Abstract
Background
The association of visceral adiposity with mortality in older adults is conflicting. Whether age influences the predicting ability of visceral adiposity (VAI) for mortality remains unknown. This study uncovered the relationship between age-adjusted visceral adiposity index and mortality through the data of NHANES 2011–2014.
Methods
This study obtained data from the National Health and Nutrition Examination Survey (NHANES) 2011–2014. The age-adjusted visceral adiposity index (AVAI) scores were expressed as quartiles. Receiver operating characteristics (ROC) curve analysis was also applied to compare the predictive ability for mortality. Multivariate weighted Cox regression models were constructed to explore the association between AVAI and mortality. Kaplan–Meier survival curves were conducted for survival analyses. Smooth curve fittings and two-piecewise linear models were applied to explore the relationships between AVAI and mortality.
Results
This study recruited 4281 subjects aged ≥ 18 years from the NHANES 2011–2014. The AUCs of AVAI were 0.82 (0.79, 0.86) and 0.89 (0.85, 0.92) for predicting all-cause mortality and cardiovascular mortality, which were superior to BMI, WC and VAI (all p < 0.05). AVAI is still an independent predictor for mortality adjusted for confounders. The associations of AVAI with all-cause and cardiovascular mortalities were dose-responsive, with higher AVAI scores indicating higher mortality risks.
Conclusion
Age significantly improves the ability of VAI for predicting all-cause and cardiovascular mortality. Age-adjusted VAI is independently associated with mortality risk, and thus could be considered a reliable parameter for assessing mortality risk.
Similar content being viewed by others
Introduction
Obesity has been recognized as a worldwide epidemic problem leading to a heavy health burden for both individuals and society [1]. The deleterious influences of obesity, such as type 2 diabetes, cancer, and cardiovascular diseases (CVD), have been widely recognized. However, obesity, measured by the body mass index (BMI), has been demonstrated to be protective in older adults, which was termed as “the obesity paradox” [2]. The underlying mechanisms of this phenomenon are complex, but one of them is that BMI does not take the heterogeneity of body fat deposition into account. Mounting evidence showed that the distribution of excessive adiposity, but not obesity itself, impacts cardiovascular diseases and other chronic disorders [3,4,5,6]. It is important to consider body fat distribution when assessing the influence of obesity on health outcomes. Studies indicate that visceral adipose tissue (VAT) is a better parameter representing obesity than whole fat mass [7]. However, methods to measure VAT are expensive and time-consuming, e.g., computed tomography (CT) and magnetic resonance imaging (MRI). Waist circumference (WC) can better reflect the distribution of excessive adipose tissue than BMI [8], but it failed to differentiate subcutaneous and visceral fat well. Moreover, the function of visceral fat differs among individuals [9], making it necessary to develop a parameter that reflects the distribution and function of adipose tissue better and cost-effectively.
Visceral adiposity index (VAI) was created to assess the function of visceral adiposity. VAI is independently associated with cardiovascular and cerebrovascular events in Italians [10]. The sex-specific index comprises simple anthropometric measures and common lipidemic parameters. The VAI formula has BMI, WC, serum triglycerides (TG), and HDL cholesterol (HDL-C) and can reflect visceral adiposity dysfunction. Therefore, VAI is a more useful tool for predicting the incidence of diabetes than its components [11].
However, the association between VAT and all-cause mortality in elders remains conflicting according to previous studies [12,13,14,15]. Some studies showed that central obesity was associated with higher mortality risk [13,14,15], while other longitudinal studies demonstrated that greater VAT fails to predict higher all-cause mortality [12, 16]. The contradictions in these studies suggest that VAI may not be a comprehensive indicator of mortality risk. Age, perhaps an overlooked important factor, might be associated with these inconsistencies. Previous research has demonstrated a close relationship between age and changes in body composition, including reduced muscle mass, increased body fat, and fat infiltration in muscles, all of which are closely associated with functional decline and mortality in the geriatric population. Aging is also associated with changes in localized fat distribution and increased visceral fat mass [17,18,19]. One study has shown that age significantly improves the model fitting for visceral fat area and created a new index to reflect visceral fat volume and function, known as the Chinese Visceral Adiposity Index (CVAI).[20].Therefore, age is an important factor that cannot be ignored. Aging plays a crucial role in mortality and many chronic diseases, including cancer, neurodegeneration, and CVD. Thus, we seek to develop a new index including BMI, WC, HDL-C, TG, and age, termed age-adjusted VAI (AVAI), to better reflect the role of age in VAI. This study aimed to discover the association of AVAI and mortality, and further validate whether AVAI is superior for predicting mortality compared to previous parameters.
Materials and methods
Study population and design
The National Health and Nutrition Examination Survey (NHANES) is a cross-sectional study representing the health and nutritional status of the population within the USA. The Centers for Disease Control and Prevention has approved the NHANES protocol and written informed consent was obtained from all participants. This study enrolled 19,931 respondents from NHANES (2011–2014). A total of 7954 adults remained after excluding individuals less than 18 years. This study also excluded participants with missing VAI-related data (n = 1760) and other covariates (n = 5908) and individuals without follow-up data (n = 28). Finally, 4281 subjects were included. Informed consent was obtained from each subject (Fig. 1).
Assessment of outcomes
We observe all-cause mortality as the end point. Participants were followed up through December 31, 2015 unless dropping out or meeting the intended outcome. The mortality status of participants was authenticated by matching with the National Death Index. Referring to the International Classification of Disease, 10th Edition (ICD-10), Clinical Modification System codes, cardiovascular mortality was identified as death caused by CVD or cerebrovascular disease (ICD-10 codes I00–I09, I11, I13, I20 to I51, and I60–I69).
Anthropometric and serum biochemical parameters
Anthropometric and biochemical data were collected during the NHANES study. Waist circumference (WC) was measured at the iliac crest using a tape measure with a precision of 1 mm. Body mass index (BMI) was calculated by dividing weight in kilograms by the square of height in meters. A blood sample was collected from the antecubital vein of all participants by a trained phlebotomist. Detailed information regarding laboratory testing for triglycerides (TG), total cholesterol (TC), low-density lipoprotein cholesterol (LDL-C), high-density lipoprotein cholesterol (HDL-C), glycated hemoglobin (HbA1c), glucose and insulin levels can be found in the NHANES Laboratory/Medical Technician Procedures Manual [21, 22]. VAI was calculated as follows:
The multivariate regression model incorporated age, race, education level, marital status, hypertension, diabetes, smoking status, WC, BMI, HDL-C, TG, total cholesterol, and glucose. Age was significantly associated with mortality after adjusting for potential confounders and parameters included in VAI. The new index was defined as age-adjusted visceral adiposity index (AVAI) including age, BMI, WC, HDL-C, and TG. AVAI was estimated as follows:
where both TG and HDL levels are expressed in mmol/L[10].
Covariates
The standardized questionnaires and physical examinations were used to assess covariates, including age, sex, race, education level, marital status, smoking status, alcohol consumption, history of hypertension, and diabetes. Disease states were defined in detail. Individuals with an average systolic blood pressure (SBP) ≥ 140 mmHg or an average diastolic blood pressure (DBP) ≥ 90 mmHg, or those diagnosed with hypertension and receiving antihypertensive medication, were classified as having hypertension. Participants with a fasting plasma glucose level ≥ 7.0 mmol/L or an HbA1c level ≥ 6.5%, as well as those with a diagnosed case of diabetes, were designated as having diabetes.
Statistical analysis
All estimates were calculated accounting for NHANES sample weights. AVAI was expressed as quartiles. Continuous variables were checked for normal distribution before analysis, and these variables did not follow a normal distribution. Thus, continuous variables are presented as median (quantile 1st, quantile 3rd), while categorical variables are expressed as percentages, respectively. We conducted Kruskal–Wallis test (continuous variables) or Chi-square tests (categorical variables) to calculate the differences among different groups. Taking into account the complex survey design in NHANES, weighted Cox regression models were constructed to explore the association between AVAI and mortality risk instead of traditional Cox regression, which was expressed as calculated odds ratios (ORs) and 95% confidence interval (95% CIs). Crude analysis adjusted for no covariate (model 1), adjusted model adjusted for age, gender and race (model 2), fully adjusted model adjusted for age, gender, race, marital status, education level, smoking status, hypertension, diabetes, level of systolic blood pressure, glucose and total cholesterol (model 3). Kaplan–Meier survival analyses were applied to analyze the differences of survival rates according to AVAI groups, and the differences were examined by log-rank test. We also conducted smooth curve fittings to address the nonlinearity of AVAI and mortality after adjustment for the same covariates as in the Cox regression models. Then two-piecewise linear regression models were constructed to examine the difference of relationship at the threshold. The point with the highest likelihood among all the possible values was chosen as the threshold value. A logarithmic likelihood ratio test evaluated the differences between two-piecewise linear regression models. Receiver operator characteristic (ROC) curve was used to compare the predictive ability for mortality among AVAI and classical obesity-related parameters.
Empower stars (www.empowerstats.com, X&Y Solutions Inc., Boston, MA) was used for all statistical analyses. P < 0.05 was considered statistically significant.
Results
Population characteristics
This study included 4256 participants aged ≥ 18 years old from NHANES (2011–2014). Among all the participants, the medium age was 48 (34–63) years, and 49.87% were male. Based on AVAI quartiles, the basic characteristics are presented Table 1. All baseline covariates have significant differences among the AVAI groups (all p < 0.01). Subjects with higher AVAI scores had lower HDL-C concentrations and higher age, BMI, WC, glucose level, HbA1c, TG, and systolic blood pressure than those with lower VAI scores (p < 0.01). Meanwhile, individuals with higher AVAI scores were mostly likely to be male, smokers, and those with hypertension and diabetes. Throughout the 35 months of average follow-up period, 3.34% all-cause deaths and 1.05% cardiovascular deaths occurred.
Adjusted VAI improves predictive performance for mortality
ROC curve analysis was used to verify whether VAI has a better predictive ability for mortality than previously established parameters. The area under the ROC curve (AUCs) of VAI for all-cause and cardiovascular mortality was 0.60 (0.56, 0.65) and 0.64 (0.57, 0.72), showing a better predictive ability than BMI, but a lower predictive ability than WC. Moreover, the AUCs of AVAI were 0.82 (0.79, 0.86) and 0.89 (0.85, 0.92) for predicting all-cause mortality and cardiovascular mortality, which were superior to BMI, WC and VAI (Fig. 2 and Table 2).
The relationship of AVAI with mortality
Kaplan–Meier survival curves were diverged according to AVAI quartiles. The highest risk for all-cause and cardiovascular mortality was observed in the group with the highest AVAI score (log-rank p < 0.001) (Fig. 3). Weighted multivariate Cox regression was used to evaluate the relationship between AVAI and mortality risk. After adjusting for potential confounders, compared with the reference (Q1), the HRs (95% CI) for all-cause death was 1.13 (1.12, 1.14), 1.92 (1.90, 1.94), and 2.33 (2.30, 2.36) for Q2, Q3, and Q4 groups, respectively (all P for trend < 0.01). Weighted multivariate Cox regression failed to detect any relationship between AVAI and cardiovascular mortality due to inefficient cardiovascular events (Table 3).
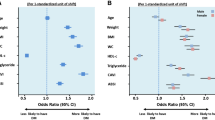
Dose–response relationship between AVAI and mortality risk
We also tried to use smooth curve fittings to find the non-linear relationships between AVAI and mortality risks (Fig. 4). The results of standard logistic regression and two-piecewise linear regression are presented in Table 4. According to two-piecewise linear regression, the cutoff values were − 3.46 for all-cause mortality and − 4.59 for cardiovascular mortality, but the linear relationships were demonstrated by standard linear regression. Therefore, there is a dose–response relationship between AVAI and cause-specific mortality.
Discussion
This was a large-scale, multi-ethnic analysis evaluating the association between AVAI scores and all-cause and cardiovascular mortality in US adults. Individuals with higher AVAI scores also have more cardiovascular risk factors, such as hypertension, diabetes and hyperlipidemia. ROC demonstrated that AVAI is a better predictor than traditional obesity-related parameters for all-cause and cardiovascular mortality, which have higher sensitivity and specificity. Further Cox regression found that AVAI scores are independently associated with mortality in this study regardless of the socioeconomic, medical condition, lifestyle factors, and other covariates. The relationships between AVAI and cause-specific mortality are dose-responsive.
Visceral adiposity promotes metabolic dysfunctions, including type 2 diabetes, hypertension, and hyperlipidemia [23,24,25,26,27]. However, it is difficult to quantify visceral adipose tissues. VAI can be used to reflect visceral adiposity and adipose tissue dysfunction [10]. Some studies have found that VAI is significantly associated with diabetes, hypertension, and cardiovascular disease [28,29,30,31,32,33,34,35,36]. One study discovered that the VAI based on simple measurement has a better predicting ability for CVD than other simple ratios, e.g., BMI and WC [37], However, in the present study, VAI did not show better predicting performance for mortality than waist circumference. The inconsistency could be due to the differences in race and age among the studied cohorts. According to previous studies, aging is an important process influencing body fat distribution and mortality. Evidence has shown that a combination of metabolic syndrome parameters with age can enhance its predictive power [38]. We successfully demonstrated that age-adjusted VAI is independently associated with all-cause mortality and is a better indicator for mortality than simple anthropometric parameters and VAI.
However, obesity has been demonstrated to be a heterogeneous disorder, and there are differences between subcutaneous areas and visceral adipose tissue, including anatomical, cellular, molecular, and physiological aspects [39]. In contrast to subcutaneous adipose tissue, the adipocytes in VAT are larger and dysfunctional, and large adipocytes are insulin resistant and hyperlipolytic, resulting in a higher level of plasma glucose and free fatty acids (FFAs) [40]. Meanwhile, visceral adipose tissue is characterized by being rich in blood supply, and can be seen as an endocrine organ due to its secretory function [41, 42]. Visceral adipose tissue (VAT) adipocytes expand under excess energy intake, and synthesize a variety of proinflammatory proteins, termed adipokines, including leptin, monocyte chemoattractant proteins (MCP-1), tumor necrosis factor (TNF-a) and IL-6. These adipokines contribute to a chronic, low-grade inflammatory state in obesity, which raises the metabolic risk [6, 41,42,43,44,45,46]. Although VAI is a relatively comprehensive and easily measurable index for visceral adipose and significantly associated with insulin resistance, it does not take age into account and cannot comprehensively predict metabolic risk. Similar to obesity, aging is also an important factor influencing the function of visceral adipose tissue and plays a crucial role in many chronic diseases, including cancer, neurodegeneration, and CVD [47, 48]. Aging influences the function of visceral tissue through many mechanisms. Firstly, adipose tissue redistribution occurs with age, and the growth in fat mass occurs mostly with the expansion of the visceral adipose tissue due to the declining levels of hormones, such as testosterone, estrogen, and norepinephrine [49,50,51]. Removing VAT in rats through surgery could improve glucose tolerance, reduce liver triglycerides and increase life span [52, 53]. Secondly, aging also increases the size of VAT depot and promotes larger adipocytes in VAT, and further increases the expression of proinflammatory adipokines in hypertrophic adipocytes [54]. Based on in vitro experiments, older adipocytes decreased the gene expression of adiponectin and leptin and showed significant leptin resistance compared to young mature adipocytes [55]. Aging also processes the activation of stress response through the mitochondrial pathway, which increases reactive oxygen species [56]. Thirdly, immune cells are important component of VAT, such as adipose tissue macrophages (ATMs) [57]. Studies have demonstrated that the proportion of M2-like ATMs significantly decreases in aged mice, and aged ATMs showed increased secretion of proinflammatory cytokines and decreased expression of PPARγ [58, 59]. Therefore, aging is an important factor contributing to the inflammatory state. The term “inflammaging” was used to characterize the chronic low-grade inflammation triggered by endogenous signals that accompany aging. This inflammatory condition raises the incidence of cardiovascular disease, type 2 diabetes, and neurological disorders in geriatric patients [60,61,62,63]. Retrospective observational studies associate metformin with increased human life span and fewer age-related diseases by suppressing adipocyte proinflammatory responses [64]. Therefore, age is significantly associated with dysfunction of adipose and mortality and is essential for predicting mortality risk.
Based on the above discussion, we can conclude that AVAI has certain guiding significance, especially for geriatric patients. Firstly, geriatric patients often have insufficient awareness of changes in their body composition, making it difficult for them to adhere to the detection of such changes, especially with time-consuming and laborious examinations like CT scans. AVAI, as a simple indicator, can be calculated using routine biochemical and physical examination data. This is very helpful for geriatric patients to understand the changes in their body composition, particularly abdominal fat, and to manage it by changing dietary habits and increasing physical exercise. Secondly, AVAI shows good correlation with other metabolic indicators such as blood glucose, blood pressure, and blood lipids, reflecting the overall metabolic burden in geriatric individuals. AVAI can serve as an indicator for assessing the metabolic health status of geriatric patients. By monitoring changes in AVAI, doctors can intervene early and improve the metabolic health of geriatric patients. Lastly, our study found that AVAI outperforms other indicators in predicting mortality risk, which helps doctors assess the risk of mortality in geriatric patients and take appropriate intervention measures in a timely manner.
This study has some strengths, including the large nationwide, representative of US adults and adjustment for main covariates. However, the study also has some limitations. First, visceral adiposity was not measured directly. Second, in the study some variables like smoking status and medical history may lead to recall bias. Moreover, the findings are only applicable to the population in North America and should be cautiously applied to the population in other regions. Data from areas except the USA may help assess whether AVAI is also superior in other races.
Conclusion
Age significantly improves the ability of VAI for predicting all-cause and cardiovascular mortality. Age-adjusted VAI is independently associated with mortality risk, and thus could be considered as a reliable parameter assessing mortality risk. We found that AVAI could stably predict all-cause and cardiovascular mortality in a dose-responsive manner.
Data availability
Publicly available datasets were analyzed in this study. This data can be found here: https://www.cdc.gov/nchs/nhanes/index.htm.
References
Stefan N, Häring HU, Hu FB et al (2013) Metabolically healthy obesity: epidemiology, mechanisms, and clinical implications. Lancet Diabetes Endocrinol 1:152–162. https://doi.org/10.1016/s2213-8587(13)70062-7
Lavie CJ, Milani RV, Ventura HO (2009) Obesity and cardiovascular disease: risk factor, paradox, and impact of weight loss. J Am Coll Cardiol 53:1925–1932. https://doi.org/10.1016/j.jacc.2008.12.068
Després JP (2012) Body fat distribution and risk of cardiovascular disease: an update. Circulation 126:1301–1313. https://doi.org/10.1161/circulationaha.111.067264
Tchernof A, Després JP (2013) Pathophysiology of human visceral obesity: an update. Physiol Rev 93:359–404. https://doi.org/10.1152/physrev.00033.2011
Smith U (2015) Abdominal obesity: a marker of ectopic fat accumulation. J Clin Invest 125:1790–1792. https://doi.org/10.1172/jci81507
Bastien M, Poirier P, Lemieux I et al (2014) Overview of epidemiology and contribution of obesity to cardiovascular disease. Prog Cardiovasc Dis 56:369–381. https://doi.org/10.1016/j.pcad.2013.10.016
Piché ME, Tchernof A, Després JP (2020) Obesity phenotypes, diabetes, and cardiovascular diseases. Circ Res 126:1477–1500. https://doi.org/10.1161/circresaha.120.316101
Britton KA, Massaro JM, Murabito JM et al (2013) Body fat distribution, incident cardiovascular disease, cancer, and all-cause mortality. J Am Coll Cardiol 62:921–925. https://doi.org/10.1016/j.jacc.2013.06.027
Neeland IJ, Ross R, Després JP et al (2019) Visceral and ectopic fat, atherosclerosis, and cardiometabolic disease: a position statement. Lancet Diabetes Endocrinol 7:715–725. https://doi.org/10.1016/s2213-8587(19)30084-1
Amato MC, Giordano C, Galia M et al (2010) Visceral Adiposity Index: a reliable indicator of visceral fat function associated with cardiometabolic risk. Diabetes Care 33:920–922. https://doi.org/10.2337/dc09-1825
Mohammadreza B, Farzad H, Davoud K et al (2012) Prognostic significance of the complex “Visceral Adiposity Index” vs. simple anthropometric measures: Tehran lipid and glucose study. Cardiovasc Diabetol 1:20. https://doi.org/10.1186/1475-2840-11-20
Ballin M, Nordström P, Niklasson J et al (2021) Associations of visceral adipose tissue and skeletal muscle density with incident stroke, myocardial infarction, and all-cause mortality in community-dwelling 70-year-old individuals: a prospective cohort study. J Am Heart Assoc 10:e020065. https://doi.org/10.1161/jaha.120.020065
Shil Hong E, Khang AR, Roh E et al (2015) Counterintuitive relationship between visceral fat and all-cause mortality in an elderly Asian population. Obesity (Silver Spring) 23:220–227. https://doi.org/10.1002/oby.20914
Koster A, Murphy RA, Eiriksdottir G et al (2015) Fat distribution and mortality: the AGES-Reykjavik Study. Obesity (Silver Spring) 23:893–897. https://doi.org/10.1002/oby.21028
de Santana FM, Domiciano DS, Gonçalves MA et al (2019) Association of appendicular lean mass, and subcutaneous and visceral adipose tissue with mortality in older Brazilians: the São Paulo ageing & health study. J Bone Miner Res 34:1264–1274. https://doi.org/10.1002/jbmr.3710
Santanasto AJ, Goodpaster BH, Kritchevsky SB et al (2017) Body composition remodeling and mortality: the health aging and body composition study. J Gerontol A Biol Sci Med Sci 72:513–519. https://doi.org/10.1093/gerona/glw163
Kuk JL, Saunders TJ, Davidson LE et al (2009) Age-related changes in total and regional fat distribution. Ageing Res Rev 8:339–348. https://doi.org/10.1016/j.arr.2009.06.001
Ponti F, Santoro A, Mercatelli D et al (2019) Aging and imaging assessment of body composition: from fat to facts. Front Endocrinol (Lausanne) 10:861. https://doi.org/10.3389/fendo.2019.00861
Szulc P, Duboeuf F, Chapurlat R (2017) Age-related changes in fat mass and distribution in men-the cross-sectional STRAMBO study. J Clin Densitom 20:472–479. https://doi.org/10.1016/j.jocd.2016.08.003
Xia MF, Chen Y, Lin HD et al (2016) A indicator of visceral adipose dysfunction to evaluate metabolic health in adult Chinese. Sci Rep 6:38214. https://doi.org/10.1038/srep38214
Mazidi M, Kengne AP, George ES et al (2021) The association of red meat intake with inflammation and circulating intermediate biomarkers of type 2 diabetes is mediated by central adiposity. Br J Nutr 125:1043–1050. https://doi.org/10.1017/s0007114519002149
Borrud L, Chiappa MM, Burt VL et al (2014) National Health and Nutrition Examination Survey: national youth fitness survey plan, operations, and analysis, 2012. Vital Health Stat 2:1–24
Stefan N (2020) Causes, consequences, and treatment of metabolically unhealthy fat distribution. Lancet Diabetes Endocrinol 8:616–627. https://doi.org/10.1016/s2213-8587(20)30110-8
Longo M, Zatterale F, Naderi J et al (2019) Adipose tissue dysfunction as determinant of obesity-associated metabolic complications. Int J Mol Sci. https://doi.org/10.3390/ijms20092358
Burhans MS, Hagman DK, Kuzma JN et al (2018) Contribution of adipose tissue inflammation to the development of type 2 diabetes mellitus. Compr Physiol 9:1–58. https://doi.org/10.1002/cphy.c170040
Fox CS, Massaro JM, Hoffmann U et al (2007) Abdominal visceral and subcutaneous adipose tissue compartments: association with metabolic risk factors in the Framingham Heart Study. Circulation 116:39–48. https://doi.org/10.1161/circulationaha.106.675355
Hayashi T, Boyko EJ, Leonetti DL et al (2003) Visceral adiposity and the prevalence of hypertension in Japanese Americans. Circulation 108:1718–1723. https://doi.org/10.1161/01.cir.0000087597.59169.8d
Han L, Fu KL, Zhao J et al (2014) Visceral adiposity index score indicated the severity of coronary heart disease in Chinese adults. Diabetol Metab Syndr 6:143. https://doi.org/10.1186/1758-5996-6-143
Li R, Li Q, Cui M et al (2017) Visceral adiposity index, lipid accumulation product and intracranial atherosclerotic stenosis in middle-aged and elderly Chinese. Sci Rep 7:7951. https://doi.org/10.1038/s41598-017-07811-7
Koloverou E, Panagiotakos DB, Kyrou I et al (2019) Visceral adiposity index outperforms common anthropometric indices in predicting 10-year diabetes risk: Results from the ATTICA study. Diabetes Metab Res Rev 35:e3161. https://doi.org/10.1002/dmrr.3161
Clemente G, Mancini M, Giacco R et al (2015) Visceral adiposity and subclinical atherosclerosis in healthy young men. Int J Food Sci Nutr 66:466–470. https://doi.org/10.3109/09637486.2015.1042845
Wei J, Liu X, Xue H et al (2019) Comparisons of visceral adiposity index, body shape index, body mass index and waist circumference and their associations with diabetes mellitus in adults. Nutrients. https://doi.org/10.3390/nu11071580
Nusrianto R, Ayundini G, Kristanti M et al (2019) Visceral adiposity index and lipid accumulation product as a predictor of type 2 diabetes mellitus: the Bogor cohort study of non-communicable diseases risk factors. Diabetes Res Clin Pract 155:107798. https://doi.org/10.1016/j.diabres.2019.107798
Xue Y, Shen Q, Li C et al (2020) The visceral adipose index in relation to incidence of hypertension in Chinese adults: China Health and Nutrition Survey (CHNS). Nutrients. https://doi.org/10.3390/nu12030805
Zhang Z, Shi D, Zhang Q et al (2018) Visceral adiposity index (VAI), a powerful predictor of incident hypertension in prehypertensives. Intern Emerg Med 13:509–516. https://doi.org/10.1007/s11739-018-1836-8
Yang F, Wang G, Wang Z et al (2014) Visceral adiposity index may be a surrogate marker for the assessment of the effects of obesity on arterial stiffness. PLoS ONE 9:e104365. https://doi.org/10.1371/journal.pone.0104365
Kouli GM, Panagiotakos DB, Kyrou I et al (2017) Visceral adiposity index and 10-year cardiovascular disease incidence: the ATTICA study. Nutr Metab Cardiovasc Dis 27:881–889. https://doi.org/10.1016/j.numecd.2017.06.015
Moebus S, Balijepalli C, Lösch C et al (2010) Age- and sex-specific prevalence and ten-year risk for cardiovascular disease of all 16 risk factor combinations of the metabolic syndrome—a cross-sectional study. Cardiovasc Diabetol 9:34. https://doi.org/10.1186/1475-2840-9-34
Ibrahim MM (2010) Subcutaneous and visceral adipose tissue: structural and functional differences. Obes Rev 11:11–18. https://doi.org/10.1111/j.1467-789X.2009.00623.x
Misra A, Vikram NK (2003) Clinical and pathophysiological consequences of abdominal adiposity and abdominal adipose tissue depots. Nutrition 19:457–466. https://doi.org/10.1016/s0899-9007(02)01003-1
Unamuno X, Gómez-Ambrosi J, Rodríguez A et al (2018) Adipokine dysregulation and adipose tissue inflammation in human obesity. Eur J Clin Invest 48:e12997. https://doi.org/10.1111/eci.12997
Oikonomou EK, Antoniades C (2019) The role of adipose tissue in cardiovascular health and disease. Nat Rev Cardiol 16:83–99. https://doi.org/10.1038/s41569-018-0097-6
Amato MC, Pizzolanti G, Torregrossa V et al (2014) Visceral adiposity index (VAI) is predictive of an altered adipokine profile in patients with type 2 diabetes. PLoS ONE 9:e91969. https://doi.org/10.1371/journal.pone.0091969
Katagiri H, Yamada T, Oka Y (2007) Adiposity and cardiovascular disorders: disturbance of the regulatory system consisting of humoral and neuronal signals. Circ Res 101:27–39. https://doi.org/10.1161/circresaha.107.151621
Figueroa AL, Takx RA, MacNabb MH et al (2016) Relationship between measures of adiposity, arterial inflammation, and subsequent cardiovascular events. Circ Cardiovasc Imaging 9:e004043. https://doi.org/10.1161/circimaging.115.004043
Scheja L, Heeren J (2019) The endocrine function of adipose tissues in health and cardiometabolic disease. Nat Rev Endocrinol 15:507–524. https://doi.org/10.1038/s41574-019-0230-6
Niccoli T, Partridge L (2012) Ageing as a risk factor for disease. Curr Biol 22:R741-752. https://doi.org/10.1016/j.cub.2012.07.024
Hou Y, Dan X, Babbar M et al (2019) Ageing as a risk factor for neurodegenerative disease. Nat Rev Neurol 15:565–581. https://doi.org/10.1038/s41582-019-0244-7
Tchernof A, Brochu D, Maltais-Payette I et al (2018) Androgens and the regulation of adiposity and body fat distribution in humans. Compr Physiol 8:1253–1290. https://doi.org/10.1002/cphy.c170009
Moreau KL (2018) Intersection between gonadal function and vascular aging in women. J Appl Physiol 1985:1881–1887. https://doi.org/10.1152/japplphysiol.00117.2018
Camell CD, Sander J, Spadaro O et al (2017) Inflammasome-driven catecholamine catabolism in macrophages blunts lipolysis during ageing. Nature 550:119–123. https://doi.org/10.1038/nature24022
Foster MT, Shi H, Seeley RJ et al (2011) Removal of intra-abdominal visceral adipose tissue improves glucose tolerance in rats: role of hepatic triglyceride storage. Physiol Behav 104:845–854. https://doi.org/10.1016/j.physbeh.2011.04.064
Muzumdar R, Allison DB, Huffman DM et al (2008) Visceral adipose tissue modulates mammalian longevity. Aging Cell 7:438–440. https://doi.org/10.1111/j.1474-9726.2008.00391.x
Skurk T, Alberti-Huber C, Herder C et al (2007) Relationship between adipocyte size and adipokine expression and secretion. J Clin Endocrinol Metab 92:1023–1033. https://doi.org/10.1210/jc.2006-1055
Yu YH, Zhu H (2004) Chronological changes in metabolism and functions of cultured adipocytes: a hypothesis for cell aging in mature adipocytes. Am J Physiol Endocrinol Metab 286:E402-410. https://doi.org/10.1152/ajpendo.00247.2003
Lin MT, Beal MF (2006) Mitochondrial dysfunction and oxidative stress in neurodegenerative diseases. Nature 443:787–795. https://doi.org/10.1038/nature05292
Khan S, Chan YT, Revelo XS et al (2020) The immune landscape of visceral adipose tissue during obesity and aging. Front Endocrinol (Lausanne) 11:267. https://doi.org/10.3389/fendo.2020.00267
Lumeng CN, Liu J, Geletka L et al (2011) Aging is associated with an increase in T cells and inflammatory macrophages in visceral adipose tissue. J Immunol 187:6208–6216. https://doi.org/10.4049/jimmunol.1102188
Lumeng CN, Bodzin JL, Saltiel AR (2007) Obesity induces a phenotypic switch in adipose tissue macrophage polarization. J Clin Invest 117:175–184. https://doi.org/10.1172/jci29881
Ferrucci L, Fabbri E (2018) Inflammageing: chronic inflammation in ageing, cardiovascular disease, and frailty. Nat Rev Cardiol 15:505–522. https://doi.org/10.1038/s41569-018-0064-2
Prattichizzo F, De Nigris V, Spiga R et al (2018) Inflammageing and metaflammation: The yin and yang of type 2 diabetes. Ageing Res Rev 41:1–17. https://doi.org/10.1016/j.arr.2017.10.003
Liu D, Richardson G, Benli FM et al (2020) Inflammageing in the cardiovascular system: mechanisms, emerging targets, and novel therapeutic strategies. Clin Sci (Lond) 134:2243–2262. https://doi.org/10.1042/cs20191213
Franceschi C, Garagnani P, Parini P et al (2018) Inflammaging: a new immune-metabolic viewpoint for age-related diseases. Nat Rev Endocrinol 14:576–590. https://doi.org/10.1038/s41574-018-0059-4
Barzilai N, Crandall JP, Kritchevsky SB et al (2016) Metformin as a tool to target aging. Cell Metab 23:1060–1065. https://doi.org/10.1016/j.cmet.2016.05.011
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
On behalf of all authors, the corresponding author states that there is no conflict of interest.
Statement of human and animal rights
The study involving human participants was reviewed and approved by the Centers for Disease Control and Prevention.
Informed consent
The patients/participants provided their written informed consent to participate in this study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Liu, W., Weng, S., Chen, Y. et al. Age-adjusted visceral adiposity index (VAI) is superior to VAI for predicting mortality among US adults: an analysis of the NHANES 2011–2014. Aging Clin Exp Res 36, 24 (2024). https://doi.org/10.1007/s40520-023-02660-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s40520-023-02660-z