Abstract
Purpose of Review
Hepatitis B (HBV) vaccinated patients have mixed responses with regard to antibody titers and subsequent level of immunity. This review aims to examine the diverse strategies employed by transplant centers for infection prevention when utilizing HBV-infected kidneys, including our own center’s practice.
Recent Findings
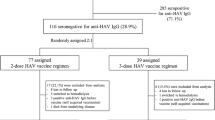
Transplant centers have implemented varied prophylaxis approaches based on recipients’ anti-HB titers for utilizing HBV-infected kidneys. We retrospectively reviewed ten recipients who received kidneys from HBV-positive donors at our center. Recipients with anti-HBs titers above 100 mIU/mL received entecavir prophylaxis, while those with lower titers received perioperative HBIG. Throughout the follow-up, all patients remained negative for HBV NAT and HBsAg. Six patients experienced asymptomatic anti-HBc seroconversion, of which two patients cleared anti-HBc within 1 year. One patient experienced a decline in anti-HBs titers below 100 mIU/mL but remained free of HBV infection.
Summary
The utilization of Hepatitis B-infected kidneys for transplantation in HBV-immunized recipients is safe. Asymptomatic seroconversion is frequent, but viremia is prevented by immunization and/or entecavir. The role of HBIG prophylaxis is unclear. Most patients with preoperative anti-HBs titer > 100 mIU/mL maintain those titers during the first-year post-transplant.
Similar content being viewed by others
Data Availability
Direct URL citations appear in the printed text. Supporting information can be found online in the supporting information section at the end of this article.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance
Lentine KL, Smith JM, Hart A, et al. OPTN/SRTR 2020 Annual data report: kidney. Am J Transplant. 2022;22(Suppl 2):21–136. https://doi.org/10.1111/ajt.16982.
Sise ME, Strohbehn IA, Bethea E, Gustafson JL, Chung RT. Balancing the risk and rewards of utilizing organs from Hepatitis C viremic donors. Curr Opin Organ Transplant. 2019Jun;24(3):351–7.
Cho JY, Sohn W, Sinn DH, Gwak GY, Paik YH, Choi MS, Kohl’s KC, Paik SW, Yoo BC, Lee JH. Long-term real-world entecavir therapy in treatment-naïve hepatitis B patients: baseline hepatitis B virus DNA and hepatitis B surface antigen levels predict virological response. Korean J Intern Med. 2017;32(4):636–46.
Ringelhan M, McKeating JA, Protzer U. Viral hepatitis and liver cancer. Philos Trans R Soc Lond B Biol Sci. 2017 Oct 19;372(1732):20160274. https://doi.org/10.1098/rstb.2016.0274. (Erratum.In:PhilosTransRSocLondBBiolSci.2018Jan5;373(1737)).
Zitt E, Hafner-Giessauf H, Wimmer B, et al. Response to active hepatitis B vaccination and mortality in incident dialysis patients. Vaccine. 2017;35(5):814–20. https://doi.org/10.1016/j.vaccine.2016.12.032.
• Huprikar S, Danziger-Isakov L, Ahn J, et al. Solid organ transplantation from hepatitis B virus-positive donors: consensus guidelines for recipient management. Am J Transplant. 2015;15(5):1162–72. https://doi.org/10.1111/ajt.13187. Provides a foundation for the transplant centers to develop HBV prophylaxis protocols when starting to utilize hepatitis B infected organs.
Tuncer M, Tekin S, Yücetin L, Şengül A, Demirbaş A. Hepatitis B surface antigen positivity is not a contraindication for living kidney donation. Transplant Proc. 2012;44(6):1628–9. https://doi.org/10.1016/j.transproceed.2012.04.015.
Jiang H, Wu J, Zhang X, et al. Kidney transplantation from hepatitis B surface antigen positive donors into hepatitis B surface antibody positive recipients: a prospective nonrandomized controlled study from a single center. Am J Transplant. 2009;9(8):1853–8. https://doi.org/10.1111/j.1600-6143.2009.02707.x.
Chancharoenthana W, Townamchai N, Pongpirul K, et al. The outcomes of kidney transplantation in hepatitis B surface antigen (HBsAg)-negative recipients receiving graft from HBsAg-positive donors: a retrospective, propensity score-matched study. Am J Transplant. 2014;14(12):2814–20. https://doi.org/10.1111/ajt.12921.
Wang XD, Liu JP, Song TR, et al. Kidney transplantation from HBsAg+ living donors to HBsAg- recipients: clinical outcomes at a high volume center in china. Clin Infect Dis. 2021;72:1016–23.
• Delman AM, Turner KM, Safdar K, Anwar N, Silski LS, Lee TC, Luckett K, Cuffy MC, Quillin RC, Schoech M, Kaiser TE, Govil A, Bari K, Shah SA. Expanding the donor pool: first use of hepatitis B virus NAT positive slid organ allografts into seronegative recipients. Annals of Surg. 2021;274(4):556–64. This is the largest series describing the transplantation of HBV NAT + kidney and liver allografts into HBV seronegative recipients.
Author information
Authors and Affiliations
Contributions
Authors S. M., A. R., and N. R. wrote the manuscript. All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Ethics Approval and Consent to Participate
This study was approved by Medical City Healthcare Institutional Review Board as part of Master Retrospective Protocol Medical City Outcomes Research (MCOR-01). Informed consent from patients was not obtained as this was a retrospective study using deidentified data.
Competing Interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Muqueet, S., Reddy, N.A., Curtis, A. et al. Outcomes of Entecavir Prophylaxis in Hepatitis B Immune Patients Receiving Hepatitis B Infected Kidneys: A Single Center Experience. Curr Transpl Rep 11, 15–19 (2024). https://doi.org/10.1007/s40472-023-00425-1
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40472-023-00425-1