Abstract
Polycystic ovary syndrome (PCOS) is the most common endocrine disorder and cause of subfertility in women. The etiology of PCOS has not been fully elucidated; however, insulin resistance has been shown to exacerbate the disease process due to its effect on androgen synthesis. Progressive resistance training (PRT) is an anabolic exercise modality that can improve skeletal muscle size and quality (metabolic capacity), and studies have consistently shown that PRT can increase insulin sensitivity in type 2 diabetes and other cohorts. However, PRT is not currently recommended or routinely prescribed in PCOS. The objective of this article was to provide a rationale for the application of PRT in the management and treatment of PCOS. This will be accomplished by (1) overviewing the pathophysiology of PCOS with emphasis on the etiological role of insulin resistance; (2) summarizing the effectiveness of PRT in treating insulin resistance; (3) presenting evidence that PRT is feasible to prescribe in women with PCOS; and (4) providing general recommendations for PRT to complement existing guidelines for aerobic training in this cohort. We also provide recommendations for future research.
Similar content being viewed by others
Insulin resistance is a key etiological factor in polycystic ovary syndrome (PCOS). |
Progressive resistance training (PRT) can increase insulin sensitivity in patients with type 2 diabetes, but is not currently recommended or routinely prescribed in PCOS. |
1 Introduction
Polycystic ovary syndrome (PCOS) is the most common endocrine disorder in women, affecting 9–18 % of the female population during the reproductive years [1]. Many of these cases remain undiagnosed [1]. Hyperandrogenism, menstrual irregularity and polycystic ovaries define the condition [2], and common features include insulin resistance, hirsutism, acne, alopecia, overweight-obesity and other cardiometabolic risk factors (e.g. inflammation, dyslipidemia, etc.) [3, 4]. The prominent symptoms of PCOS include oligo/anovulation and oligo/amenorrhea contributing to infertility and increased risk of miscarriages [5, 6]. Depression [7], anxiety [8], body image difficulties [9] and low health-related quality of life [10] are commonly noted in this population. Women with PCOS also have a higher relative risk of type 2 diabetes mellitus (T2DM) [11–13], cardiovascular disease [12], and ovarian and endometrial cancers [14, 15] versus their healthy peers.
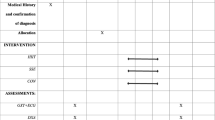
In 2011, the PCOS Australian Alliance published the first evidence-based guidelines for the assessment and management of PCOS [16]. The guidelines [16] acknowledge exercise as a first-line therapy and recommend a minimum of 150 min/week to improve clinical outcomes. Of this, 90 min/week should be spent engaged in aerobic activity at a moderate-to-high intensity (Table 1) [16]. Notably absent from the guidelines [16] is advocacy for progressive resistance training (PRT), an exercise modality that is recommended within exercise prescription position statements for healthy adults and those with major non-communicable diseases, including hypertension, heart disease, cancer, obesity, and T2DM [17–23].
Investigations have consistently shown that PRT can reverse or abate many of the physiological, functional and psychological impairments that accrue as a consequence of ageing and chronic disease [24]. PRT is well recognized as a potent exercise modality for increasing skeletal muscle size and quality (metabolic capacity) [24, 25] and, accordingly, many studies have shown that PRT can effectively treat metabolic diseases, including T2DM and obesity [25–28]. This is a key consideration for women with PCOS given that insulin resistance and obesity are highly prevalent and are known to exacerbate the disease process [29, 30]. PRT can potentially improve clinical outcomes while lowering the risk of cardiometabolic diseases and cancers in women with PCOS. However, to date, this exercise modality has been minimally investigated [31–35] and is not recommended or routinely prescribed in this population [16].
The objective of this article is to provide a rationale for the application of PRT in the management and treatment of PCOS. This will be accomplished by (1) overviewing the pathophysiology of PCOS with emphasis on the etiological role of insulin resistance; (2) summarizing the effectiveness of PRT in treating insulin resistance; (3) presenting evidence that PRT is feasible to prescribe in women with PCOS; and (4) providing general recommendations for PRT to complement existing guidelines for aerobic training in this cohort. We also provide recommendations for future research.
2 Pathophysiology of Polycystic Ovary Syndrome (PCOS)
In 2003, the European Society of Human Reproduction and Embryology and the American Society for Reproductive Medicine established a consensus definition of PCOS in Rotterdam, The Netherlands [2]. This definition, known as the Rotterdam criteria, specifies that two of the following three conditions must be present for a diagnosis of PCOS: (1) oligo- or anovulation; (2) elevated circulating androgen concentrations (hyperandrogenaemia; e.g. elevated testosterone, dehydroepiandrosterone) or clinical manifestations of androgen excess (hyperandrogenism, e.g. hirsutism, acne, alopecia); and (3) polycystic ovaries identified by ultrasound [2]. There are other consensus statements for PCOS diagnosis; however, the Rotterdam consensus [2] is the most widely accepted [36]. The National Institutes of Health also recommend that diagnosis include the PCOS phenotype (i.e. the conditions contributing to the diagnosis) [37].
The cause of PCOS is unknown [4] and therefore the etiology has not been comprehensively elucidated [38]. The prevailing view is that PCOS is a polygenic disorder resulting from the interaction of predisposing and protective genetic variants influenced by environmental factors (e.g. physical inactivity) [29]. Evidence for a genetic influence is based on the clustering of cases within families and suggests an autosomal dominant form of inheritance [39]. Many candidate genes have been investigated for a causal role in PCOS. However, these investigations remain contradictory and inconclusive [40]. No specific gene has been conclusively implicated in the causation of PCOS to date [39].
Lifestyle-related metabolic diseases, particularly overweight-obesity and insulin resistance, have been shown to exacerbate PCOS [29, 41]. For example, women with PCOS suffer a greater burden of overweight-obesity [42] and long-term weight gain [43] versus their unaffected peers. The prevalence of insulin resistance, glucose intolerance and T2DM is also much higher in PCOS than in healthy controls [13, 30]. Notably, insulin resistance can affect both normal weight and overweight women with PCOS [30, 44]. For example, a study employing the hyperinsulinemic-euglycemic clamp confirmed insulin resistance in 75 % of normal weight (body mass index [BMI] <27 kg/m2) and 95 % of overweight-obese (BMI >27 kg/m2) PCOS cases [30]. Insulin resistance in normal weight PCOS may be caused by excess abdominal fat (i.e. android obesity) [45], although these data are not conclusive [46]. Android obesity is common in PCOS [46–49] and is known to increase the risk of insulin resistance [50]. The presence of obesity and insulin resistance in PCOS may be influenced by sedentary behaviour and excess caloric intake [51]; however, the relative contribution of these factors to the etiology of PCOS is unknown.
2.1 Insulin Resistance and Androgen Excess
PCOS is a condition that deviates from the normal occurrence of ovarian follicle growth and atresia. It is characterized by accelerated growth and premature growth arrest of follicles, without atresia [52, 53]. These small arrested follicles are the cysts that characterize the disease [2]. The theca and granulosa cells within the ovary are responsible for steroidogenesis, including the production of androstenedione, testosterone, progesterone and estradiol. Insulin resistance induces hyperinsulinemia, which causes the theca cells to produce more androgens [29]. Increased androgen synthesis by the theca cells is believed to disrupt the normal process of follicular maturation and atresia leading to premature arrest [54]. Hence, insulin resistance exacerbates the PCOS disease process through its effect on androgen production. Hyperandrogenemia, in turn, may also exacerbate insulin resistance and fat accumulation in the peripheral tissues (muscle and fat cells) [52, 55, 56], creating a self-perpetuating cycle of fat accumulation, insulin resistance and androgen excess. The pathways by which these metabolic aberrations occur in PCOS are complex and require further investigation [29, 38, 52, 56].
2.2 Similarities to Type 2 Diabetes
The etiology of insulin resistance in PCOS is not well understood. However, there is evidence of similarities to the insulin resistance characterizing T2DM [57]. In both conditions, insulin resistance arises due to post-binding defects in insulin signal transduction that impair insulin-mediated glucose transporter type 4 (GLUT4) translocation and glucose uptake [52, 57–59]. Post-binding insulin signal transduction defects that are common to both PCOS and T2DM include reduced phosphorylation of insulin receptor substrate 1 (IRS-1) and associated phosphoinositide 3-kinase [60], reduced signalling via AS160, defects in protein kinase C ζ/λ activation, upregulation of extracellular signal-regulated kinase 1/2 (ERK1/ERK2) signalling, and possible impaired signalling of protein kinase B (Akt 1) [57]. Related impairments of oxidative metabolism have also been noted in both PCOS and T2DM [61–63]. Insulin signalling defects in these diseases are exacerbated by environmental factors (e.g. low physical activity) and overweight-obesity [59, 64, 65].
Intrinsic factors may also contribute to insulin resistance in PCOS; however, these factors are not well understood [65]. It has been suggested that women with PCOS might suffer from a ‘thrifty’ genotype [66] similar to indigenous populations that are predisposed to T2DM [67, 68]. Hence, women with PCOS may be more prone to storing fat as a fuel source (triglyceride) and require greater dosages of physical activity than healthy peers to maintain optimal body adiposity [69]. This notion remains controversial in light of recent data [70]. Excess intramyocellular triglyceride (or intramuscular lipid) resulting in elevations of metabolic byproducts such as long-chain acyl-CoA esters, ceramide and diacylglycerol has been implicated in post-binding insulin signalling defects [71, 72]. However, paradoxically, a recent study noted a trend toward lower muscle lipid content (p = 0.08), despite greater insulin resistance (p = 0.01), in 16 women with PCOS versus 13 healthy controls [70]. The women with PCOS also showed a trend toward increased muscle lipid content (p = 0.19), accompanied by increased insulin sensitivity (p = 0.01) and decreased visceral fat (p = 0.03), after 12 weeks of interval training [49, 70]. This effect of training on intramuscular lipid suggests improved fatty acid metabolism, similar to the effects noted in endurance-trained athletes [73]. Nevertheless, the effect of visceral fat, intramuscular lipid and related fatty acid moieties on the etiology of insulin resistance in women with PCOS is not well understood, indicating a need for further research.
3 A Rationale for Progressive Resistance Training (PRT) in PCOS
PRT is an anabolic form of exercise that involves challenging the skeletal muscles with unaccustomed loads, usually in the form of free- or machine weights. Several resistance exercises are typically incorporated into a training session such that multiple muscle groups are targeted [23]. Providing the trained muscles with 48–72 h of recovery prior to the next training stimulus optimizes adaptation, and two to three full body training sessions per week on non-consecutive days are recommended for untrained or novice lifters [23]. The most favourable adaptations of skeletal muscle in inexperienced lifters appear to be elicited by sets of 8–12 repetitions performed to the onset of neuromuscular fatigue [i.e. 8–12 repetitions maximum (RM)], the point at which proper technique can no longer be maintained [23]. To facilitate continued adaptation over the long-term, i.e. attenuate the onset of a health- or performance-related plateau, the training intensity (load) and/or training volume (number of sets and exercises) must be progressively increased and/or the exercises must be made more complex [23]. Once the desired plateau has been attained, health and performance are maintained with maintenance training, which may involve the periodic manipulation of training variables, including training frequency, intensity and repetition range, types of exercises, time under tension, etc. [23].
3.1 PRT Improves Insulin Sensitivity
Insulin resistance contributes to androgen excess and the etiology of PCOS, therefore interventions to remedy PCOS should be effective in targeting this pathology. Skeletal muscle is the largest reservoir for insulin-stimulated glucose disposal [74]. PRT can elicit improvements in skeletal muscle size and quality (metabolic capacity) contributing to improvements in insulin sensitivity and related markers of glucoregulation in patients with T2DM [25, 27, 75]. These data have been comprehensively presented in a recent systematic review of 13 randomized controlled trials (RCTs) [76]. Several studies have shown that 16 weeks of PRT can increase insulin sensitivity by more than 45 % in patients with obesity and T2DM [77, 78]. The insulin-sensitizing effects of PRT are not limited to obese patients. Non-obese patients with T2DM [79], and even lean, non-diabetic populations [80], have also been shown to benefit. The PRT-induced improvement of insulin sensitivity in T2DM is often accompanied by favourable shifts in body composition (i.e. reduced fat mass and increased fat-free mass) [76]. The loss of fat mass is likely mediated by a rise in the basal metabolic rate which occurs as a consequence of improved muscle mass and metabolism [25]. Notably, these beneficial metabolic effects of PRT can occur without changes in body weight per se [76].
Exercise-related improvements in insulin sensitivity in T2DM have been attributed to increased expression and activity of key proteins involved in the regulation of glucose uptake, metabolism and insulin signalling [81]. Such adaptation would be beneficial in PCOS. One study prescribing 6 weeks of isolated PRT in patients with T2DM noted significant improvements in the protein content of GLUT4, insulin receptors, Akt 1, Akt 2 and glycogen synthase in skeletal muscle [82]. The improvement of insulin sensitivity was also accompanied by type II muscle fibre hypertrophy [82]. Another study showed a significant increase in IRS-1 expression (65 %) in skeletal muscle secondary to 12 weeks of PRT, and this change was concomitant with several favourable metabolic adaptations [83]. PRT has also been shown to induce significant increases in mitochondrial density (+10 %) and oxidative capacity (+57 %) [84] contributing to greater turnover of glucose/glycogen and triglyceride within the myocyte.
The evidence base for PRT in the treatment of insulin resistance has informed exercise prescription guidelines for patients with T2DM. The American College of Sports Medicine and the American Diabetes Association recommend that patients with T2DM engage in two to three PRT sessions per week on non-consecutive days [22]. Training intensities should commence at 10–15 RM and progress to 8–10 RM. Higher intensities are recommended as preferable for the improvement of insulin sensitivity [22]. Moreover, it is advised that PRT be prescribed in combination with aerobic training [22]. While there is evidence that either modality is effective in isolation, the greatest metabolic improvements occur when aerobic and PRT are combined [28].
3.2 PRT in PCOS
The adaptations that underlie, or are associated with, improved insulin sensitivity in T2DM would be favourable for women with PCOS. These adaptations could potentially contribute to ameliorating the disease process and related symptoms. To our knowledge, only four studies have incorporated PRT within a comprehensive lifestyle-based intervention for women with PCOS [31–35]. These studies are summarized in Table 2. Given the multimodal nature of the interventions applied in these studies, it is not possible to draw conclusions regarding the isolated effect of PRT on specific clinical outcomes in PCOS. However, it is important to elucidate the strengths and weaknesses of the PRT regimens prescribed in these studies, and determine the feasibility and safety of these prescriptions by evaluating adherence and adverse events attributed to PRT, if any.
Bruner et al. [32] conducted a 12-week pilot RCT in 12 young women with PCOS, elevated BMI (36.6 kg/m2) and abdominal obesity (mean waist circumference = 98.9 cm). The women were randomized into an experimental group (n = 7) that received aerobic plus PRT plus nutritional counseling, and a control group (n = 5) that received nutritional counseling only. The exercise programme was performed three times per week and the PRT component involved 12 standard exercises that were performed for two sets of 10 repetitions each session. The training volume was progressed to three sets of 15 repetitions, and once 15 repetitions could be ‘completed comfortably,’ the load was progressed by 2.2 kg or 5 %. It was not clear if each set was performed to neuromuscular fatigue as the training intensity was not defined according to RM. Several clinically important outcome measures were collected pre- and post-intervention. The experimental group significantly increased cardiorespiratory fitness, and significantly reduced subcutaneous adiposity (sum of two skinfolds) versus the control group. No additional group × time interactions effects were noted. The authors did not provide information about compliance, supervision or adverse events.
Thomson et al. [33, 34] conducted a 20-week RCT enrolling 104 women with PCOS and elevated BMI (>25 kg/m2). Participants were randomized into three groups: (1) diet only (DO); (2) diet plus aerobic training (DA); and (3) diet plus combined aerobic and resistance training (DC). The frequency of aerobic training was not equated between DA (five sessions per week) and DC (three sessions per week); hence, the study did not specifically investigate the additive (isolated) effect of PRT. The PRT component undertaken by DC consisted of training twice per week on non-consecutive days. Each training session involved five standard exercises that were initiated at 50–60 % of 1RM for the first 2 weeks and then loads were increased to 65–75 % of 1RM. Subsequently, the loads were increased once participants could perform three sets of 12 repetitions. It is not clear if participants trained to neuromuscular fatigue. The rate of volume (number of sets and repetitions) progression was also not detailed. Outcomes were collected pre- and post-intervention and included measures of body composition, cardiometabolic risk, endocrine system status, reproductive function, depression and PCOS-specific quality of life. The DC group significantly improved body fat percentage, fat mass and fat-free mass versus the DO group. No group × time interaction effects were reported for DC versus DA. Notably, the study had a large attrition rate (50 %), with only 52 women completing the intervention and testing sessions. In those who completed the intervention, the average compliance to exercise training (in DA and DC) was 79 % [33]. Eight participants withdrew from the study due to injury or illness; however, the authors did not mention the cause of these adverse events. No information was provided about the supervision of training sessions.
Two additional studies [31, 35] utilized uncontrolled designs and prescribed PRT with aerobic training and nutrition classes or nutrition advice. No specific details were provided about the PRT component of the intervention in either of these studies. Significant improvements were noted in anthropometric measures, dietary intake and physical activity participation. The authors did not provide information about compliance, supervision or adverse events.
Of the four studies that have investigated the effect of lifestyle-based interventions incorporating PRT [31–35], only one has reported on participant compliance [33] and none have reported on adverse events due to exercise training. Two studies detailed standard PRT regimens [32–34]; however, training intensity and progression were not well reported. Two studies [31, 35] provided no information about the PRT aspect of their intervention.
4 Future Research Directions
The exercise guidelines provided by the PCOS Australian Alliance (Table 1) are based on six to eight studies that have primarily investigated the effectiveness of walking or cycling prescribed three to five sessions per week for 12–24 weeks [85–87]. These interventions have been shown to elicit a number of clinically relevant adaptations, including increased aerobic fitness, ovulation and menstrual cyclicity, and reduced body weight, waist circumference, waist-to-hip ratio, hirsutism, total testosterone, and insulin resistance [85–87]. However, the PCOS Australian Alliance [16] have acknowledged that this evidence base is largely preliminary and that more high-quality research is needed. Most of the trials have utilized non-randomized or uncontrolled study designs [49, 70, 85, 88–91], and of the few RCTs [92–94], none have adhered to current standards of reporting [95]. With the exception of two studies [88, 94], sample sizes have been small (n = 20 to n = 40), thus limiting the generalizability of the findings to the broader PCOS population. Furthermore, few studies have prescribed PRT [31, 32, 34] and no study has investigated the isolated effect of PRT.
Robust RCTs are required to determine if specific dosages of PRT can effectively treat a range of pertinent outcomes in PCOS, including insulin sensitivity, endocrine status (e.g. androgens), polycystic ovary morphology, body composition (i.e. fat mass, fat-free mass and visceral adiposity), hirsutism, cardiometabolic risk factors, psychological health status, ovulatory and menstrual cyclicity, and fertility (conception). PRT could be hypothesized to improve all of these outcomes given its effectiveness in treating insulin resistance and related outcomes in T2DM.
Thorough and standardized reporting [95] is required of future clinical trials. Patient characteristics should be clearly described, including PCOS phenotypes and comorbidities. Interventions should be thoroughly defined with respect to frequency, intensity, modality, session duration, delivery, and supervision. This is essential for determining the PRT prescription required to positively affect specific outcomes and determine dose-response relationships, as well as potential facilitators of adherence (e.g. high versus low intensity, supervised versus unsupervised training, etc.). Compliance to training should be defined a priori and appropriately reported to determine the feasibility and generalizability of prescribing PRT in this patient population. Thorough reporting of adverse events, including a priori definitions, is necessary to determine the risk-to-benefit ratio of PRT in this cohort, which is suggested to be favourable based on data from other chronically diseased populations [24]. Future investigations should also be conducted explicitly with targeted subpopulations within this cohort (e.g. women attempting to conceive, women suffering from clinical depression, etc.).
Long-term behavioural change is the challenge to exercise prescription in most clinical cohorts, and women with PCOS are no exception. Future studies can contribute to the successful dissemination of their research findings if barriers and motivators to the exercise programme are investigated and reported.
5 Conclusions
There is a physiological rationale for prescribing PRT in women with PCOS. Insulin resistance and androgen excess are interrelated features of the disease that contribute to its exacerbation. PRT has consistently been shown to increase insulin sensitivity in patients with T2DM, and given that the underlying features of insulin resistance are similar between these conditions, it can be hypothesized that PRT can improve clinical outcomes in PCOS as well. Four studies incorporating PRT within a lifestyle-based intervention suggest that this modality of training is feasible to prescribe [31–35]. Although gaps in the knowledge are clearly evident, there is sufficient empirical evidence to support the addition of PRT to exercise prescription guidelines in PCOS.
5.1 Recommendations for PRT in PCOS
In Table 3, we present general recommendations for PRT that align with numerous position statements published by the American College of Sports Medicine and Exercise and Sport Science Australia [17–23]. Our recommendations are designed to elicit improvements in skeletal muscle size and quality (metabolic capacity) to potentially improve a number of clinically relevant outcomes in PCOS. These recommendations for PRT should be considered by healthcare professionals, including exercise physiologists [96], who provide quality care to women with PCOS, and should be used in conjunction with existing guidelines for aerobic training provided by the PCOS Australian Alliance [16].
References
March WA, Moore VM, Willson KJ, et al. The prevalence of polycystic ovary syndrome in a community sample assessed under contrasting diagnostic criteria. Human Reprod. 2010;25(2):544–51.
Rotterdam ESHRE/ASRM-sponsored PCOS Consensus Workshop Group. Revised 2003 consensus on diagnostic criteria and long-term health risks related to polycystic ovary syndrome. Fertil Steril. 2004;81(1):19–25.
Ehrmann DA. Polycystic ovary syndrome. N Engl J Med. 2005;352(12):1223–36.
Norman RJ, Dewailly D, Legro RS, et al. Polycystic ovary syndrome. Lancet. 2007;370(9588):685–97.
Giudice LC. Endometrium in PCOS: implantation and predisposition to endocrine CA. Best Pract Res Clin Endocrinol Metab. 2006;20(2):235–44.
Gorry A, White DM, Franks S. Infertility in polycystic ovary syndrome. Endocrine. 2006;30(1):27–33.
Bhattacharya SM, Jha A. Prevalence and risk of depressive disorders in women with polycystic ovary syndrome (PCOS). Fertil Steril. 2010;94(1):357–9.
Deeks AA, Gibson-Helm ME, Teede HJ. Anxiety and depression in polycystic ovary syndrome: a comprehensive investigation. Fertil Steril. 2010;93(7):2421–3.
Himelein MJ, Thatcher SS. Depression and body image among women with polycystic ovary syndrome. J Health Psychol. 2006;11(4):613–25.
Barnard L, Ferriday D, Guenther N, et al. Quality of life and psychological well being in polycystic ovary syndrome. Hum Reprod. 2007;22(8):2279–86.
Schmidt J, Landin-Wilhelmsen K, Brännström M, et al. Cardiovascular disease and risk factors in PCOS women of postmenopausal age: a 21-year controlled follow-up study. J Clin Endocrinol Metab. 2011;96(12):3794–803.
de Groot PC, Dekkers OM, Romijn JA, et al. PCOS, coronary heart disease, stroke and the influence of obesity: a systematic review and meta-analysis. Hum Reprod Update. 2011;17(4):495–500.
Moran LJ, Misso ML, Wild RA, et al. Impaired glucose tolerance, type 2 diabetes and metabolic syndrome in polycystic ovary syndrome: a systematic review and meta-analysis. Hum Reprod Update. 2010;16(4):347–63.
Chittenden BG, Fullerton G, Maheshwari A, et al. Polycystic ovary syndrome and the risk of gynaecological cancer: a systematic review. Reprod Biomed Online. 2009;19(3):398–405.
Dumesic DA, Lobo RA. Cancer risk and PCOS. Steroids. 2013;78(8):782–5.
Teede HJ, Misso ML, Deeks AA, et al. Assessment and management of polycystic ovary syndrome: summary of an evidence-based guideline. Med J Aust. 2011;195(6):S65–112.
Hordern MD, Dunstan DW, Prins JB, et al. Exercise prescription for patients with type 2 diabetes and pre-diabetes: a position statement from Exercise and Sport Science Australia. J Sci Med Sport. 2012;15(1):25–31.
Sharman JE, Stowasser M. Australian Association for Exercise and Sports Science position statement on exercise and hypertension. J Sci Med Sport. 2009;12(2):252–7.
Hayes S, Spence R, Galvao D, et al. Australian Association of Exercise and Sport Science position stand: optimising cancer outcomes through exercise. J Sci Med Sport. 2009;12:428–34.
Donnelly J, Blair S, Jakicic J, American College of Sports Medicine Position Stand, et al. Appropriate physical activity intervention strategies for weight loss and prevention of weight regain for adults. Med Sci Sports Exerc. 2009;41(2):459–71.
Selig SE, Levinger I, Williams AD, et al. Exercise & Sports Science Australia Position Statement on exercise training and chronic heart failure. J Sci Med Sport. 2010;13(3):288–94.
Colberg SR, Sigal RJ, Fernhall B, et al. Exercise and type 2 diabetes: the American College of Sports Medicine and the American Diabetes Association: joint position statement. Diabetes Care. 2010;33(12):e147–67.
Kraemer W, Adams K, Cafarelli E, et al. Progression models in resistance training for healthy adults. Med Sci Sports Exerc. 2002;34(2):364–80.
Ciccolo J, Kraemer WJ. Resistance training for the prevention and treatment of chronic disease. Boca Raton: CRC Press; 2013.
Tresierras M, Balady G. Resistance training in the treatment of diabetes and obesity: mechanisms and outcomes. J Cardiopulm Rehabil Prev. 2009;29(2):67–75.
Strasser B, Schobersberger W. Evidence for resistance training as a treatment therapy in obesity. J Obes 2011. doi:10.1155/2011/482564.
Strasser B, Siebert U, Schobersberger W. Resistance training in the treatment of the metabolic syndrome. Sports Med. 2010;40(5):397–415.
Sigal R, Kenny G, Boulé N, et al. Effects of aerobic training, resistance training, or both on glycemic control in type 2 diabetes. Ann Intern Med. 2007;147:357–69.
Diamanti-Kandarakis E, Christakou C. Insulin resistance in PCOS. In: Farid N, Diamanti-Kandarakis E, editors. Diagnosis and management of polycystic ovary syndrome. New York: Springer; 2009. p. 35–61.
Stepto NK, Cassar S, Joham AE, et al. Women with polycystic ovary syndrome have intrinsic insulin resistance on euglycaemic-hyperinsulaemic clamp. Hum Reprod. 2013;28(3):777–84.
Aubuchon M, Laughbaum N, Poetker A, et al. Supervised short-term nutrition and exercise promotes weight loss in overweight and obese patients with polycystic ovary syndrome. Fertil Steril. 2009;91(4):1336–8.
Bruner B, Chad K, Chizen D. Effects of exercise and nutritional counseling in women with polycystic ovary syndrome. Appl Physiol Nutr Metab. 2006;31(4):384–91.
Thomson RL, Buckley JD, Lim SS, et al. Lifestyle management improves quality of life and depression in overweight and obese women with polycystic ovary syndrome. Fertil Steril. 2010;94(5):1812–6.
Thomson RL, Buckley JD, Noakes M, et al. The effect of a hypocaloric diet with and without exercise training on body composition, cardiometabolic risk profile, and reproductive function in overweight and obese women with polycystic ovary syndrome. J Clin Endocrinol Metab. 2008;93(9):3373–80.
Mahoney D. Lifestyle modification intervention among infertile overweight and obese women with polycystic ovary syndrome. J Am Assoc Nurse Pract 2013. doi:10.1002/2327-6924.12073.
Boyle J, Teede HJ. Polycystic ovary syndrome: an update. Aust Fam Physician. 2012;41(10):752–6.
National Institutes of Health. Evidence-based methodology workshop on polycystic ovary syndrome, 3–5 December 2012. Executive summary. Final report. National Institutes of Health; 2012. Available from: https://prevention.nih.gov/docs/programs/pcos/FinalReport.pdf.
Tsilchorozidou T, Overton C, Conway GS. The pathophysiology of polycystic ovary syndrome. Clin Endocrinol. 2003;60(1):1–17.
Amato P, Simpson JL. The genetics of polycystic ovary syndrome. Best Pract Res Clin Obstet Gynaecol. 2004;18(5):707–18.
Urbanek M. The genetics of the polycystic ovary syndrome. Nat Clin Pract Endocrinol Metab. 2007;3(2):103–11.
Pasquali R, Gambineri A, Pagotto U. The impact of obesity on reproduction in women with polycystic ovary syndrome. BJOG. 2006;113(10):1148–59.
Lim SS, Davies MJ, Norman RJ, et al. Overweight, obesity and central obesity in women with polycystic ovary syndrome: a systematic review and meta-analysis. Hum Reprod Update. 2012;18(6):618–37.
Teede HJ, Joham AE, Paul E, et al. Longitudinal weight gain in women identified with polycystic ovary syndrome: results of an observational study in young women. Obesity. 2013;21(8):1526–32.
Toprak S, Yonem A, Cakir B, et al. Insulin resistance in nonobese patients with polycystic ovary syndrome. Horm Res. 2001;55(2):65–70.
Cascella T, Palomba S, De Sio I, et al. Visceral fat is associated with cardiovascular risk in women with polycystic ovary syndrome. Hum Reprod. 2008;23(1):153–9.
Carmina E, Bucchieri S, Esposito A, et al. Abdominal fat quantity and distribution in women with polycystic ovary syndrome and extent of its relation to insulin resistance. J Clin Endocrinol Metab. 2007;92(7):2500–5.
Kirchengast S, Huber J. Body composition characteristics and body fat distribution in lean women with polycystic ovary syndrome. Hum Reprod. 2001;16(6):1255–60.
Yildirim B, Sabir N, Kaleli B. Relation of intra-abdominal fat distribution to metabolic disorders in nonobese patients with polycystic ovary syndrome. Fertil Steril. 2003;79(6):1358–64.
Hutchison SK, Stepto NK, Harrison CL, et al. Effects of exercise on insulin resistance and body composition in overweight and obese women with and without polycystic ovary syndrome. J Clin Endocrinol Metab. 2011;96(1):E48–56.
Amati F, Pennant M, Azuma K, et al. Lower thigh subcutaneous and higher visceral abdominal adipose tissue content both contribute to insulin resistance. Obesity. 2012;20(5):1115–7.
Moran LJ, Ranasinha S, Zoungas S, et al. The contribution of diet, physical activity and sedentary behaviour to body mass index in women with and without polycystic ovary syndrome. Hum Reprod. 2013;28(8):2276–83.
Diamanti-Kandarakis E, Dunaif A. Insulin resistance and the polycystic ovary syndrome revisited: an update on mechanisms and implications. Endocr Rev. 2012;33(6):981–1030.
Welt CK, Taylor AE, Fox J, et al. Follicular arrest in polycystic ovary syndrome is associated with deficient inhibin A and B biosynthesis. J Clin Endocrinol Metab. 2005;90(10):5582–7.
Jonard S, Dewailly D. The follicular excess in polycystic ovaries, due to intra-ovarian hyperandrogenism, may be the main culprit for the follicular arrest. Hum Reprod Update. 2004;10(2):107–17.
Lovejoy J, Bray G, Bourgeois M, et al. Exogenous androgens influence body composition and regional body fat distribution in obese postmenopausal women: a clinical research center study. Clin Endocrinol Metab. 1996;81(6):2198–203.
Livingstone C, Collison M. Sex steroids and insulin resistance. Clin Sci. 2002;102(2):151–66.
Corbould A. Insulin resistance in skeletal muscle and adipose tissue in polycystic ovary syndrome: are the molecular mechanisms distinct from type 2 diabetes? Panminerva Med. 2008;50(4):279–94.
Dantas WS, Gualano B, Rocha MP, et al. Metabolic disturbance in PCOS: clinical and molecular effects on skeletal muscle tissue. Scientific World J 2013. doi:10.1155/2013/178364.
Kahn SE, Hull RL, Utzschneider KM. Mechanisms linking obesity to insulin resistance and type 2 diabetes. Nature. 2006;444(7121):840–6.
Dunaif A, Wu X, Lee A, et al. Defects in insulin receptor signaling in vivo in the polycystic ovary syndrome (PCOS). Am J Physiol Endocrinol Metab. 2001;281(2):E392–9.
Skov V, Glintborg D, Knudsen S, et al. Reduced expression of nuclear-encoded genes involved in mitochondrial oxidative metabolism in skeletal muscle of insulin-resistant women with polycystic ovary syndrome. Diabetes. 2007;56(9):2349–55.
Patti ME, Butte AJ, Crunkhorn S, et al. Coordinated reduction of genes of oxidative metabolism in humans with insulin resistance and diabetes: potential role of PGC1 and NRF1. Proc Natl Acad Sci U S A. 2003;100(14):8466–71.
Mootha VK, Lindgren CM, Eriksson K-F, et al. PGC-1α-responsive genes involved in oxidative phosphorylation are coordinately downregulated in human diabetes. Nat Genet. 2003;34(3):267–73.
Puder JJ, Varga S, Kraenzlin M, et al. Central fat excess in polycystic ovary syndrome: relation to low-grade inflammation and insulin resistance. J Clin Endocrinol Metab. 2005;90(11):6014–21.
Corbould A, Kim YB, Youngren JF, et al. Insulin resistance in the skeletal muscle of women with PCOS involves intrinsic and acquired defects in insulin signaling. Am J Physiol Endocrinol Metab. 2005;288(5):E1047–54.
Holte J. Polycystic ovary syndrome and insulin resistance: thrifty genes struggling with over-feeding and sedentary life style? J Endocrinol Invest. 1998;21(9):589–601.
Busfield F, Duffy DL, Kesting JB, et al. A genomewide search for type 2 diabetes: susceptibility genes in indigenous Australians. Am J Hum Genet. 2002;70(2):349–57.
Sukala W, Page R, Cheema B. Targeting the type 2 diabetes epidemic in Polynesia: historical perspective and rationale for exercise intervention trials. Ethn Dis. 2012;22(2):123–8.
Chakravarthy MV, Booth FW. Eating, exercise, and “thrifty” genotypes: connecting the dots toward an evolutionary understanding of modern chronic diseases. J Appl Physiol. 2004;96(1):3–10.
Hutchison S, Teede H, Rachoń D, et al. Effect of exercise training on insulin sensitivity, mitochondria and computed tomography muscle attenuation in overweight women with and without polycystic ovary syndrome. Diabetologia. 2012;55(5):1424–34.
Stannard S, Johnson N. Insulin resistance and elevated triglyceride in muscle: more important for survival than ‘thrifty’ genes? J Physiol. 2003;554(3):595–607.
Cooney GJ, Thompson AL, Furler SM, et al. Muscle long-chain Acyl CoA Esters and insulin resistance. Ann N Y Acad Sci. 2002;967(1):196–207.
Amati F, Dube JJ, Alvarez-Carnero E, et al. Skeletal muscle triglycerides, diacylglycerols, and ceramides in insulin resistance: another paradox in endurance-trained athletes? Diabetes. 2011;60(10):2588–97.
Zierath JR, Krook A, Wallberg-Henriksson H. Insulin action and insulin resistance in human skeletal muscle. Diabetologia. 2000;43(7):821–35.
Peppa M, Koliaki C, Nikolopoulos P, et al. Skeletal muscle insulin resistance in endocrine disease. J Biomed Biotechnol 2010. doi:10.1155/2010/527850.
Gordon B, Benson A, Bird S, et al. Resistance training improves metabolic health in type 2 diabetes: a systematic review. Diabetes Res Clin Pract. 2009;83:157–75.
Ibanez J, Izquierdo M, Arguelles I, et al. Twice-weekly progressive resistance training decreases abdominal fat and improves insulin sensitivity in older men with type 2 diabetes. Diabetes Care. 2005;28:662–7.
Shaibi G, Cruz M, Ball G, et al. Effects of resistance training on insulin sensitivity in overweight latino adolescent males. Med Sci Sports Exerc. 2006;38(7):1208–15.
Ishii T, Yamakita T, Sato T, et al. Resistance training improves insulin sensitivity in NIDDM subjects without altering maximal oxygen uptake. Diabetes Care. 1998;21(8):1353–5.
Poehlman E, Dvorak R, DeNino W, et al. Effects of resistance training and endurance training on insulin sensitivity in nonobese, young women: a controlled randomized trial. J Clin Endocrinol Metab. 2000;85:2463–8.
Hawley J, Lessard S. Exercise training-induced improvements in insulin action. Acta Physiol. 2008;192:127–35.
Holten M, Zacho M, Gaster M, et al. Strength training increases insulin-mediated glucose uptake, GLUT4 content, and insulin signaling in skeletal muscles in patients with type 2 diabetes. Diabetes. 2004;53:294–305.
Jorge MLMP, de Oliveira VN, Resende NM, et al. The effects of aerobic, resistance, and combined exercise on metabolic control, inflammatory markers, adipocytokines, and muscle insulin signaling in patients with type 2 diabetes mellitus. Metabolism. 2011;60(9):1244–52.
Jubrias SA, Esselman PC, Price LB, et al. Large energetic adaptations of elderly muscle to resistance and endurance training. J Appl Physiol. 2001;90(5):1663–70.
Moran LJ, Hutchison SK, Norman RJ, et al. Lifestyle changes in women with polycystic ovary syndrome. Cochrane Database Syst Rev 2011;(2):CD007506.
Harrison CL, Lombard CB, Moran LJ, et al. Exercise therapy in polycystic ovary syndrome: a systematic review. Hum Reprod Update. 2011;17(2):171–83.
Thomson RL, Buckley JD, Brinkworth GD. Exercise for the treatment and management of overweight women with polycystic ovary syndrome: a review of the literature. Obes Rev. 2011;12(5):e202–10.
Giallauria F, Palomba S, Maresca L, et al. Exercise training improves autonomic function and inflammatory pattern in women with polycystic ovary syndrome (PCOS). Clin Endocrinol. 2008;69(5):792–8.
Harrison CL, Stepto NK, Hutchison SK, et al. The impact of intensified exercise training on insulin resistance and fitness in overweight and obese women with and without polycystic ovary syndrome. Clin Endocrinol. 2012;76(3):351–7.
Palomba S, Giallauria F, Falbo A, et al. Structured exercise training programme versus hypocaloric hyperproteic diet in obese polycystic ovary syndrome patients with anovulatory infertility: a 24-week pilot study. Hum Reprod. 2008;23(3):642–50.
Randeva HS, Lewandowski KC, Drzewoski J, et al. Exercise decreases plasma total homocysteine in overweight young women with polycystic ovary syndrome. J Clin Endocrinol Metab. 2002;87(10):4496–501.
Brown AJ, Setji TL, Sanders LL, et al. Effects of exercise on lipoprotein particles in women with polycystic ovary syndrome. Med Sci Sports Exerc. 2009;41(3):497–504.
Stener-Victorin E, Jedel E, Janson PO, et al. Low-frequency electroacupuncture and physical exercise decrease high muscle sympathetic nerve activity in polycystic ovary syndrome. Am J Physiol Regul Integr Comp Physiol. 2009;297(2):R387–95.
Vigorito C, Giallauria F, Palomba S, et al. Beneficial effects of a three-month structured exercise training program on cardiopulmonary functional capacity in young women with polycystic ovary syndrome. J Clin Endocrinol Metab. 2007;92(4):1379–84.
Schulz KF, Altman DG, Moher D. CONSORT 2010 statement: updated guidelines for reporting parallel group randomised trials. Trials. 2010;11:32. doi:10.1186/1745-6215-11-32.
Cheema B, Robergs R, Askew C. Exercise physiologists emerge as allied healthcare professionals in the era of non-communicable disease pandemics: a report from Australia, 2006–2012. Sports Med. Epub 25 Mar 2014. http://www.ncbi.nlm.nih.gov/pubmed/24664532.
Acknowledgments
Birinder S. Cheema is guarantor of the paper, taking responsibility for the integrity of the work as a whole, from inception to published article. All authors have contributed to the preparation of the manuscript and have approved and read the final article. This research received no specific grant from any funding agency in the public, commercial or not-for-profit sectors. All authors declare they have no competing interests.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Cheema, B.S., Vizza, L. & Swaraj, S. Progressive Resistance Training in Polycystic Ovary Syndrome: Can Pumping Iron Improve Clinical Outcomes?. Sports Med 44, 1197–1207 (2014). https://doi.org/10.1007/s40279-014-0206-6
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40279-014-0206-6