Abstract
Background
Opioid analgesics are commonly used to manage pain; however, it is unclear how they affect patient function. This study examines the association between opioid analgesics and incident limitations in activities of daily living (ADL), instrumental activities of daily living (IADL), and cognitive functioning among community-dwelling older adults.
Methods
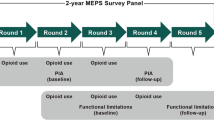
Data included 10,003 participants of the 2016 and 2018 waves of the Health and Retirement Study, which sampled US adults aged 51–98 years. The primary exposure was self-reported opioid pain medication use in 2016. Outcomes included incident limitations in ADL, IADL, and cognitive functioning in 2018. Statistical methods adjusted for confounding using multivariable logistic regressions, inverse probability of treatment weighting, and propensity scores.
Results
Opioid use (adjusted odds ratio [aOR]: 1.34, 95% confidence interval [CI] 1.07–1.68) was associated with a statistically significant higher odds of incident ADL limitation in multivariable regression and in propensity score adjustment (aOR: 1.41, 95% CI 1.13–1.76). The association between opioid use and ADL and IADL limitations was modified by age. Adults aged < 65 years had a higher odds of incident ADL (aOR: 1.83, 95% CI 1.38–2.42) and IADL (aOR: 1.42, 95% CI 1.06–1.90) limitations compared with those aged ≥ 65 years.
Conclusions
Community-dwelling adults using opioid analgesics to manage pain may be at risk for incident ADL limitations. Middle-aged adults, compared with those older than 65 years of age, experienced the greatest odds for incident ADL and IADL limitations following opioid use. According to sensitivity analyses, our findings were robust to unmeasured confounding.


Similar content being viewed by others
References
Dahlhamer J, et al. Prevalence of chronic pain and high-impact chronic pain among adults: United States, 2016. MMWR Morb Mortality Wkly Rep. 2018;67(36):1001–6. https://doi.org/10.15585/mmwr.mm6736a2.
Patel KV, et al. Prevalence and impact of pain among older adults in the United States: findings from the 2011 National Health and Aging Trends Study. Pain. 2013;154(12):2649–57. https://doi.org/10.1016/j.pain.2013.07.029.
Institute of Medicine. Relieving pain in America: a blueprint for transforming prevention, care, education, and research. Washington, DC: The National Academies Press; 2011. https://doi.org/10.3109/15360288.2012.678473.
Dahlhamer JM, Connor EM, Bose J, Lucas JW, Zelaya CE. Prescription opioid use among adults with chronic pain: United States, 2019. National Health Statistics Reports; no 162. Hyattsville, MD: National Center for Health Statistics. 2021. https://doi.org/10.15620/cdc:107641
Dowell D, Haegerich TM, Chou R. CDC guideline for prescribing opioids for chronic pain: United States, 2016. JAMA. 2016;315(15):1624–45. https://doi.org/10.1001/jama.2016.1464.
O’Neil CK, Hanlon JR, Marcum ZA. Adverse effects of analgesics commonly used by older adults with osteoarthritis: focus on non-opioid and opioid analgesics. Am J Geriatr Pharmacother. 2012;10(6):331–42. https://doi.org/10.1016/j.amjopharm.2012.09.004.
Volkow ND, McLellan AT. Opioid abuse in chronic pain: misconceptions and mitigation strategies. N Engl J Med. 2016;374(13):1253–63. https://doi.org/10.1056/NEJMra1507771.
Shah R, et al. Association of co-prescribing of opioid and benzodiazepine substitutes with incident falls and fractures among older adults: a cohort study. BMJ Open. 2021;11(12): e052057. https://doi.org/10.1136/bmjopen-2021-052057.
Drug Enforcement Administration, Department of Justice. Schedules of controlled substances: rescheduling of hydrocodone combination products from schedule III to schedule II. Final rule. Fed Regist. 2014;79(163):49661.
Kuo YF, et al. Opioid prescriptions in older medicare beneficiaries after the 2014 federal rescheduling of hydrocodone products. J Am Geriatr Soc. 2018;66(5):945–53. https://doi.org/10.1111/jgs.15332.
Liaw V, et al. Opioid prescribing among adults with disabilities in the United States after the 2014 Federal Hydrocodone Rescheduling Regulation. Public Health Rep. 2020;135(1):114–23. https://doi.org/10.1177/0033354919892638.
Scholl L, et al. Drug and opioid-involved overdose deaths: United States, 2013–2017. MMWR Morb Mortal Wkly Rep. 2019;67(5152):1419. https://doi.org/10.15585/mmwr.mm675152e1.
Chou R, et al. Opioid treatments for chronic pain comparative effectiveness review, vol. 229. Rockville: Agency for Healthcare Research and Quality (US); 2020. https://doi.org/10.23970/AHRQEPCCER229.
Sites BD, Beach ML, Davis MA. Increases in the use of prescription opioid analgesics and the lack of improvement in disability metrics among users. Reg Anesth Pain Med. 2014;39(1):6–12. https://doi.org/10.1097/AAP.0000000000000022.
Schnitzer TJ, et al. Efficacy of tramadol in treatment of chronic low back pain. J Rheumatol. 2000;27(3):772–8.
Steiner DJ, et al. Efficacy and safety of the seven-day buprenorphine transdermal system in opioid-naive patients with moderate to severe chronic low back pain: an enriched, randomized, double-blind, placebo-controlled study. J Pain Symptom Manag. 2011;42(6):903–17. https://doi.org/10.1016/j.jpainsymman.2011.04.006.
Veiga DR, et al. Effectiveness of opioids for chronic noncancer pain: a two-year multicenter, prospective cohort study with propensity score matching. J Pain. 2019;20(6):706–15. https://doi.org/10.1016/j.jpain.2018.12.007.
Sonnega A, et al. Cohort profile: the Health and Retirement Study (HRS). Int J Epidemiol. 2014;43(2):576–85. https://doi.org/10.1093/ije/dyu067.
Fonda S, Herzog AR. Documentation of physical functioning measured in the Health and Retirement Study and the asset and health dynamics among the Oldest Old Study. Ann Arbor: University of Michigan Survey Research Center; 2004.
Crimmins EM, et al. Assessment of cognition using surveys and neuropsychological assessment: the Health and Retirement Study and the Aging, Demographics, and Memory Study. J Gerontol B Psychol Sci Soc Sci. 2011;66(Suppl. 1):i162–71.
Katz S, et al. Studies of illness in the aged: the index of ADL: a standardized measure of biological and psychosocial function. JAMA. 1963;185(12):914–9. https://doi.org/10.1001/jama.1963.03060120024016.
Lawton MP, Brody EM. Assessment of older people: self-maintaining and instrumental activities of daily living. Gerontologist. 1969;9(3_Part_1):179–86.
Langa KM, et al. A comparison of the prevalence of dementia in the United States in 2000 and 2012. JAMA Intern Med. 2017;177(1):51–8. https://doi.org/10.1001/jamainternmed.2016.6807.
Tisnado DM, et al. What is the concordance between the medical record and patient self-report as data sources for ambulatory care? Med Care. 2006;44(2):132–40.
Steffick DE, Wallace RB, Herzog AR (2000) Documentation of affective functioning measures in the Health and Retirement Study. Ann Arbor, MI: University of Michigan.
Austin PC. Using the standardized difference to compare the prevalence of a binary variable between two groups in observational research. Commun Stat-Simul C. 2009;38(6):1228–34. https://doi.org/10.1080/03610910902859574.
Team R. RStudio: integrated development environment for R. Boston: RStudio, PBC; 2020.
DuGoff EH, Schuler M, Stuart EA. Generalizing observational study results: applying propensity score methods to complex surveys. Health Serv Res. 2014;49(1):284–303.
Lin DY, Psaty BM, Kronmal RA. Assessing the sensitivity of regression results to unmeasured confounders in observational studies. Biometrics. 1998;54(3):948–63.
Pollack SW, Skillman SM, Frogner BK. The health workforce delivering evidence-based non-pharmacological pain management. Seattle: University of Washington, Center for Health Workforce Studies; 2020.
Karmali RN, et al. The association between the supply of select nonpharmacologic providers for pain and use of nonpharmacologic pain management services and initial opioid prescribing patterns for Medicare beneficiaries with persistent musculoskeletal pain. Health Serv Res. 2021;56(2):275–88. https://doi.org/10.1111/1475-6773.13561.
Clark F, et al. Effectiveness of a lifestyle intervention in promoting the well-being of independently living older people: results of the well elderly 2 randomised controlled trial. J Epidemiol Community Health. 2012;66(9):782–90. https://doi.org/10.1136/jech.2009.099754.
Deandrea S, et al. Risk factors for falls in community-dwelling older people: a systematic review and meta-analysis. Epidemiology. 2010;21(5):658–68.
DeRigne L, Stoddard-Dare P, Quinn L. Workers without paid sick leave less likely to take time off for illness or injury compared to those with paid sick leave. Health Aff (Millwood). 2016;35(3):520–7. https://doi.org/10.1377/hlthaff.2015.0965.
Gaskin DJ, Richard P. The economic costs of pain in the United States. J Pain. 2012;13(8):715–24. https://doi.org/10.1016/j.jpain.2012.03.009.
Riffin C, et al. Multifactorial examination of caregiver burden in a national sample of family and unpaid caregivers. J Am Geriatr Soc. 2019;67(2):277–83. https://doi.org/10.1111/jgs.15664.
Clegg A, Young JB. Which medications to avoid in people at risk of delirium: a systematic review. Age Ageing. 2011;40(1):23–9. https://doi.org/10.1093/ageing/afq140.
Cherrier MM, et al. Comparative cognitive and subjective side effects of immediate-release oxycodone in healthy middle-aged and older adults. J Pain. 2009;10(10):1038–50. https://doi.org/10.1016/j.jpain.2009.03.017.
Whitlock EL, et al. Association between persistent pain and memory decline and dementia in a longitudinal cohort of elders. JAMA Intern Med. 2017;177(8):1146–53. https://doi.org/10.1001/jamainternmed.2017.1622.
Allegri N, et al. Systematic review and meta-analysis on neuropsychological effects of long-term use of opioids in patients with chronic noncancer pain. Pain Pract. 2019;19(3):328–43. https://doi.org/10.1111/papr.12741.
Kendall SE, et al. The cognitive effects of opioids in chronic non-cancer pain. Pain. 2010;150(2):225–30. https://doi.org/10.1016/j.pain.2010.05.012.
Giles GM, et al. Making functional cognition a professional priority. Am J Occup Ther. 2020;74(1):7401090010p1–6. https://doi.org/10.5014/ajot.2020.741002.
Esechie A, et al. Trends in prescribing pattern of opioid and benzodiazepine substitutes among Medicare part D beneficiaries from 2013 to 2018: a retrospective study. BMJ Open. 2021;11(11): e053487. https://doi.org/10.1136/bmjopen-2021-053487.
American Geriatrics Society Panel on the Pharmacological Management of Persistent Pain in Older Persons. Pharmacological management of persistent pain in older persons. J Am Geriatr Soc. 2009;57(8):1331–46. https://doi.org/10.1111/j.1532-5415.2009.02376.x.
Paice JA, et al. Management of chronic pain in survivors of adult cancers: American Society of Clinical Oncology clinical practice guideline. J Clin Oncol. 2016;34(27):3325–45. https://doi.org/10.1200/jco.2016.68.5206.
Gibson DC, et al. Risk of an opioid-related emergency department visit or hospitalization among older breast, colorectal, lung, and prostate cancer survivors. Mayo Clin Proc. 2022;97(3):560–70. https://doi.org/10.1016/j.mayocp.2021.08.030.
Vu JV, et al. Statewide implementation of postoperative opioid prescribing guidelines. N Engl J Med. 2019;381(7):680–2. https://doi.org/10.1056/nejmc1905045.
Simon AU, Collins CER. Lifestyle Redesign® for chronic pain management: a retrospective clinical efficacy study. Am J Occup Ther. 2017;71(4):7104190040p1–7. https://doi.org/10.5014/ajot.2017.025502.
Frogner BK, et al. Physical therapy as the first point of care to treat low back pain: an instrumental variables approach to estimate impact on opioid prescription, health care utilization, and costs. Health Serv Res. 2018;53(6):4629–46. https://doi.org/10.1111/1475-6773.12984.
Pritchard KT, Baillargeon J, Raji MA, Chou LN, Downer B, Kuo YF. Association of occupational and physical therapy with duration of prescription opioid use after hip or knee arthroplasty: a retrospective cohort study of medicare enrollees. Arch Phys Med Rehabil. 2021;102(7):1257–1266. https://doi.org/10.1016/j.apmr.2021.01.086.
Acknowledgements
We thank Sarah Toombs Smith, PhD, ELS (University of Texas Medical Branch), who aided in proofreading and editing the manuscript. She was not compensated for her contribution beyond her institutional salary.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
This study was supported with funding from the National Institutes on Drug Abuse R01DA039192, the National Institute on Aging K01AG058789 and P30-AG024832, the Agency for Healthcare Research and Quality T32HS02613301, and the National Center for Complementary and Integrative Health F31AT011856. The funders had no role in the design and conduct of the study, the collection, management, analysis, and interpretation of the data, the preparation, review, or approval of the manuscript, and the decision to submit the manuscript for publication.
Conflict of interest
The authors have no conflicts of interest that are directly relevant to the content of this article.
Ethics approval
The University of Michigan’s Institutional Review Board approved the Health and Retirement Study. No other approval was applicable.
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Availability of data and material
Health and Retirement Study [RAND HRS Longitudinal File]* public use dataset. Produced and distributed by the University of Michigan with funding from the National Institute on Aging (grant number NIA U01AG009740), Ann Arbor, MI, USA (2021).
Code availability
Not applicable.
Author contributions
Concept and design: all authors. Acquisition, analysis, or interpretation of data: all authors. Drafting of the manuscript: all authors. Critical revision of the manuscript for important intellectual content: all authors. Statistical analysis: BD, Y-FK, and KTP. Obtained funding: BD, Y-FK, MAR, and KTP. Supervision: JB and Y-FK.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Pritchard, K.T., Downer, B., Raji, M.A. et al. Incident Functional Limitations Among Community-Dwelling Adults Using Opioids: A Retrospective Cohort Study Using a Propensity Analysis with the Health and Retirement Study. Drugs Aging 39, 559–571 (2022). https://doi.org/10.1007/s40266-022-00953-y
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40266-022-00953-y