Abstract
Purpose of Review
Kratom, a preparation of the leaves collected from the Southeast Asian plant Mitragyna speciosa, has increased in use within the United States (US) predominantly due to its stimulant and opioid-like effects. It contains many active alkaloids, most notably mitragynine. Clinical pharmacological research and toxicological information are limited, hindering forensic interpretation and an understanding of the role kratom use may play in death. Despite arguments from some vocal proponents and vendors that kratom poses no risk to users, there is a growing body of evidence that kratom use can result in significant adverse events, including death.
Recent Findings
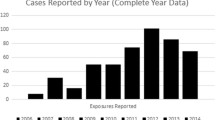
Toxicological data for blood specimens analyzed between January 2018 and September 2022 in postmortem and driving under the influence of drugs cases were reviewed for the presence of mitragynine, the primary alkaloid of Mitragyna speciosa. Reported blood mitragynine concentrations, compound positivity, and concomitant findings were evaluated.
Summary
The forensic interpretation of mitragynine continues to be challenging. Kratom has been implicated in an increasing number of overdoses and deaths, and its significance is difficult to ascertain due to a substantial number of confounding variables, including a limited scope of toxicological testing and frequent co-positivity with drugs of abuse. Mitragynine has been listed as the primary toxicological finding in several overdose deaths albeit at a lower frequency compared to overall positivity, particularly when present at elevated concentrations (> 1000 ng/mL); these cases provide forensic confirmation of harms due to kratom use.

Similar content being viewed by others
Data Availability
The data underlying this article will be shared on reasonable request to the corresponding author.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
• Han C, Schmitt J, Gilliland KM. DARK classics in chemical neuroscience: kratom. ACS Chem Neurosci. 2020;11(23):3870. https://doi.org/10.1021/acschemneuro.9b00535. This article is a good review on the chemical properties, pharmacology, and use of kratom.
Cinosi E, Martinotti G, Simonato P, Singh D, Demetrovics Z, Roman-Urrestarazu A, Bersani FS, Vicknasingam B, Piazzon G, Li JH, Yu WJ, Kapitány-Fövény M, Farkas J, Di Giannantonio M, Corazza O. Following “the roots” of kratom (Mitragyna speciosa): the evolution of an enhancer from a traditional use to increase work and productivity in Southeast Asia to a recreational psychoactive drug in Western countries. Biomed Res Int. 2015;2015:968786. https://doi.org/10.1155/2015/968786.
Eastlack SC, Cornett EM, Kaye AD. Kratom-pharmacology, clinical implications, and outlook: a comprehensive review. Pain Ther. 2020;9(1):55–69. https://doi.org/10.1007/s40122-020-00151-x.
Prozialeck WC, Lamar PC, Krupp M 2nd, Moon M, Phelps LE, Grundmann O. Kratom use within the context of the evolving opioid crisis and the COVID-19 pandemic in the United States. Front Pharmacol. 2021;26(12):729220. https://doi.org/10.3389/fphar.2021.729220.
Grundmann O. Patterns of kratom use and health impact in the US-results from an online survey. Drug Alcohol Depend. 2017;1(176):63–70. https://doi.org/10.1016/j.drugalcdep.2017.03.007.
Garcia-Romeu A, Cox DJ, Smith KE, Dunn KE, Griffiths RR. Kratom (Mitragyna speciosa): user demographics, use patterns, and implications for the opioid epidemic. Drug Alcohol Depend. 2020;1(208):107849.
Smith KE, Dunn KE, Rogers JM, Garcia-Romeu A, Strickland JC, Epstein DH. Assessment of kratom use disorder and withdrawal among an online convenience sample of US adults. J Addict Med. 2022;16(6):666–70.
Brown PN, Lund JA, Murch SJ. A botanical, phytochemical and ethnomedicinal review of the genus Mitragyna korth: implications for products sold as kratom. J Ethnopharmacol. 2017;18(202):302–25. https://doi.org/10.1016/j.jep.2017.03.020.
Sharma A, McCurdy CR. Assessing the therapeutic potential and toxicity of Mitragyna speciosa in opioid use disorder. Expert Opin Drug Metab Toxicol. 2021;17(3):255–7. https://doi.org/10.1080/17425255.2021.1853706.
•• Kruegel AC, Uprety R, Grinnell SG, Langreck C, Pekarskaya EA, Le Rouzic V, Ansonoff M, Gassaway MM, Pintar JE, Pasternak GW, Javitch JA, Majumdar S, Sames D. 7-Hydroxymitragynine is an active metabolite of mitragynine and a key mediator of its analgesic effects. ACS Cent Sci. 2019;5(6):992–1001. https://doi.org/10.1021/acscentsci.9b00141. Demonstrating that 7-hydroxymitragynine is a metabolite of mitragynine and furthers our understanding of kratom’s effects.
Kruegel AC, Grundmann O. The medicinal chemistry and neuropharmacology of kratom: a preliminary discussion of a promising medicinal plant and analysis of its potential for abuse. Neuropharmacology. 2018;134(Pt A):108–20. https://doi.org/10.1016/j.neuropharm.2017.08.026.
León F, Obeng S, Mottinelli M, Chen Y, King TI, Berthold EC, Kamble SH, Restrepo LF, Patel A, Gamez-Jimenez LR, Lopera-Londoño C, Hiranita T, Sharma A, Hampson AJ, Canal CE, McMahon LR, McCurdy CR. Activity of Mitragyna speciosa (“kratom”) alkaloids at serotonin receptors. J Med Chem. 2021;64(18):13510–23.
Obeng S, Kamble SH, Reeves ME, Restrepo LF, Patel A, Behnke M, Chear NJ, Ramanathan S, Sharma A, León F, Hiranita T, Avery BA, McMahon LR, McCurdy CR. Investigation of the adrenergic and opioid binding affinities, metabolic stability, plasma protein binding properties, and functional effects of selected indole-based kratom alkaloids. J Med Chem. 2020;63(1):433–9.
•• Kamble SH, León F, King TI, Berthold EC, Lopera-Londoño C, Siva Rama Raju K, Hampson AJ, Sharma A, Avery BA, McMahon LR, McCurdy CR. Metabolism of a kratom alkaloid metabolite in human plasma increases its opioid potency and efficacy. ACS Pharmacol Transl Sci. 2020;3(6):1063–8. https://doi.org/10.1021/acsptsci.0c00075. This research of a mitragynine metabolite that is a potent MOR agonist could help explain kratom’s pharmacology and psychoactive properties.
• Váradi A, Marrone GF, Palmer TC, Narayan A, Szabó MR, Le Rouzic V, Grinnell SG, Subrath JJ, Warner E, Kalra S, Hunkele A, Pagirsky J, Eans SO, Medina JM, Xu J, Pan YX, Borics A, Pasternak GW, McLaughlin JP, Majumdar S. Mitragynine/corynantheidine pseudoindoxyls as opioid analgesics with Mu agonism and delta antagonism, which do not recruit β-arrestin-2. J Med Chem. 2016;59(18):8381–97. https://doi.org/10.1021/acs.jmedchem.6b00748. An important paper on the MOR pharmacology of Mitragyna alkaloids.
Wade P. Bentuangie Kratom Strains & Their Effects [Internet]. Kratom.org. 2022. [cited 29 November 2022] Available from: kratom.org/strains/bentuangie
Eggleston W, Stoppacher R, Suen K, Marraffa JM, Nelson LS. Kratom use and toxicities in the United States. Pharmacotherapy. 2019;39(7):775–7. https://doi.org/10.1002/phar.2280.
Leong Bin Abdullah MFI, Singh D. The adverse cardiovascular effects and cardiotoxicity of kratom (Mitragyna speciosa Korth.): a comprehensive review. Front Pharmacol. 2021;27(12):726003. https://doi.org/10.3389/fphar.2021.726003.
Stringer J, Welsh C, Tommasello A. Methadone-associated Q-T interval prolongation and torsades de pointes. Am J Health Syst Pharm. 2009;66(9):825–33. https://doi.org/10.2146/ajhp070392.
Smith KE, Lawson T. Prevalence and motivations for kratom use in a specimen of substance users enrolled in a residential treatment program. Drug Alcohol Depend. 2017 Nov;1(180):340–8. https://doi.org/10.1016/j.drugalcdep.2017.08.034.
Weiss ST, Douglas HE. Treatment of kratom withdrawal and dependence with buprenorphine/naloxone: a case series and systematic literature review. J Addict Med. 2021;15(2):167–72. https://doi.org/10.1097/ADM.0000000000000721.
Broyan VR, Brar JK, Allgaier Student T, Allgaier JT. Long-term buprenorphine treatment for kratom use disorder: a case series. Subst Abus. 2022;43(1):763–6.
Smith KE, Dunn KE, Epstein DH, Feldman JD, Garcia-Romeu A, Grundmann O, Henningfield JE, McCurdy CR, Rogers JM, Schriefer D, Singh D, Weiss ST. Need for clarity and context in case reports on kratom use, assessment, and intervention. Subst Abus. 2022;43(1):1221–4.
•• Papsun DM, Chan-Hosokawa A, Friederich L, Brower J, Graf K, Logan B. The trouble with kratom: analytical and interpretative issues involving mitragynine. J Anal Toxicol. 2019;43(8):615–29. https://doi.org/10.1093/jat/bkz064. This paper constitutes the largest dataset of mitragynine in forensic toxicology casework.
Bourgine J, Garnier-Jardin C, Chrétien B, Le Boisselier R, Loilier M, Lelong-Boulouard V, et al. Fatal intoxication with kratom: a case report. Toxicologie Analytique et Clin. 2019;31:S36–7.
• Wang C, Walker AE. Fatal mitragynine-associated toxicity in Canada: a case report and review of the literature. Acad Forensic Pathology. 2019;8:340–6. Case report with elevated mitragynine blood concentration and mitragynine is primarily implicated
• Matson M, Schenk N. Fatality of 33-year-old man involving kratom toxicity. J Forensic Sci. 2019;64:1933–5. Case report with elevated mitragynine blood concentration and mitragynine is primarily implicated
• Mata DC, Andera KM. Case series: mitragynine blood and tissue concentrations in fatalities from 2017 to 2018 in Orange County, CA, USA. Forensic. Chemistry. 2020;17:100205. Case series of cases involving mitragynine with more detail
•• Gershman K, Timm K, Frank M, Lampi L, Melamed J, Gerona R, et al. Deaths in Colorado attributed to kratom. New England J Med. 2019;380:97–8. Case series of cases involving mitragynine with more detail
• Behonick GS, Vu C, Czarnecki L, El-Ters M, Shanks KG. Two single-drug fatal intoxications by mitragynine. J Anal Toxicol. 2022;46(5):e110–4. https://doi.org/10.1093/jat/bkac016. Case report with elevated mitragynine blood concentration and mitragynine is listed in COD
• Trakulsrichai S, Sathirakul K, Auparakkitanon S, Krongvorakul J, Sueajai J, Noumjad N, et al. Pharmacokinetics of mitragynine in man. Drug Des, Dev Ther. 2015;9:2421–9. An important paper on one of the few pharmacokinetic studies of kratom use in humans
Grundmann O. Patterns of kratom use and health impact in the US-results from an online survey. Drug Alcohol Depend. 2017;1(176):63–70.
• Tanna RS, Nguyen JT, Hadi DL, Manwill PK, Flores-Bocanegra L, Layton ME, et al. Clinical pharmacokinetic assessment of Kratom (Mitragyna Speciosa), a botanical product with opioid-like effects, in healthy adult participants. Pharmaceutics. 2022;14:620. An important paper on one of the few pharmacokinetic studies of kratom use in humans
• Chadchoy P, Sinchai T. The relationship between Mitragynine blood concentrations and death in Thailand. Interdiscip Res Rev. 2020;15:18–21. An important paper reporting blood mitragynine concentrations in non-pathological causes of death
Brower J. Mitragynine-only deaths in North Carolina. In: Society of Forensic Toxicologists Annual Conference. Society of Forensic Toxicologists; 2022.
Karinen R, Fosen JT, Rodge S, Vindenes V. An accidental poisoning with mitragynine. Forensic Sci Int. 2014;245:e29–232.
O’Malley Olsen E, O’Donnell J, Mattson CL, Schier JG, Wilson N. Unintentional drug overdose deaths with kratom detected – 27 states, July 2016-December 2017. Morbid Mortal Weekly Rep. 2019;68(14):326–7.
•• Schmitt J, Bingham K, Knight L. Kratom-associated fatalities in northern Nevada – what mitragynine level is fatal? Am J Forensic Med Pathol. 2021;42(4):341–9. Case series of cases involving mitragynine with more detail
Basiliere S, Kerrigan S. Temperature and pH-dependent stability of mitragyna alkaloids. J Anal Toxicol. 2020;44:314–24. https://doi.org/10.1093/jat/bkz103.
Basiliere S, Brower J, Winecker R, Friederich L, Kerrigan S. Identification of five mitragyna alkaloids in blood and tissues using liquid chromatography-quadrupole/time-of-flight mass spectrometry. Forensic Toxicol. 2020;38:420–35. https://doi.org/10.1007/s11419-020-00537-8.
Nacca N, Schult RF, Li L, Spink DC, Ginsberg G, Navarette K, et al. Kratom adulterated with phenylethylamine and associated intracerebral hemorrhage: linking toxicologists and public health officials to identify dangerous adulterants. J Med Toxicol: Official J Am College Med Toxicol. 2020;16:71–4.
Hoonwijit U, Waithum K, Tansrisawad N. Comparison of mitragynine stability in human blood in common blood collection tubes. Chulalongkorn Med J. 2020;64:439447.
Takayama H. Chemistry and pharmacology of analgesic indole alkaloids from the rubiaceous plant, mitragyna speciosa. Chem Pharm Bull. 2004;52(8):916–28.
Hanapi NA, Chear NJY, Azizi J, Yusof SR. Kratom alkaloids: interactions with enzymes. Front Pharmacol. 2021;17(12):751656.
Henningfield JE, Rodricks JV, Manguson AM, Huestis MA. Respiratory effects of oral mitragynine and oxycodone in a rodent model. Psychopharmacology. 2022;239(12):3793–804.
Kapp F, Maurer H, Auwärter V, Winkemann M, Hermanns-Clausen M. Intrahepatic cholestasis following abuse of powdered kratom (mitragyna speciosa). J Med Toxicol. 2011;7:227–31.
Nelsen JL, Lapoint J, Hodgman MJ. Seizure and coma following kratom (mitragynine speciosa korth) exposure. J Med Toxicol. 2020;6:424–6.
Dorman C, Wong M, Khan A. Cholestatic hepatitis from prolonged kratom use: a case report. Hepatology. 2015;61(3):1086–7.
Tayabeli K, Bolzon C, Foster P, Patel J, Kalim MO. Kratom: a dangerous player in the opioid crisis. J Community Hosp Intern Med Perspect. 2018;8(3):107–10.
Afzal H, Esang M, Rahman S. A case of kratom-induced seizures. Cureus. 2020;12:e6588.
Ahmad J, Odin JA, Hayashi PH, Fontana RJ, Conjeevaram H, Avula B, et al. Liver injury associated with kratom, a popular opioid-like product: experience from the U.S. drug induced liver injury network and a review of the literature. Drug Alcohol Depend. 2021;1(218):108426. https://doi.org/10.1016/j.drugalcdep.2020.108426.
Schimmel J, Dart RC. Kratom (Mitragyna Speciosa) liver injury: a comprehensive review. Drugs. 2020;80:263–83.
Singh D, Narayanan S, Müller CP, Swogger MT, Rahim AA, Leong Bin Abdullah MFI, et al. Severity of kratom (Mitragyna speciosa Korth.) psychological withdrawal symptoms. J Psychoact Drugs. 2018;50:445–50.
Overbeek DL, Abraham J, Munzer BW. Kratom (Mitragynine) ingestion requiring naloxone reversal. Clin Pract Cases Emerg Med. 2019;3:24–6.
Stanciu CN, Gnanasegaram SA, Ahmed S, Penders T. Kratom withdrawal: a systematic review with case series. J Psychoact Drugs. 2019;51:12–8.
Assangkornchai S, Muekthong A, Sam-Angsri N, Pattanasttayawong U. The use of mitragynine speciosa (“krathom”), an addictive plant in Thailand. Subst Use Misuse. 2007;24(14):2145–57.
McWhirter L, Morris S. A case report of inpatient detoxification after kratom (mitragyna speciosa) dependence. Eur Addict Res. 2010;16(4):229–31.
Cumpston KL, Carter M, Wills BK. Clinical outcomes after Kratom exposures: a poison center case series. Am J Emerg Med. 2018;36:166–8.
Post S, Spiller HA, Chounthirath T, Smith GA. Kratom exposures reported to United States poison control centers: 2011-2017. Clin Toxicol (Phil). 2019;57:847–54.
•• Corkery JM, Streete P, Claridge H, Goodair C, Papanti D, Orsolini L, et al. Characteristics of deaths associated with kratom use. J Psychopharmacol (Oxford, England). 2019;33:1102–23. [High level review of mitragynine involvement in fatalities]
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare no competing interests.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Papsun, D., Schroeder, W., Brower, J. et al. Forensic Implications of Kratom: Kratom Toxicity, Correlation with Mitragynine Concentrations, and Polypharmacy. Curr Addict Rep 10, 272–281 (2023). https://doi.org/10.1007/s40429-023-00477-4
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40429-023-00477-4