Abstract
Background
Information on drug safety in different ethnic populations reported in public documents such as the European Public Assessment Reports (EPARs), European Summary of Product Characteristics (SmPCs) or Singapore Package Inserts (SGPIs) generally appears limited.
Objective
This study aimed to clarify the extent of drug safety data in ethnic populations that is available in drug registration dossiers used for registration in the European Union (EU) and Singapore, and how much of this information is then included in the EPARs and SmPCs or SGPIs.
Methods
For this purpose, drug registration dossiers and these public documents for a selection of 25 drugs authorized both in the EU and Singapore were compared (note, the number of available full registration dossiers was only 24 due to a technical issue).
Results
Detailed safety data in ethnic groups were present in 23/24 (96%) of the drug registration dossiers, but was only present in 12/25 (48%) of the EPARs, 8/25 (32%) of the SmPCs, and 9/25 (36%) of the SGPIs. Furthermore, in many cases where ethnicity-specific safety information was provided in the SmPC or SGPIs, details on the ethnic subpopulations was not provided.
Conclusions
Despite the fact that safety data analyzed with respect to ethnic populations are available in almost all screened registration dossiers, this information is often unknown to patients or prescribers as it was often not included in the EPARs, EU SmPCs or SGPIs. In order to increase the availability of such potentially important safety information, it is recommended to at least provide ethnic populations and group size in these public documents. In this way, trust in the registered drugs in different ethnic populations may be increased, and more robust treatment decisions may be obtained in clinical practice.
Similar content being viewed by others
Ethnicity-specific drug safety data were present in 96% of registration dossiers of new chemical entities examined in this study, yet ethnicity-specific safety information was present in only 48% of the European Public Assessment Reports (EPARs), 32% of the European Union Summaries of Product Characteristics (SmPCs) and 36% of the Singapore Package Inserts (SGPIs). |
National regulatory authorities in non-European regions that reference European Medicines Agency (EMA) public documents may therefore be unaware of safety data for specific groups that may be pertinent to ethnic populations in their countries. |
Ethnicity-specific safety information for a drug often remains unknown to prescribers because translation from dossiers towards EPARs and SmPCs/SGPIs is incomplete. |
It is recommended that public documents from EMA assessments include specific information on ethnic populations and group sizes in clinical trials to increase transparency of the totality of evidence available on authorized drugs. |
1 Introduction
One of the responsibilities of drug regulatory authorities is to govern the safe use of medicines. Both in the US and many countries in Europe, the regulatory development of drug regulation and pharmacovigilance was fuelled by safety-related disasters, i.e. the sulfanilamide incident in 1937 in the US and the thalidomide incident in the early 1960s in Europe [1, 2]. The safety review and monitoring systems established have enabled drug regulatory agencies to manage safety events. For example, the thalidomide crisis was prevented in the US due to the safety review process of the US FDA where the drug was not approved due to insufficient data on the safety and effectiveness of the drug [3, 4]. Since their establishment, regulatory authorities such as the FDA and the European Medicines Agency (EMA) have strengthened their drug assessment processes to ensure the efficacy, safety and quality of drugs available to their populations [5,6,7,8]. Predicting drug behavior in ethnic/racial populations is gaining importance due to increased globalization of both drug development and access to medicine. Furthermore, pharmaceutical regulation is moving toward global convergence, and many smaller national regulatory authorities take reference from publicly available assessment reports from well-regarded medicine registration authorities to facilitate the approval process and expedite access to innovative medicines in their countries [9]. Of note, in this paper the term ‘ethnicity’ will be used in order to classify different origins, a term that is considered broader and considered to encompass the term ‘race’.
Over the last decade, it has become increasingly clear that safety can be variable in different ethnic populations. For example, in the case of carbamazepine, which is indicated for the treatment of epilepsy, bipolar disorder and trigeminal neuralgia, very rare but severe skin reactions such as Stevens–Johnson syndrome (SJS) and toxic epidermal necrolysis (TEN) have a higher incidence in South-East Asian populations compared with Caucasian/White populations (in fact pointing at the same population, with the term Caucasian generally more often used in the European Union [EU] region and the term Whites more often used in the US region) [10,11,12,13,14]. Patients carrying the HLA-B*1502 allele have a significantly higher risk of developing SJS/TEN, and this allele is more prevalent in certain Asian subpopulations, such as Han Chinese (1.9–12.4%), Thai (≈ 7.5%), Malay (≈ 8%) and Indian (2–6%), partially accounting for the increased incidence of carbamazepine-induced SJS/TEN in these ethnic populations [15,16,17]. Likewise, allopurinol was associated with causing severe cutaneous adverse reactions (SCAR) [18]. In this case, the allele variant HLA-B*5801 was related to the risk of SCAR, and, also in this case, the allele is more commonly found in East Asian subpopulations [16, 19]. Another example of ethnicity differences is the lower dose of warfarin required in Singapore Chinese compared with Singapore Indians to achieve the optimal therapeutic range for balancing bleeding risk with risk of a recurrent thromboembolic event; the difference in doses between these ethnic groups is explained in large part by the different distributions of the VKORC1 and CYP2C9 genotypes in the two ethnic populations [20].
These examples illustrate that different ethnic populations may react differently to drugs and that the prevalence of different adverse events (AEs) in different ethnic populations can be a clue to a potential genetic association. In this light, it is understandable that pharmaceutical companies would generally analyse and compare AEs in different ethnic populations included in clinical trials in support of registration of a medicinal product [21]. Such safety information in ethnic groups is included in the benefit–risk evaluation before drug marketing authorization (MA) can be granted. In the EU, as a matter of transparency, relevant outcomes of such evaluations are summarized in public documents such as the European Public Assessment Report (EPAR) and in the Summary of Product Characteristics (SmPC), both of which can be accessed on the EMA website by patients and health care professionals [22]. Likewise, in Singapore, the approved package inserts (SGPIs) can also be accessed by patients and health care professionals on the website of the Health Sciences Authority (HSA), the Singapore drug regulatory agency.
Since the EU population mainly consists of Caucasians, historically, patients with Caucasian background often form the majority of the patients included in the clinical trials supporting drug registration in the EU. However, increased globalization has led to the situation that more non-Caucasian people live in Europe and that more value needs to be given in the EU to safety information in other ethnic populations. In Singapore, the Singapore population mainly consists of three non-Caucasian ethnicities (≈ 75% Chinese, ≈ 14% Malay and ≈ 9% Indian). The HSA takes reference from the ICH E5 Guideline (Ethnic Factors in the Acceptability of Foreign Clinical Data) and accepts the use of foreign clinical data in regulatory submissions supporting drug registration. Hence, the clinical dossier submitted to the HSA is mostly the same as that submitted to major regulatory agencies, such as the EMA and FDA, and the foreign clinical data are assessed if it can be extrapolated to the Singapore population [23]. In this light, it is considered very valuable to include the detailed breakdown of the ethnic background and group size of the patients in the clinical studies (i.e. breakdown of the various patient populations for the pharmacokinetic/pharmacodynamic studies, efficacy endpoints, safety endpoints, and even AEs that occurred in the studies) in the dossiers to facilitate regulatory reviews. Furthermore, summaries of such information should also be included in public documents, such as the EPAR, EU SmPC and SGPI. This will allow prescribers and patients to be able to better interpret the clinical efficacy and safety results in the relevant ethnic populations.
When we undertook this study, it was not completely clear how and where ethnicity-related drug safety data from clinical studies are documented and assessed in registration applications in the EU and Singapore, and how much of this information is subsequently included in the EPAR and/or EU SmPC or SGPI. For this purpose, we have addressed the following research questions for each selected drug in this study. Are ethnicity data on subjects included in the clinical studies generally provided by the company? Are drug safety data according to ethnic group subsequently presented in registration dossiers and public EU and Singapore product information documents? If so, what is the level of detail regarding ethnicity characteristics for the drug safety data in the registration file? Finally, how much of the information provided in the registration dossier is subsequently included in the EPAR and SmPC/SGPI?
2 Methods
2.1 Drug Selection
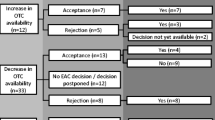
In selecting drugs for our review in February 2018, the final aim was to examine new chemical entities with large-scale clinical studies that were registered in both the EU and Singapore (Fig. 1). First, all medicinal products registered via the Centralised Procedure (CP) at the EMA between January 2008 and December 2012 were retrieved from the EMA website. Generic drugs, biosimilars and fixed-dose combination drugs were excluded in this search, since, for such products, limited or no new clinical efficacy and safety studies are available. The search yielded 204 drugs in the EU, of which 75 were also registered in Singapore.
Subsequently, drugs with conditional approval or approved under exceptional circumstances, drugs for pediatric use and orphan drugs at the EMA were excluded due to the smaller number of patients included in clinical studies. This selection yielded 57 drugs. From these 57 drugs, we focused on drugs used in diabetes (Anatomical Therapeutic Chemical [ATC] code A10), antithrombotic agents (ATC code B01), drugs for cardiac therapy (ATC code C01), sex hormones and modulators of the genital system (ATC code G03), antivirals for systemic use (ATC code J05), antiepileptics (ATC code N03), psycholeptics (ATC code N05) and psychoanaleptics (ATC code N06) because the clinical study sizes of these types of products are generally larger, potentially increasing the chance of finding relevant safety data for such products. This selection yielded 22 drugs.
Subsequently, three antidiabetic drugs, of specific interest for drug safety in Singapore, were added to the study, i.e. sitagliptin, canagliflozin and empagliflozin. These three drugs were authorized in the EU in 2007, 2013 and 2014, respectively, but were not captured in our initial search algorithm because they were not approved in the predefined time period for drug selection (2008–2012). The final selection thus consisted of 25 drugs, which are listed in Table 1. Of note, in this paper, a drug containing the same active substance registered under a different name but on the basis of the same dossier is considered to be the same drug.
2.2 Data Collection for Ethnicity-Linked Safety Data
For each drug in the final selected set, registration dossiers were retrieved at the Dutch Medicines Evaluation Board. In the registration dossiers, investigation focussed on the Summary of Clinical Safety (module 2.7.4 of the registration dossier) and the individual clinical study reports (module 5.3 of the registration dossier). As employees of the Dutch Medicines Evaluation Board, authors AT, YY and MM have access to the EMA registration files. Furthermore, EPARs and SmPCs were retrieved from the EMA public website, and Singapore SGPIs were retrieved from the HSA database in Singapore.
Safety data were collected from all documents by systemic text search using all of the following keywords: ‘safety’, ‘ethnicity’, ‘race’, ‘population’, ‘Asian’ or ‘update’, and reading and evaluating the text search results by reading the surrounding text, titles and figures. Pharmacogenomic data were identified using the keywords ‘gene’, ‘genetic’ and ‘genomic’. Documents were also manually reviewed on graphs/plots and certain document parts, such as parts containing information regarding special populations, benefit–risks and conclusions/summary of safety. The following study details (i.e. exact information and its location) were reported for each selected drug: category of the studies (e.g. safety trials), size and type of the patient populations, number of reported AEs per ethnic group, and information on genetics if possibly relevant for safety.
Furthermore, AEs, AE rates and types, risks and undesirable effects from registration dossiers, EPARs, SmPCs and SGPIs were scored per ethnicity group. All ethnic populations were taken into account during analysis for the relationship with safety data. AEs were categorized according to the level of ethnic information available. If AEs occurred in specific ethnic populations, this information was categorized under Specified Ethnic Population. For instance, this could be text such as: “The Caucasian race did not affect safety aspects of the drug”. Next to this, if only ‘race’ or ‘ethnicity’ was acknowledged, such as: “Race had no clinically meaningful effect on the safety profile”, these data were classified as Unspecified Ethnic Population. Lastly, if ethnicity was not addressed at all, this was described as Ethnicity Data Unavailable. Data from registration dossiers, EPARs and SmPCs/SGPIs were compared.
3 Results
3.1 Ethnicity Data in Registration Dossiers, European Public Assessment Reports and Summary of Product Characteristics (SmPCs)
In total, 25 SmPCs and 25 EPARs were evaluated; the number of available full-registration dossiers was only 24, due to a technical issue. As graphically shown in Fig. 2, general safety data related to ethnicity were found in 23/24 (96%) dossiers, in 17/25 (68%) EPARs, and in 10/25 (40%) SmPCs and SGPIs. Safety data were specified per ethnic group in 23/24 (96%) registration dossiers, 12/25 (48%) EPARs, 8/25 (32%) SmPCs, and 9/25 (36%) SGPIs.
Available ethnicity-specified safety data in registration dossiers, EPARs, SmPCs and SGPIs. A distinction is made between the following situations: specified ethnic population mentioned (ethnic data per population, e.g. Caucasian, Asian, Black); unspecified ethnic population mentioned (only mentioning ‘race’ or ‘ethnicity’), or ethnicity information unavailable. SGPI Singapore Package Insert, SmPC Summary of Product Characteristics, EPAR European Public Assessment Report
The analysis showed that a substantial number of SmPCs and SGPIs (15/25, 60%) and EPARs (8/25, 32%) lacked ethnicity information related to safety, despite the fact that such data were present in the 24 available registration dossiers.
3.2 Safety Data Specified for Racial/Ethnic Populations
The number of dossiers, EPARs and SmPCs containing safety data related to Caucasian and Asian populations are depicted in Table 2. In general, specific ethnic information was more often included for Caucasians (23/24, 96%) compared with Asians (20/24, 83%) in the dossiers, which can partly be explained by a lack of detailed ethnic analysis in the registration dossier, whereas, in a few cases, clinical studies in registration dossiers did not include Asian patients. Overall, safety specified for Caucasian or Asian ethnicity was less often mentioned in the SmPCs (6/25 [24%] and 8/25 [32%], respectively) and SGPIs (6/25 [24%] and 5/25 [20%], respectively), compared with the dossiers. The table also lists the availability of safety information for Blacks/African Americans and Hispanics, which we also collected as these documents were reviewed. Also for these ethic groups, safety data related to ethnicity were included in the majority of dossiers, however were less frequently reported in EPARs, SmPCs or SGPIs.
3.3 Level of Detail Regarding Ethnicity in Drug Dossiers
The level of detail regarding ethnic populations in relation to safety data in the investigated documents was also analyzed. The ethnic groups mostly reported in the registration dossiers were Whites/Caucasians (23/24, 96%), Blacks/African Americans (22/24, 92%), Asians (20/24, 83%) and Hispanic (15/24, 63%) [Fig. 3]. In 16/24 registration dossiers (67%), the term ‘Others’ was used to indicate ethnicities not belonging to the four major groups that were specified. Although ethnicity related to safety was less frequently mentioned in the EPARs, SmPCs and SGPIs compared with the registration dossiers (see Fig. 3), the same ethnic groups were mostly reported in these documents.
Most prevalent safety data for ethnic groups in SGPIs, SmPCs, EPARs and dossiers. Note: ‘Asian (unspecified)’ covers all Asian races as no distinction was made between the different Asian subpopulations. SGPI Singapore Package Insert, SmPC Summary of Product Characteristics, EPAR European Public Assessment Report
Next to these four major ethnicities, smaller ethnic groups were also identified or grouped in all investigated registration dossiers, such as Pacific Islander (3/24, 13%), Alaskan Native (1/24, 4%), Hawaiian Native (1/24, 4%), non-Hispanic (10/24, 42%), non-Caucasian (2/24, 8%), non-Black (1/24, 4%) and non-Indian (1/24, 4%).
Further analysis was performed on the description of safety data related to particular Asian ethnicities in the dossiers, EPARs, SmPCs and SGPIs. In some registration dossiers, a distinction in Asian race was made with defined Asian subpopulations reported in the investigated documentation. Specific safety data relevant for the major ethnic groups in Singapore, i.e. Chinese, Indian and Malay, were seldom present in the screened documents. Specific safety data in the Indian population were found in 3/24 (12%) dossiers and 1/25 (4%) EPARs and SmPCs, but were not found in the SGPIs, while safety information in the Chinese population was mentioned in 1/24 (4%) dossiers and 2/25 (8%) EPARs, SmPCs and SGPIs.
Some of the dossiers used alternative ethnic groupings, such as Oriental (3/24, 13%), Japanese (2/24, 8%) or Korean (1/24, 4%), for the Asian ethnicities. These specific Asian ethnicities were not mentioned in any of the EPARs or SmPCs.
3.4 Wording of Ethnicity-Specified Data in the SmPC and Singapore Package Insert
Closer examination of the ethnicity-specified safety information provided in the SmPC yielded some differences in the way information was presented and how useful the information was to patients and prescribers, e.g. only a very general statement on the effect of race is provided in section 5.2 of the SmPC, summarizing pharmacokinetic information of a drug, for sitagliptin (brand name Januvia®) (SmPC Januvia) [24]. In this section, the following is stated: “No dose adjustment is necessary based on gender, race, or body mass index (BMI). These characteristics had no clinically meaningful effect on the pharmacokinetics of sitagliptin based on a composite analysis of Phase I pharmacokinetic data and on a population pharmacokinetic analysis of Phase I and Phase II data.”
This information does not allow prescribers to understand which races or population sizes were evaluated in the pharmacokinetic analysis of this drug, although the dose adjustment was considered not necessary. However, it was noted that details on the ethnicity of the patients (i.e. White, Black, Hispanic, Asian and Other) was available in the sitagliptin phase 3 studies in the dossier. This finding clearly indicates that ethnicity-related information was lost in translation from the dossier to the SmPC.
Of note, in contrast to the situation in the SmPC, in the SGPI for sitagliptin (Januvia®) [25], the abovementioned ethnic background of patients was included: “No dosage adjustment is necessary based on race. Race had no clinically meaningful effect on the pharmacokinetics of sitagliptin based on a composite analysis of available pharmacokinetic data, including subjects of white, Hispanic, black, Asian, and other racial groups.”
Likewise, information related to ethnicity was provided in a more elaborate fashion in the SmPC of linagliptin (Trajenta®) [SmPC Trajenta] [26]. In the pharmacokinetic section (Section 5.2) of the SmPC, the following information is provided: “No dosage adjustment is necessary based on race. Race had no obvious effect on the plasma concentrations of linagliptin based on a composite analysis of available pharmacokinetic data, including patients of Caucasian, Hispanic, African, and Asian origin. In addition the pharmacokinetic characteristics of linagliptin were found to be similar in dedicated phase I studies in Japanese, Chinese and Caucasian healthy volunteers.”
In the SGPI for dapagliflozin (Forxiga®) [27], even more elaborate and adequate information is provided on the ethnic background of patients, including the numbers per group: “No dosage adjustment from the dapagliflozin dose of 10 mg once daily is recommended on the basis of race. Race (White, Black, or Asian) was evaluated as a covariate in a population pharmacokinetic model using data from healthy subject and patient studies. Differences in systemic exposures between these races were small. Compared to Whites (n = 1147), Asian subjects (n = 47) had no difference in estimated mean dapagliflozin systemic exposures (90% CI range; 3.7% lower, 1% higher). Compared to Whites, Black subjects (n = 43) had 4.9% lower estimated mean dapagliflozin systemic exposures (90% CI range; 7.7% lower, 3.7% lower).”
This information would appear more useful to inform patients and prescribers on the specific ethnic groups that had been studied, which lead to the conclusion that no dosage adjustment is necessary based on race.
4 Discussion
The results of this investigation show that from the initial registration dossiers, having great detail and granular information on ethnicity-specified safety information, to the high-level summary and evaluation on product characteristics in the SmPC or SGPI, a sharp decline of reported safety data specified per population was found, with such data available in 23/24 (96%) registration dossiers and 8/25 (32%) SmPCs and SGPIs. In two additional SmPCs, ethnicity was mentioned in an unspecific manner (i.e. ‘safety was not different between different races’), adding up to 10/25 SmPCs where at least some information on ethnicity-specified safety was provided. However, in the majority of SmPCs and SGPIs, safety information was not specified for different ethnic populations. In general, it was observed that the amount of information on ethnicity-specified information in EPARs was in between that in registration dossiers and SmPCs and SGPIs, i.e. ethnicity-specified safety information given in 12/25 (48%) and in an unspecified manner in 5/25 (20%) EPARs.
Our findings are indicative of a suboptimal translation of safety data from registration dossiers to product information documents after registration. This can be partly explained by the fact that sometimes no relevant differences were observed in safety between different ethnic populations, or by the lack of power to come to robust conclusions in this respect, potentially reducing the chance of mentioning such data in the public documents (i.e. EPAR, SmPCs and SGPIs).
Although the omission of ethnicity-related safety information when clinically relevant differences exist is obviously not acceptable, also in case no clinically relevant differences appear to exist, not mentioning such data clearly is not a desirable situation, e.g. due to the increased globalization and diversity of ethnic populations in Europe for which potentially relevant safety information is now often not publicly available. Furthermore, several examples have arisen where drug response is different between different racial or ethnic populations, e.g. for carbamazepine, allopurinol and warfarin, as mentioned above, as well as other drugs such as rosuvastatin and abacavir [20, 28, 29]. For these drugs, an increased risk of adverse reactions and/or adjustments to doses are recommended for specific racial or ethnic groups or genetic variants whose incidence varies across ethnic groups [16, 28,29,30,31]. With increasing globalization in drug development, and to minimize duplication of clinical studies in different regions, there is a need for many regulatory agencies to consider the acceptance of foreign clinical data to support drug registration. In this light, it is important to acknowledge that in certain parts of the world, registration of new drugs is mainly based on assessment reports from other regions, not on the actual dossier. Hence, in these situations, efficacy and safety information specified for the different ethnic populations in the assessment reports (and consequently in EPARs) would greatly facilitate regulatory reviews. In this respect, even the notion that only a small number of certain ethnicities were included in clinical trials to provide safety information with these ethnic populations would be of relevance for review and possibly for clinical practice. In this study, although we found that 83% of the registration dossiers contained data on Asian populations, it is unfortunate that only a minority of the public documents mention the different ethnic populations included in the trials, which is a serious loss of information translation.
It should be acknowledged that the Asian ‘race’ often refers to more than 40 different ethnic populations, such as ‘Chinese’, ‘Japanese’, ‘Korean’ or ‘Indian’. Interestingly, South Asians are often grouped together with East Asians under ‘Asian’ race, yet South Asians are genetically closer to Europeans than they are to East Asians [32]. Hence, grouping populations by continent rather than genetic proximity may obscure potential signals of ethnic differences in drug response.
With respect to the wording regarding ethnic background of the subjects included in clinical studies, it is apparent that this is not always expressed in the same way for every drug in the SmPC, with examples mentioning nothing on ethnic background in case no relevant difference was apparent from the clinical registration studies, to examples where the different ethnic backgrounds included in the clinical registration package were provided. The lack of translation of safety data in subpopulations from the dossier to the SmPC and EPAR may be due to a lack of clinical relevance, e.g. due to the fact that AEs were not significantly increased in different ethnic subpopulations, or that the different ethnic groups were too small to be able to draw valid conclusions. In this respect, it is acknowledged that the SmPC is intended to be a legal document providing essential drug characteristics to the public. Indeed, as indicated in a study by Ramamoorthy et al. [33], approximately one-fifth of the new drugs approved in the US between 2009 and 2013 demonstrated differences in exposure and/or response between different ethnic groups, and this information was therefore included in the product label. Although this rationale could be understood, a too-strict summarization of the data, i.e. not mentioning safety data per ethnic population in the product information in case no clinical relevant difference was observed, hides the complete picture on ethnicity and safety in both SmPC and EPARs, and may hinder selection of the optimal drug or dose based on the patient’s specific ethnic background and other relevant demographic or health characteristics. In the current situation, with included ethnicities not being reported in the SmPC or SGPI, it is almost impossible for the prescriber to check if specific clinical data are available in these ethnic subpopulations. This situation is likely to contribute to worries on the safety of a drug product in different ethnic populations.
With the drive towards smart healthcare systems, statistical models of all trial data could be embedded in prescribing systems to recommend a drug regimen that would minimize risk and maximize benefit based on the individual’s characteristics, with ethnicity being among one of them. For such systems to function appropriately, it is crucial that all information, such as safety information in different ethnicities or races, are made available so this can be fed into such systems.
In the meantime, it would be advisable to routinely mention the ethnic background for major patients’ ethnic groups, as well as the population sizes that were included in the clinical development for a drug in the SmPC, SGPI and/or EPAR, to increase transparency around the totality of evidence available for the drug.
It is recognized that providing such information will increase the length of the SmPC, which in the end may act negatively on the willingness of prescribers to check the SmPC. To prevent this, the SmPC should only contain the relevant ethnic information that would facilitate clinical use, and the detailed ethnic information can be included in a specific section of the EPAR, which is intended to provide a more elaborate summary of the data supporting registration of a drug. Alternatively, more efficient ways of including information in the SmPC may be considered, such as the use of forest plots in order to provide an easily interpretable representation of, for example, ethnicity data, as was previously suggested by Menon-Anderson et al. [34]. Those interested in obtaining the more detailed data would then at least know that such data exist. Furthermore, as the EU moves towards electronic product information (ePI), there may be opportunities to include summary data on ethnic subpopulations without overshadowing other valuable information [35].
5 Conclusions
Despite the fact that ethnicity-specified safety data were only present in 12/25 (48%) EPARs, 8/25 (32%) SmPCs, and 9/25 (36%) SGPIs, detailed safety data in ethnic groups were present in almost all (96%) of the registration dossiers for a selection of 25 drugs that were registered in the EU in the time period 2007–2013.
Due to this situation, detailed safety information by ethnic group is often unknown to researchers, prescribers and patients due to information loss in translation towards EPARs and SmPCs or SGPIs. In order to increase awareness that such information exists, it is recommended to at least provide ethnic populations and group size investigated in clinical trials in these public regulatory documents. In this way, trust in the registered drugs in different ethnic populations may be increased, and more robust treatment decisions may be obtained in clinical practice. Regulatory agencies in other parts of the world that take reference from the EPARs and SmPCs would also be better informed of the size of the safety database in ethnic groups more closely related to the populations in their country.
References
Geiling EMK, Cannon PR. Pathologic effects of elixir of sulfanilamide (diethylene glycol) poisoning: a clinical and experimental correlation: final report. J Am Med Assoc. 1938;111(10):919–26.
Eriksson T, Björkman S, Höglund P. Clinical pharmacology of thalidomide. Eur J Clin Pharmacol. 2001;57(5):365–76.
Annas GJ, Elias S. Thalidomide and the titanic: reconstructing the technology tragedies of the twentieth century. Am J Public Health. 1999;89(1):98–101.
Jüni P, Nartey L, Reichenbach S, Sterchi R, Dieppe PA, Egger M. Risk of cardiovascular events and rofecoxib: cumulative meta-analysis. Lancet. 2004;364(9450):2021–9.
Downing NS, Aminawung JA, Shah ND, Braunstein JB, Krumholz HM, Ross JS. Regulatory review of novel therapeutics—comparison of three regulatory agencies. N Engl J Med. 2012;366(24):2284–93.
FitzGerald GA. Regulatory science: what it is and why we need it. Clin Pharmacol Ther. 2011;89(2):291–4.
Pezzola A, Sweet CM. Global pharmaceutical regulation: the challenge of integration for developing states. Glob Health. 2016;12(1):85.
Rägo L, Santoso B. Drug regulation: history, present and future. In: van Boxtel CJ, Santoso B, Edwards IR, editors. Drug benefits and risks: international textbook of clinical pharmacology, 2nd edition. IOS Press and Uppsala Monitoring Centre; 2008. pp.65–76.
Chong SSF, Lim JCW, Tominaga T. Developing key performance indicators to measure the progress of regional regulatory convergence and cooperation in Asia-Pacific Economic Cooperation (APEC). AAPS Open. 2018;4:4.
Chung W-H, Hung S-I, Hong H-S, Hsih M-S, Yang L-C, Ho H-C, et al. Medical genetics: a marker for Stevens-Johnson syndrome. Nature. 2004;428(6982):486.
Lonjou C, Thomas L, Borot N, Ledger N, de Toma C, LeLouet H, et al. A marker for Stevens-Johnson Syndrome: ethnicity Matters. Pharmacogenom J. 2006;6(4):265–8.
Nevitt SJ, Sudell M, Weston J, Tudur Smith C, Marson AG. Antiepileptic drug monotherapy for epilepsy: a network meta-analysis of individual participant data. Cochrane Database Syst Rev. 2017. https://doi.org/10.1002/14651858.CD011412.pub2.
Wang Q, Sun S, Xie M, Zhao K, Li X, Zhao Z. Association between the HLA-B alleles and carbamazepine-induced SJS/TEN: a meta-analysis. Epilepsy Res. 2017;135:19–28.
Manolio TA, Hutter CM, et al. Research directions in genetic predispositions to stevens-johnson syndrome/toxic epidermal necrolysis. Clin Pharmacol Ther. 2018;103(3):390–4.
Mehta TY, Prajapati LM, Mittal B, Joshi CG, Sheth JJ, Patel DB, et al. Association of HLA-B*1502 allele and carbamazepine-induced Stevens-Johnson syndrome among Indians. Indian J Dermatol Venereol Leprol. 2009;75(6):579.
Tassaneeyakul W, Jantararoungtong T, Chen P, Lin P-Y, Tiamkao S, Khunarkornsiri U, et al. Strong association between HLA-B*5801 and allopurinol-induced Stevens-Johnson syndrome and toxic epidermal necrolysis in a Thai population. Pharmacogenet Genomics. 2009;19(9):704–9.
Man CBL, Kwan P, Baum L, Yu E, Lau KM, Cheng ASH, et al. Association between HLA-B*1502 allele and antiepileptic drug-induced cutaneous reactions in Han Chinese. Epilepsia. 2007;48(5):1015–8.
Hung S-I, Chung W-H, Liou L-B, Chu C-C, Lin M, Huang H-P, et al. HLA-B*5801 allele as a genetic marker for severe cutaneous adverse reactions caused by allopurinol. Proc Natl Acad Sci U S A. 2005;102(11):4134–9.
Dean L. Allopurinol Therapy and HLA-B*58:01 Genotype. In: Pratt V, McLeod H, Rubinstein W, Dean L, Kattman B, Malheiro A (eds). Medical genetics summaries. Bethesda (MD): National Center for Biotechnology Information (US); 2012.
Lee S-C, Ng S-S, Oldenburg J, Chong P-Y, Rost S, Guo J-Y, et al. Interethnic variability of warfarin maintenance requirement is explained by VKORC1 genotype in an Asian population. Clin Pharmacol Ther. 2006;79(3):197–205.
ICH Guideline E5 R1. Ethnic Factors in the Acceptability of Foreign Clinical Data. 5 Feb 1998. Available at: https://www.ich.org/fileadmin/Public_Web_Site/ICH_Products/Guidelines/Efficacy/E5_R1/Step4/E5_R1__Guideline.pdf. Accessed 17 Aug 2018.
Vromans L, Doyle G, Petak-Opel S, Rödiger A, Röttgermann M, Schlüssel E, et al. Shaping medicinal product information: a before and after study exploring physicians’ perspectives on the summary of product characteristics. BMJ Open. 2013;3(8):1–9.
WHO Drug Information. Regulatory Collaboration. Vol 30, No. 4, 2016. Available at: https://www.who.int/medicines/publications/druginformation/WHO-DI_30-4_RegCollaboration.pdf. Accessed 17 Aug 2018.
Annex 1: Summary of Product Characteristics for Januvia 25 mg (sitagliptin), EMA. https://www.ema.europa.eu/en/documents/product-information/januvia-epar-product-information_en.pdf. Accessed 17 Aug 2018.
Package Insert for Januvia 25 mg (sitagliptin), Singapore, revised Aug 2017. https://eservice.hsa.gov.sg/prism/common/enquirepublic/SearchDRBProduct.do?action=load. Accessed 17 Aug 2018.
Annex 1: Summary of Product Characteristics for Trajenta 5 mg (linagliptin), EMA. https://www.ema.europa.eu/en/documents/product-information/trajenta-epar-product-information_en.pdf. Accessed 17 Aug 2018.
Package Insert for Forxiga 5 mg and 10 mg (dapagliflozin), Singapore, revised Oct 2018. https://eservice.hsa.gov.sg/prism/common/enquirepublic/SearchDRBProduct.do?action=load Accessed 17 Aug 2018.
Mallal S, Nolan D, Witt C, Masel G, Martin AM, Moore C, et al. Association between presence of HLA-B*5701, HLA-DR7, and HLA-DQ3 and hypersensitivity to HIV-1 reverse-transcriptase inhibitor abacavir. Lancet. 2002;359(9308):727–32.
Mallal S, Phillips E, Carosi G, Molina J-M, Workman C, Tomazic J, et al. HLA-B*5701 screening for hypersensitivity to abacavir. N Engl J Med. 2008;358(6):568–79.
Chen P, Lin J-J, Lu C-S, Ong C-T, Hsieh PF, Yang C-C, et al. Carbamazepine-induced toxic effects and HLA-B*1502 screening in Taiwan. N Engl J Med. 2011;364(12):1126–33.
Toh DSL, Tan LL, Aw DCW, Pang SM, Lim SH, Thirumoorthy T, et al. Building pharmacogenetics into a pharmacovigilance program in Singapore: using serious skin rash as a pilot study. Pharmacogenom J. 2014;14(4):316–21.
Teo Y-Y, Sim X, Ong RTH, Tan AKS, Chen J, Tantoso E, et al. Singapore genome variation project: a haplotype map of three southeast Asian populations. Genome Res. 2009;19(11):2154–62.
Ramamoorthy A, Pacanowski MA, Bull J, Zhang L. Racial/ethnic differences in drug disposition and response: review of recently approved drugs. Clin Pharmacol Ther. 2015;97(3):263–73.
Menon-Andersen D, Yu B, Madabushi R, Bhattaram V, Hao W, Uppoor RS, et al. Essential pharmacokinetic information for drug dosage decisions: a concise visual presentation in the drug label. Clin Pharmacol Ther. 2011;90(3):471–4.
European Medicines Association, Heads of Medicines Agencies, European Commission. Public consultation on key principles for the electronic product information of EU medicines. 31 Jan 2019. https://www.ema.europa.eu/en/documents/press-release/public-consultation-key-principles-electronic-product-information-eu-medicines_en.pdf. Accessed 17 Aug 2018.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
No external funding was received for this research. Open access was funded by Radboud University Medical Centre, Nijmegen, The Netherlands.
Conflicts of Interest
YY, ACT and MM are appointed by the Medicines Evaluation Board in The Netherlands. CS and JP are appointed by the Singapore Health Authority, the HSA. The authors have no further conflicts of interest.
Ethical Approval
This article does not contain any studies with human participants performed by any of the authors.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (http://creativecommons.org/licenses/by-nc/4.0/), which permits any noncommercial use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Maliepaard, M., Taams, A.C., Sung, C. et al. Ethnicity-Specific Drug Safety Data in European Medicines Agency Registration Dossiers, European Public Assessment Reports, and European and Singapore Drug Labels: Lost in Translation?. Pharm Med 33, 407–416 (2019). https://doi.org/10.1007/s40290-019-00302-2
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40290-019-00302-2