuse, 31(3), 127–135.
Brown, H. D., & DeFulio, A. (2020). Contingency management for the treatment of methamphetamine use disorder: A systematic review. Drug & Alcohol Dependence, 216, Article 108307.
California State Senate District 11. (2021). Senator Wiener’s recovery incentives act, confronting growing meth and overdose crisis, passes unanimously. https://sd11.senate.ca.gov/news/20210602-senator-wiener%E2%80%99s-recovery-incentives-act-confronting-growing-meth-and-overdose-crisis. Accessed 2 Jan 2022.
Carroll, K. M., & Rounsaville, B. J. (2007). A perfect platform: Combining contingency management with medications for drug abuse. American Journal of Drug & Alcohol Abuse, 33(3), 343–365.
Carroll, K. M., Ball, S. A., Jackson, R., Martino, S., Petry, N. M., Stitzer, M. L., Wells, E. A., & Weiss, R. D. (2011). Ten take home lessons from the first 10 years of the CTN and 10 recommendations for the future. American Journal of Drug & Alcohol Abuse, 35(5), 275–282.
Castells, X., Kosten, T. R., Capellà, D., Vidal, X., Colom, J., & Casas, M. (2009). Efficacy of opiate maintenance therapy and adjunctive interventions for opioid dependence with comorbid cocaine use disorders: A systematic review and meta-analysis of controlled clinical trials. American Journal of Drug & Alcohol Abuse, 35(5), 339–349.
Centers for Disease Control and Prevention. (2020). Understanding the epidemic. https://www.cdc.gov/drugoverdose/epidemic/index.html and NCHS Data Brief No. 394, December 2020. Accessed 2 Jan 2022.
Dallery, J., DeFulio, A., & Meridith, S. (2015). Applied behavior analysis and substance abuse. In H. Roane, T. Falcomata, & J. Ringdahl (Eds.), Clinical and organizational applications of applied behavior analysis. Elsevier.
Dallery, J., Raiff, B. R., Grabinski, M. J., & Marsch, L. A. (2019). Technology-based contingency management in the treatment of substance use disorders. Perspectives on Behavior Science, 42, 445–464.
Daniulaityte, R., Silverstein, S. M., Crawford, T. N., Martins, S. S., Zule, W., Zaragoza, A. J., & Carlson, R. G. (2020). Methamphetamine use and its correlates among individuals with opioid use disorder in a Midwestern U.S. city. Substance Use & Misuse, 55(11), 1781–1789.
DeFulio, A., & Silverman, K. (2012). The use of incentives to reinforce medication adherence. Preventive Medicine, 55(Suppl), S86–S94.
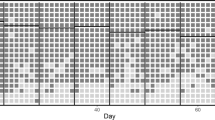
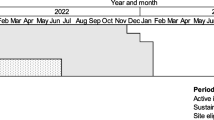
DeFulio, A., Furgeson, J., Brown, H. D., & Ryan, S. (2021a). A smartphone-smartcard platform for implementing contingency management in buprenorphine maintenance patients with concurrent stimulant use disorder. Frontiers in Psychiatry, 12, Article 778992.
DeFulio, A., Rzeszutek, M. J., Furgeson, J., Ryan, S., & Rezania, S. (2021b). A smartphone-smartcard platform for contingency management in an inner-city substance use disorder outpatient program. Journal of Substance Abuse Treatment, 120, Article 108188.
Department of Health & Human Services, Office of Inspector General. (2020). Medicare and state health care programs: Fraud and abuse; Revisions to safe harbors under the anti-kickback statute, and civil monetary penalty rules regarding beneficiary inducements; Final rule. Federal Register, 85(232), 77684–77895.
Ducharme, L. J., Knudsen, H. K., Abraham, A. J., & Roman, P. M. (2010). Counselor attitudes toward the use of motivational incentives in addiction treatment. American Journal on Addiction, 19(6), 496–503.
Dutra, L., Stathopoulou, G., Basden, S. L., Leyro, T. M., Powers, M. B., & Otto, M. W. (2008). A meta-analytic review of psychosocial interventions for substance use disorders. American Journal of Psychiatry, 165(2), 179–187.
Eijkenaar, F., Emmert, M., Scheppach, M., & Schöffski, O. (2013). Effects of pay for performance in health care: A systematic review of systematic reviews. Health Policy, 110(2–3), 115–130.
Emanuel, E. J., Ubel, P. A., Kessler, J. B., Meyer, G., Muller, R. W., Navathe, A. S., Patel, P., Pearl, R., Rosenthal, M. B., Sacks, L., Sen, A. P., Sherman, P., & Volpp, K. G. (2016). Using behavioral economics to design physician incentives that deliver high-value care. Annals of Internal Medicine, 164(2), 114–119.
Fairbrother, G., Hanson, K. L., Friedman, S., & Butts, G. C. (1999). The impact of physician bonuses, enhanced fees, and feedback on childhood immunization coverage rates. American Journal of Public Health, 89(2), 71–175.
Florence, C., Luo, F., & Rice, K. (2021). The economic burden of opioid use disorder and fatal opioid overdose in the United States, 2017. Drug & Alcohol Dependence, 218, Article 108350.
Food & Drug Administration. (2019). Policy for device software functions and mobile medical applications: Guidance for industry and Food and Drug Administration staff. https://www.fda.gov/media/80958/download. Accessed 2 Jan 2022.
Foster, S., Lee, K., Edwards, C., Pelullo, A. P., Khatri, U. G., Lowenstein, M., & Perrone, J. (2020). Providing Incentive for Emergency Physician X-Waiver Training: An Evaluation of Program Success and Postintervention Buprenorphine Prescribing. Annals of Emergency Medicine, 76(2), 206–214.
Griffith, J. D., Rowan-Szal, G. A., Roark, R. R., & Simpson, D. D. (2000). Contingency management in outpatient methadone treatment: a meta-analysis. Drug and Alcohol Dependence, 58(1-2), 55–66.
Hartzler, B., & Rabun, C. (2013). Community opioid treatment perspectives on contingency management: Perceived feasibility, effectiveness, and transportability of social and financial incentives. Journal of Substance Abuse Treatment, 45(2), 242–248.
Hartzler, B., Jackson, T. R., Jones, B. E., Beadnell, B., & Calsyn, D. A. (2014). Disseminating contingency management: Impacts of staff training and implementation at an opiate treatment program. Journal of Substance Abuse Treatment, 46(4), 429–438.
Heinrich, C. J., & Hill, C. J. (2008). Role of State Policies in the Adoption of Naltrexone for Substance Abuse Treatment: Role of State Policies in the Adoption of Naltrexone. Health Services Research, 43(3), 951–970.
Higgins, S. T., Budney, A. J., Bickel, W. K., Foerg, F. E., Donham, R., & Badger, G. J. (1994). Incentives improve outcome in outpatient behavioral treatment of cocaine dependence. Archives of General Psychiatry, 51, 568–576.
Higgins, S. T., Silverman, K., & Heil, S. H. (Eds.). (2007). Contingency management in substance abuse treatment. Guilford Press.
Higgins, S. T., Bernstein, I. M., Washio, Y., Heil, S. H., Badger, G. J., Skelly, J. M., Higgins, T. M., & Solomon, L. J. (2010). Effects of smoking cessation with voucher-based contingency management on birth outcomes. Addiction, 105(11), 2023–2030.
Higgins, S. T., Kurti, A. N., & Davis, D. R. (2019). Voucher-based contingency management is efficacious but underutilized in treating addictions. Perspectives on Behavior Science, 42(3), 501–524.
Hser, Y. I., Saxon, A. J., Huang, D., Hasson, A., Thomas, C., Hillhouse, M., Jacobs, P., Teruya, C., McLaughlin, P., Wiest, K., Cohen, A., & Ling, W. (2014). Treatment retention among patients randomized to buprenorphine/naloxone compared to methadone in a multi-site trial. Addiction, 109(1), 79–87.
Jarvis, B. P., Holtyn, A. F., DeFulio, A., Dunn, K. E., Everly, J. J., Leoutsakos, J.-M. S., Umbricht, A., Fingerhood, M., Bigelow, G. E., & Silverman, K. (2017). Effects of incentives for naltrexone adherence on opiate abstinence in heroin-dependent adults. Addiction, 112(5), 830–837.
Jarvis, B. P., Holtyn, A. F., DeFulio, A., Koffarnus, M. N., Leoutsakos, J.-M. S., Umbricht, A., Fingerhood, M., Bigelow, G. E., & Silverman, K. (2019). The effects of extended-release injectable naltrexone and incentives for opiate abstinence in heroin-dependent adults in a model therapeutic workplace: A randomized trial. Drug and Alcohol Dependence, 197, 220–227.
Kadden, R. M., Litt, M. D., Kabela-Cormier, E., & Petry, N. M. (2007). Abstinence rates following behavioral treatments for marijuana dependence. Addictive Behaviors, 32, 1220–1236.
Kates, N., Arroll, B., Currie, E., Hanlon, C., Gask, L., Klasen, H., Meadows, G., Rukundo, G., Sunderji, N., Ruud, T., & Williams, M. (2019). Improving collaboration between primary care and mental health services. World Journal of Biological Psychiatry, 20(10), 748–765.
Kirby, K. C., Benishek, L. A., Dugaosh, K. L., & Kerwin, M. E. (2006). Substance abuse treatment providers’ beliefs and objections regarding contingency management: Implications for dissemination. Drug and Alcohol Dependence, 85(1), 19–27.
Kirby, K. C., Carpenedo, C. M., Stitzer, M. L., Dugosh, K. L., Petry, N. M., Roll, J. M., Saladin, M. E., Cohen, A. J., Hamilton, J., Reese, K., Sillo, G. R., Stabile, P. Q., & Sterling, R. C. (2012). Is exposure to an effective contingency management intervention associated with more positive provider beliefs? Journal of Substance Abuse Treatment, 42(4), 356–365.
Koffarnus, M. N., Bickel, W. K., & Kablinger, A. S. (2018). Remote alcohol monitoring to facilitate incentive-based treatment for alcohol use disorder: A randomized trial. Alcoholism, Clinical and Experimental Research, 42(12), 2423–2431.
Krawczyk, N., Williams, A. R., Saloner, B., & Cerdá, M. (2021). Who stays in medication treatment for opioid use disorder? A national study of outpatient specialty treatment settings. Journal of Substance Abuse Treatment, 126, Article number 108329.
Kung, F. P., Tsai, C. F., Lu, C. L., Huang, L. C., & Lu, C. H. (2020). Diabetes pay-for-performance program can reduce all-cause mortality in patients with newly diagnosed type 2 diabetes mellitus. Medicine, 99(7), e19139.
Kurti, A. N., Davis, D. R., Redner, R., Jarvis, B. P., Zvorsky, I., Keith, D. R., Bolivar, H. A., White, T. J., Rippberger, P., Markesich, C., Atwood, G., & Higgins, S. T. (2016). A review of the literature on remote monitoring technology in incentive-based interventions for health-related behavior change. Translational Issues in Psychological Science., 2(2), 128–152.
LaBelle, C. T., Han, S. C., Bergeron, A., & Samet, J. H. (2016). Office-based opioid treatment with buprenorphine (OBOT-B): State-wide implementation of the Massachusetts Collaborative Care Model in community health centers. Journal of Substance Abuse Treatment, 60, 6–13.
Li, J., Patel, B., Giardino, A. P., Camp, E. A., & Macias, C. G. (2019). The effect of a primary care provider incentive program on pediatric emergency medicine visits. Pediatric Emergency Care, 35(5), 363–368.
Lussier, J. P., Heil, S. H., Mongeon, J. A., Badger, G. J., & Higgins, S. T. (2006). A meta-analysis of voucher-based reinforcement therapy for substance use disorders. Addiction, 101(2), 192–203.
Maricich, Y. A., Bickel, W. K., Marsch, L. A., Gatchalian, K., Botbyl, J., & Luderer, H. F. (2021). Safety and efficacy of a prescription digital therapeutic as an adjunct to buprenorphine for treatment of opioid use disorder. Current Medical Research and Opinion, 37(2), 167–173.
McGovern, M. P., & Carroll, K. M. (2003). Evidence-based practices for substance use disorders. Psychiatric Clinics of North America, 26(4), 991–1010.
Meredith, S. E., Jarvis, B. P., Raiff, B., Rojewski, A. M., Kurti, A., Cassidy, R. N., Erb, P., Sy, J. R., & Dallery, J. (2014). The ABCs of incentive-based treatment in health care: A behavior analytic framework to inform research and practice. Psychology Research and Behavior Management, 7, 103–114.
Milby, J. B., Schumacher, J. E., Raczynski, J. M., Caldwell, E., Engle, M., Michael, M., & Carr, J. (1996). Sufficient conditions for effective treatment of substance abusing homeless persons. Drug and Alcohol Dependence, 43(1-2), 39–47.
Miller, W. R., Sorensen, J. L., Selzer, J. A., & Brigham, G. S. (2006). Disseminating evidence-based practices in substance abuse treatment: A review with suggestions. Journal of Substance Abuse Treatment, 31(1), 25–39.
National Institute on Drug Abuse. (1978). Self-administration of abused substances: Methods for study. Research Monograph, 20, NTIS PB 288471.
Newsome, G. (2021). Veto of California State Bill 110. https://www.gov.ca.gov/wp-content/uploads/2021/10/SB-110-1082021.pdf. Accessed 2 Jan 2022.
Notley, C., Gentry, S., Livingstone-Banks, J., Bauld, L., Perera, R., & Hartmann-Boyce, J. (2019). Incentives for smoking cessation. Cochrane Database of Systematic Reviews, 7, CD004307.
Office of National Drug Control Policy. (2021). Biden Harris statement of drug policy priorities April-1. Available from: https://www.whitehouse.gov/wp-content/uploads/2021/03/BidenHarris-Statement-of-Drug-Policy-Priorities-April-1.pdf. Accessed 2 Jan 2022.
Ogundeji, Y. K., Bland, J. M., & Sheldon, T. A. (2016). The effectiveness of payment for performance in health care: A meta-analysis and exploration of variation in outcomes. Health Policy, 120(10), 1141–1150.
Oluwoye, O., Kriegel, L., Alcover, K. C., McPherson, S., McDonell, M. G., & Roll, J. M. (2020). The dissemination and implementation of contingency management for substance use disorders: A systematic review. Psychology of Addictive Behaviors, 34(1), 99–110.
Pace, C. A., & Uebelacker, L. A. (2018). Addressing unhealthy substance use in primary care. Medical Clinics of North America, 102(4), 567–586.
Palmquist, K. B., & Swortwood, M. J. (2021). Quantification of fentanyl analogs in oral fluid using LC-QTOF-MS. Journal of Forensic Science, 66, 1871–1878.
Peirce, J. M., Petry, N. M., Stitzer, M. L., Blane, J., Kellogg, S., Satterfield, F., Schwartz, M., Krasnansky, J., Pencer, E., Silva-Vazquez, L., Kirby, K. C., Royer-Malvestuto, C., Roll, J. M., Cohen, A., Copersino, M. L., & Kolodner, K. (2006). Effects of lower-cost incentives on stimulant abstinence in methadone maintenance treatment: A National Drug Abuse Treatment Clinical Trials Network study. Archives of General Psychiatry, 63, 201–208.
Petry, N. M. (2010). Contingency management treatments: Controversies, and challenges. Addiction, 105(9), 1507–1509.
Petry, N. M. (2011). Contingency management for substance abuse treatment: A guide to implementing this evidence-based practice. Routledge.
Petry, N. M., & Carroll, K. M. (2013). Contingency management is efficacious in opioid-dependent outpatients not maintained on agonist pharmacotherapy. Psychology of Addictive Behaviors, 27(4), 1036–1043.
Petry, N. M., DePhilippis, D., Rash, C. J., Drapkin, M., & McKay, J. R. (2014). Nationwide dissemination of contingency management: The Veterans Administration initiative. American Journal on Addictions, 23, 205–210.
Prendergast, M., Podus, D., Finney, J., Greenwell, L., & Roll, J. (2006). Contingency management for treatment of substance use disorders: a meta-analysis. Addiction, 101(11), 1546–1560.
Ramanuj, P., Ferenchik, E., Docherty, M., Spaeth-Rublee, B., & Pincus, H. A. (2019). Evolving models of integrated behavioral health and primary care. Current Psychiatry Reports, 21(1), Article number 4.
Rash, C. J., Petry, N. M., Kirby, K. C., Martino, S., Roll, J., & Stitzer, M. L. (2012). Identifying provider beliefs related to contingency management adoption using the contingency management beliefs questionnaire. Drug and Alcohol Dependence, 21(3), 205–212.
Rosenthal, M. B., Fernandopulle, R., Song, H. R., & Landon, B. (2004). Paying for quality: Providers’ incentives for quality improvement. Health Affairs, 23(2), 127–141.
Silverman, K. (2004). Exploring the limits and utility of operant conditioning in the treatment of drug addiction. Behavior Analyst, 27(2), 209–230.
Silverman, K., Svikis, D., Robles, E., Stitzer, M. L., & Bigelow, G. E. (2001). A reinforcement-based Therapeutic Workplace for the treatment of drug abuse: Six-month abstinence outcomes. Experimental and Clinical Psychopharmacology, 9(1), 14–23.
Silverman, K., DeFulio, A., & Sigurdsson, S. O. (2012). Maintenance of reinforcement to address the chronic nature of drug addiction. Preventive Medicine, 55(Suppl), S46–S53.
Sordo, L., Barrio, G., Bravo, M. J., Indave, B. I., Degenhardt, L., Wiessing, L., Ferri, M., & Pastor-Barriuso, R. (2017). Mortality risk during and after opioid substitution treatment: Systematic review and meta-analysis of cohort studies. British Medical Journal, 357, j1550.
Stanger, C., & Budney, A. J. (2010). Contingency management approaches for adolescent substance use disorders. Child and Adolescent Psychiatric Clinics of North America, 19(3), 547–562.
Stewart, R. E., Lareef, I., Hadley, T. R., & Mandell, D. S. (2017). Can we pay for performance in behavioral health care? Psychiatric Services, 68(2), 109–111.
Strain, E. C., Stitzer, M. L., Liebson, I. A., & Bigelow, G. (1994). Comparison of buprenorphine and methadone in the treatment of opioid dependence. American Journal of Psychiatry, 151(7), 1025–1030.
Strug, D. L., Hunt, D. E., Goldsmith, D. S., Lipton, D. S., & Spunt, B. (1985). Patterns of cocaine use among methadone clients. International Journal of Addictions, 20, 1163–1175.
Timko, C., Schultz, N. R., Cucciare, M. A., Vittorio, L., & Garrison-Diehn, C. (2016). Retention in medication-assisted treatment for opiate dependence: A systematic review. Journal of Addictive Diseases, 35(1), 22–35.
Van Herck, P., De Smedt, D., Annemans, L., Remmen, R., Rosenthal, M. B., & Sermeus, W. (2010). Systematic review: Effects, design choices, and context of pay-for-performance in health care. BMC Health Services Research, 10, Article number 247.
Vandrey, R., Stitzer, M. L., Acquavita, S. P., & Quinn-Stabile, P. (2011). Pay-for-performance in a community substance abuse clinic. Journal of Substance Abuse Treatment, 41(2), 193–200.
Ward, K., Hull, B. P., & Leask, J. (2013). Financial incentives for childhood immunization – A unique but changing Australian initiative. Medical Journal of Australia, 198(11), 590–592.
Weinstock, J., Alessi, S. M., & Petry, N. M. (2007). Regardless of psychiatric severity the addition of contingency management to standard treatment improves retention and drug use outcomes. Drug and Alcohol Dependence, 87(2-3), 288–296.
Williams, A. R., Samples, H., Crystal, S., & Olfson, M. (2020). Acute care, prescription opioid use, and overdose following discontinuation of long-term buprenorphine treatment for opioid use disorder. American Journal of Psychiatry, 177, 117–124.
Funding
This research was supported by grants R41DA049390 and R44DA055396 from the National Institute on Drug Abuse.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of Interest
The author has served as a research consultant for DynamiCare Health, Inc. This company provides contingency management services for people with substance use disorders.
Research Involving Human Participants and/or Animals
This research is a review and did not involve human participants or animals.
Informed Consent
Because no human participants were involved in this study no informed consent was required.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
DeFulio, A. Dissemination of Contingency Management for the Treatment of Opioid Use Disorder. Perspect Behav Sci 46, 35–49 (2023). https://doi.org/10.1007/s40614-022-00328-z
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40614-022-00328-z