Abstract
Background
Although expanded access is an increasingly used pathway for patients to access investigational medicine, little is known on the magnitude and content of published scientific research collected via expanded access.
Methods
We performed a review of all peer-reviewed expanded access publications between January 1, 2000 and January 1, 2022. We analyzed the publications for drugs, diseases, disease area, patient numbers, time, geographical location, subject, and research methodology (single center/multicenter, international/national, prospective/retrospective). We additionally analyzed endpoints reported in all COVID-19-related expanded access publications.
Results
We screened 3810 articles and included 1231, describing 523 drugs for 354 diseases for 507,481 patients. The number of publications significantly increased over time (\(p<0.001\)). Large geographical disparities existed as Europe and the Americas accounted for 87.4% of all publications, whereas Africa only accounted for 0.6%. Oncology and hematology accounted for 53% of all publications. Twenty-nine percent of all expanded access patients (N = 197,187) reported on in 2020 and 2021 were treated in the context of COVID-19.
Conclusions
By summarizing characteristics of patients, diseases, and research methods described in all scientific literature published on expanded access, we provide a unique dataset for future research. We show that published scientific research on expanded access has surged over the past decades, partly due to COVID-19. However, international collaboration and equity in geographic access remain an issue of concern. Lastly, we stress the need for harmonization of research legislation and guidance on the value of expanded access data within real-world data frameworks to improve equity in patient access and streamline future expanded access research.
Similar content being viewed by others
We provide a unique dataset for future research by summarizing characteristics of patients, diseases, and research methods described in all scientific literature published on expanded access. |
We show that published scientific research on expanded access has surged over the past decades, partly due to COVID-19. |
We provide a systematic analysis of endpoints reported in COVID-19-related expanded access publications. |
International collaboration and equity in geographic access remain an issue of concern. |
1 Introduction
Patients who cannot be adequately treated with marketed therapies and who simultaneously are unable or ineligible to enroll in clinical trials may seek different means of accessing unlicensed treatments. Legislators have created “expanded access” pathways to allow these patients to access unregistered medicines [1]. The US Food and Drug Administration (FDA) institutionalized “expanded access” in 1987 in efforts to provide more treatment options for patients with acquired immunodeficiency syndrome (AIDS) [2]. The European Medicines Agency (EMA) has drafted guidance on compassionate use in 2007, but individual members states of the European Union (EU) have a longer history of individually regulating national “expanded access pathways,” and still retain that freedom today [3].
The primary intent of expanded access programs is to provide treatment access, which contrasts with the primary intent of research in clinical trials. Nonetheless, there is an increasing interest in simultaneously providing access whilst collecting, analyzing, and disseminating results from expanded access usage. First, these data may further estimate treatment patterns and outcomes in non-trial (e.g., “real-world”) patients [4, 5]. Second, including expanded access may increase statistical precision simply by increasing patient numbers—this pertains particularly to expanded access use of rare diseases drugs [3, 6]. While various regulators in the EU and USA mandate some form of data collection during expanded access, others restrict or even prohibit the collection and subsequent analysis [7]. To date, opinions differ to what extent data collection under expanded access is feasible, desirable, and reliable.
The evidence that stems from expanded access has been used to inform safety and efficacy labels by regulatory bodies such as the FDA and EMA [8]. Furthermore, data from expanded access are incorporated by health technology assessment bodies to determine cost-effectiveness of novel therapies in the UK, the Netherlands, the USA, and France [9]. To what degree data from expanded access of investigational medicine are published in academic literature remains unknown. A mapping of expanded access scholarship with regards to time, location, subject, research methodology, and authorship is lacking. There is no information on which drugs are used in expanded access literature, by how many patients, for which diseases, and where such expanded access programs take place.
Here, we examine to what extent research on expanded access is disseminated in the academic literature. Furthermore, we analyze the type, subject, and participants within such research. We identify disparities in scientific research across geographies and disease areas and discuss the resultant issue of access inequality. Lastly, we provide recommendations on the harmonization of expanded access research in the future and facilitate such research by the dataset created in this work.
2 Methods
We conducted a review of all publications indexed in MEDLINE through PubMed that report original results of expanded access usage. We included all peer-reviewed literature that was published between January 1, 2000 and January 1, 2022. All articles that included any term related to expanded access (e.g., compassionate use, pre-approval access, managed access, special access) were considered [10]. We relied on the self-assessed classification of expanded access by the authors and removed all instances with an erroneous expanded access classification, e.g., off-label use and clinical trials, where possible. The detailed search protocol is available in the Supplementary Material.
2.1 Citation and Review Management
All citations were exported from PubMed in EndNote Version 19 (Clarivate, London, UK), where duplicates and publications without full text were detected and removed. Citations were subsequently uploaded in Rayyan, an online systematic review platform [11]. T.B.P., D.G.J.C., N.A., and S.S.A. independently conducted the review—all records were reviewed at least twice. A random sample of 100 articles was additionally assessed by a third independent reviewer.
2.2 Eligibility, Screening, and Labeling
Based on the titles and abstract, we labeled articles for “inclusion,” “exclusion,” or further investigation (“unknown”). Articles labeled “unknown” or where reviewers disagreed on inclusion/exclusion were further assessed by reading the full text. If the third reviewer was unsure, remaining disagreement was solved through discussion of the full text with a fourth author. Exclusion reasons included:
-
1.
Non-English literature
-
2.
Not relevant (topic is not expanded access, e.g., off-label use or formal clinical trials)
-
3.
Not primary research
-
Errata, editorials, replies
-
News articles
-
Meta-analyses, guidelines, systematic reviews
-
4.
Not disseminating investigational results of pharmaceutical therapeutics
-
Devices, procedures
-
Other research topics (e.g., legal/ethical/policy issues)
Subsequently, we analyzed the full-text articles for the following predefined main outcomes: time of publication, research location (country, national/international, single center/multi-center), number of patients, research methodology (retrospective/prospective), drug, disease, and disease area. To provide the reader with insights that cannot be generalized across disease areas, and since expanded access gained particular attention during the COVID-19 pandemic, we specifically provide more detailed information on all COVID-19 related expanded access articles, including systematic analysis of all endpoints used (see Supplementary Material).
Our screening procedure was tested on 50 abstracts prior to the start of the review. The detailed protocol is provided in the Supplementary Material. To give the reader more insight into the content of expanded access publications, we describe ten randomly selected articles in detail in the Supplementary Material. We cover the expanded access research setup, patient numbers, intervention, outcomes, and author interpretation of the results, including comparison with formal clinical trial results.
2.3 Data Management and Statistics
A chart was created in Microsoft Excel 2010 (Microsoft, Redmond, WA) to tabulate the main outcome characteristics. We subsequently analyzed the data in R version 4.0.1 (PBC, Boston, MA), and code was generated to detect implausible values that were subsequently examined by the reviewers. The code to replicate this study is available on the GitHub of the first author.Footnote 1 We used descriptive statistics to summarize our findings. To detect trends across time in the number of publications, we used a Spearman rank correlation test with a two-sided significance level of 0.05.
3 Results
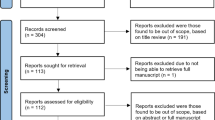
We examined 3820 publications. After removing duplicates (n = 10) and articles without full text (n = 32), we screened 3778 records for eligibility. We excluded articles not written in English (n = 184) and not concerning expanded access (n = 1333). Finally, errata, replies, and editorials (n = 101), news articles (n = 50), or meta-analyses, systematic reviews, and guidelines (n = 478) were removed. This led us to a collection of primary research on expanded access. We further removed nonpharmacological therapeutic articles, e.g., research on devices and procedures (n = 133), and research on the legal, ethical, or policy aspects of expanded access (n = 150). A schematic overview can be found in Fig. 1.
The reviewers agreed directly in 89.2% of the cases. Three reviewers reviewed 10.4% cases and four reviewers reviewed 1.5% of all cases (including a random sample review of 100 articles). T.B.P. reviewed all 3810 publications, followed by D.G.J.C. (N = 1847), S.S.A. (N = 1843), and N.K. (N = 631). The review was conducted in May and June 2022.
The number of publications over time is depicted in Fig. 2. We observe an increasing trend over time: from 12 therapeutic investigation publications in 2000 to 175 in 2021, (\(\rho\) = 0.96, p < 0.001).
The descriptive statistics are provided in Table 1. The median number of patients described was 43, but this number varied widely, ranging from N = 1 in case reports to N = 95,000. Case reports comprised almost 1 in 8 (12.3%) publications. Of the non-case report publications (i.e., N > 1), the median number of patients was 57, with an interquartile range (IQR) of 18–198 patients. Most of the data had been collected retrospectively (51%), and only 12.1% (149/1231) of all publications were international collaborations. For national (single-country) publications (n = 1082), the majority (51.1%) were collaborative publications between multiple hospitals. Most studies only included adults; 22% included mixed populations with both adults and children, or children only. Researchers in the USA generated the most publications in absolute terms (22.1%, 240/1082), followed by Italy (16.9%, 183/1082) and France (8.3%, 90/1082), see Table 2. When we calculated the number of publications relative to the average populations (in millions) from these countries during the midpoint of the time period (2006–2016), Italy had the highest output per capita, with 3.1 articles per million inhabitants. Italy is followed by Belgium and Spain, with relative publication outputs of 2.5 and 1.8 per million inhabitants, respectively. Table 2 presents the geographic distribution of the top ten most productive regions in terms of expanded access publications. Europe and the Americas accounted for 87.4% of all publications, whereas Africa only accounted for 0.6%. High-income regions (north/south/west Europe and northern America) comprised 82.5% of all publications and 92.4% of all patients described in our dataset (Fig. 3).
As the results described in this section aim to abstract information across drugs and conditions, the reader that is interested in a more detailed description of expanded access publications can find an analysis of ten randomly selected articles in the Supplementary Material. This sample demonstrates the heterogeneity of our dataset across a variety of quantitative variables such as sample size, study design, geographic region, patient populations, and expanded access program (EAP) duration. However, the articles also differ on qualitative aspects. Some authors discuss at length the differences between the patients in the EAP and the clinical trials and how these differences may result in different outcomes. Other authors are unable to report on such trial—EAP differences, as disparities in sample sizes may prevent a useful comparison (e.g., case reports). Additionally, trial results may simply be unavailable for the product while expanded access was provided, as trials might have been ongoing or not even initiated.
3.1 Disease Areas
The 1231 publications covered 354 unique diseases across 18 disease areas. The top ten most frequently appearing disease areas are depicted in Fig. 4. The two largest areas, oncology 39.6% (488/1231) and hematology 13.8% (170/1231), are further broken down per top ten most frequent diseases. Note that a single publication can cover multiple diseases (this is the case in 38 publications), for example, where a single drug is tested in adjacent diseases, such as expanded access of azacitidine to treat patients with both acute myeloid leukemia and myelodysplastic syndromes [12,13,14]. Other instances include diseases sharing a common actionable target such as ErbB2/HER2 in breast and colorectal cancer and malignant melanoma [15].
3.2 Pharmacological Therapeutics
A total of 523 unique pharmacological therapeutics were described in our dataset. Eighty-seven publications covered more than one therapeutic. The top ten most frequently appearing drugs are depicted in Table 3. Nivolumab was the most frequently appearing drug, likely due to its use in a variety of solid tumors (non-small cell lung cancer, glioblastoma, renal cell carcinoma) and non-solid tumors (Hodgkin lymphoma), as well as its use in combination therapy for melanoma with ipilimumab. There may also be one drug indication pair featuring a multiplicity of publications. In the case of cabazitaxel, a chemotherapy for castrate-resistant prostate cancer, there are individual expanded access publications from single centers [16], various single-country publications in Europe [17,18,19], and a Europe-wide publication [20]. Furthermore, these 15 publications focus on different aspects of the treatment, such as safety [21] or quality of life [22].
3.3 The Effects of the COVID-19 Pandemic
The steep increase in publications in recent years can partially be attributed to the COVID-19 pandemic. In 2020 and 2021, a large portion of publications was dedicated to medicine that could potentially treat COVID-19 infections: 29% (39/136) in 2020 and 29% (50/175) in 2021. Similarly, 49% (87/176) of expanded access publications on infectious diseases are related to COVID-19.
The pandemic boosted publications on potential treatments such as convalescent plasma (N = 15), remdesivir (N = 14), and tocilizumab (N = 11). The publications on the use of convalescent plasma to potentially treat COVID-19 infections comprised 194,256 patients, shifting the distribution of patient numbers on its own. We systematically extracted and grouped all endpoints reported in COVID-19 related publications. The 42 unique endpoints are not limited to mandatory safety monitoring: The five most frequently described endpoints in COVID-19 publications were adverse events (57%), mortality (45%), inflammatory markers (34%), oxygen support (32%), and clinical improvement (26%) (Table 4, see Supplementary Material for a complete overview of all used endpoints). In total, 41 unique drugs have been provided under compassionate use to treat COVID-19. Of these, four drugs received EMA approval, and five drugs are authorized for use by the FDA (in part under emergency use), as of January 2023 [23]. The submission to the EMA for the FDA-approved agent baricitinib was withdrawn by the applicant [24].
4 Discussion
In this paper, we have mapped the landscape of expanded access publications from January 1, 2000 to January 1, 2022. To the best of our knowledge, this is the first literature review of expanded access publications to assess drugs, diseases, patient numbers, and research methods. We have identified 1632 original investigations of expanded access, of which 1231 focus on pharmacological therapeutics, and the number of publications increases significantly over time. The increase in publications reflects a general increase in attention for expanded access, as reported by regulators, industry, and through other scholars. Our work provides the first annotated dataset that yields insights into how many patients contributed to the peer-reviewed scientific literature through expanded access programs, across diseases, geographies, and drugs.
The geographic distribution of expanded access publications highlights the disparity in the availability of investigational medicine. High-income countries produce more publications compared with low-income countries, which may be partly explained by excluding non-English literature, but may also be attributed to manufacturer and scientific willingness to provide expanded access and facilitate subsequent research. Our findings reflect the limited access to medicine in developing countries in general, but to investigational medicine in particular—an issue worth exploring in future research.
The differences between countries within the EU may be due to differences in regulatory preferences. Italy, with the highest number of publications per capita, is more liberal in allowing data collection compared with countries such as Sweden and Finland [3]. The variance in allowing expanded access programs to generate evidence among European regulators has created a maze of national pathways for manufacturers to navigate [7]. Such complexity may provoke reluctance from drug manufacturers to provide expanded access in the first place, which may impede rather than facilitate equity in patient access.
The largest share of expanded access research is devoted to oncology and (malignant) hematology, accounting for 53.5% publications. This is driven in part by the large unmet medical need of cancer patients, as well as the abundance of trials in these areas. Furthermore, regulators offer specific guidance for expanded access to oncology (for example, through the FDA’s Project Facilitate) [25], educating oncologists and expediting access to anticancer drugs.
Our findings seem to support the position that, indeed, expanded access programs can be used to collect data that can further the knowledge on an investigational medicine. The stance of some regulators (e.g., Sweden, Finland, Canada) that data collection within an EAP is prohibited (or discouraged), in part over fears of data quality or companies attempting to bypass trial regulations [3, 26, 27], seems to be at odds with the numbers of publications from those countries (n = 13, n = 5, n = 56, respectively). The number of expanded access publications show that the treatment of patients with investigational medicine is, in itself, being used as a means to support (ongoing) investigations.
Nonetheless, the analyses of expanded access data should be interpreted with caution. Expanded access data are nonblinded, nonrandomized data, and as such may be inherently confounded. These “real-world” data may harbor serious data quality issues. Furthermore, expanded access data may suffer even more quality loss, as 50.9 % of the reports in our sample collected data retrospectively. This may severely impact data quality, although main parameters (such as survival) should be straightforward to gather. In our analysis of endpoints used in EAPs for COVID-19, we found that data is collected beyond mandatory safety reporting. Endpoints included various clinical improvement ratings/scales, respiratory or oxygen support status, duration of hospitalization, viral load, and patient-reported outcomes, among others. The heterogeneity of research methods and endpoints makes it difficult to compare studies.
Ideally, an EAP should include a prespecified, prospective data collection to ensure highest data quality that is fit for purpose. Although the inclusion of expanded access data (and other sources of real-world data) in regulatory decision-making is increasing [8, 28, 29], the lack of oversight could contribute to suboptimal data quality and hesitance of regulatory bodies to include said data in decision-making processes. To expand the application of expanded access data beyond peer-reviewed publications, it is important to develop minimal data quality standards for expanded access studies in the future [30].
Harmonization on publications may be an area of potential development. Some expanded access programs harbor “salami tactics,” i.e., there are different publications per center, then per region, then per country, and subsequently, a synthesized international publication [16,17,18,19,20]. Additionally, the basis of a new publication may not be a different geographic location, but rather a different (sub)topic, publishing separately on safety [21], efficacy, and/or quality-of-life [22]. Although we acknowledge that the lack of observational research harmonization across countries impedes international collaboration, we question the incremental added value of each of these single publications as opposed to several large, overarching, international publications. As local investigators may not be aware of all scientific endeavors worldwide, drug manufacturers should better coordinate local efforts by connecting researchers across regions.
The impact of COVID-19 on the expanded access landscape is remarkable. Early in the pandemic, various authors cautioned against the widespread use of medication outside of clinical trials as randomized trials would be “the only way to find effective and safe treatments for COVID-19” [26]. Indeed, the results from the large-scale expanded access program of convalescent plasma in the USA later failed to replicate in various randomized trials [31,32,33,34]. Although we agree that the place for expanded access is in addition to clinical trials rather than instead of, there is a place for expanded access in facilitating serendipitous findings, especially in the field of rare diseases. Evidence of expanded access can be used in addition to clinical trials to explore the safety and effectiveness of medicines used in different populations, or in (slightly) different indications (for example, in the case of cancer therapies targeting the same genetic aberration in a different histology). The drawback of expanded access data collection does not imply that these data are worthless or that no data ought to be collected; we, together with other scholars [4, 6], believe that the treatment of a patient with investigational medicine should always be used to further the understanding of the potential benefits and risks of investigational medicine [30].
5 Limitations and Future Research
First, we attempted to differentiate expanded access programs from other types of access to unregistered products, such as trials, compounded medication, or off-label usage. To label a paper as “expanded access” or not, we primarily relied on the self-reported use of “expanded access,” i.e., if the authors (and editors or peer-reviewers) approved the term “expanded access.” Nonetheless, an exact definition of expanded access varies per jurisdiction. A strict interpretation of expanded access is “nontrial access to pre-approval medicine”—yet these programs can also be used after a product has been withdrawn from the market (post-withdrawal rather than pre-approval), or to bridge the gap between marketing authorization and reimbursement (post-approval, pre-reimbursement). In addition, the term expanded access is sometimes used to denote off-label usage or “compassionate use trials.” To prevent erroneous inclusion of (randomized) trials or off-label usage, we used an independent review process and deliberated in case of doubt. Note that the interchangeable usage of expanded access and off-label is not wrong per se: some countries employ a the same terminology and pathways for expanded access as for off-label usage. Most forms of off-label usage differ considerably from “expanded access,” in other instances, these concepts may be inherently related.
Second, we only focused on peer-reviewed publications indexed in PubMed that were written in English and included “expanded access” related terms. As such, we have missed both non-English publications and literature that did not incorporate these terms. Other ways of disseminating expanded access results, such as poster or oral presentations at scientific conferences have not been investigated in our work. The use of additional databases (e.g., Embase) could have resulted in more publications. Therefore, our work may underestimate the number of expanded access publications, drugs, and patients over the past two decades. Furthermore, not all expanded access programs will result in publications, and the number of publications is potentially only a proxy for the total number of expanded access programs.
Further research could focus on the bias (quality) of expanded access publications or could further explore differences between trial and expanded access publications. This concerns both patient demographics, i.e., are “expanded access” patients really more “real world” than trial patients?, as well as clinical outcomes, i.e., are expanded access patients potentially worse off than trial patients?
6 Conclusions
The increasing interest in access to investigational medicine is reflected by a rise in the number of publications of expanded access programs from 2000 to 2019 and amplified by the COVID-19 pandemic through 2020 and 2021. The 1231 publications identified in this review shed a novel light on the characteristics of patients, diseases, and research methods of expanded access programs. Harmonization of research legislation and guidance on the value of expanded access data within real-world data frameworks should ensure that patients in expanded access programs globally contribute efficiently to scientific evidence.
References
Caplan A, Bateman-House A. Compassion for each individual’s own sake. Am J Bioethics. 2014;14:16–7.
Darrow JJ, Sarpatwari A, Avorn J, Kesselheim AS. Practical, legal, and ethical issues in expanded access to investigational drugs. Hamel MB, editor. N Engl J Med. 2015;372:279–86.
Polak TB, Cucchi DGJ, van Rosmalen J, Uyl-de Groot CA, Darrow JJ. Generating evidence from expanded access use of rare disease medicines: challenges and recommendations. Front Pharmacol. 2022;13:913567.
Rozenberg O, Greenbaum D. Making it count: extracting real world data from compassionate use and expanded access programs. Am J Bioethics. 2020;20:89–92.
Polak TB, van Rosmalen J, Uyl-De Groot CA. Response to open peer commentary "making it count: extracting real world data from compassionate use and expanded access programs". Am J Bioeth. 2020;20(11):W4–W5.
Chapman CR, Moch KI, McFadyen A, Kearns L, Watson T, Furlong P, et al. What compassionate use means for gene therapies. Nat Biotechnol. 2019;37:352–5.
Polak TB, Cucchi DGJ, van Rosmalen J, Uyl-de Groot CA. The DRUG Access Protocol: access inequality and European harmonisation. Lancet Oncol. 2022;23: e202.
Polak TB, van Rosmalen J, Uyl-de Groot CA, Rosmalen J, Uyl-de Groot CA. Expanded access as a source of real-world data: an overview of FDA and EMA approvals. Br J Clin Pharmacol. 2020;86:1819–26.
Polak TB, Cucchi DG, van Rosmalen J, Uyl-de Groot CA. Real-world data from expanded access programmes in health technology assessments: a review of NICE technology appraisals. BMJ Open. 2022;12: e052186.
Kimberly LL, Beuttler MM, Shen M, Caplan AL, Bateman-House A. Pre-approval access terminology: a cause for confusion and a danger to patients. Ther Innov Regul Sci. 2017;51:494–500.
Ouzzani M, Hammady H, Fedorowicz Z, Elmagarmid A. Rayyan—a web and mobile app for systematic reviews. Syst Rev. 2016;5:210.
van der Helm LH, Alhan C, Wijermans PW, van Marwijk KM, Schaafsma R, Biemond BJ, et al. Platelet doubling after the first azacitidine cycle is a promising predictor for response in myelodysplastic syndromes (MDS), chronic myelomonocytic leukaemia (CMML) and acute myeloid leukaemia (AML) patients in the Dutch azacitidine compassionate named p. Br J Haematol. 2011;155:599–606.
Estey E, Hasserjian RP, Döhner H. Distinguishing AML from MDS: a fixed blast percentage may no longer be optimal. Blood. 2022;139:323–32.
Duetz C, Cucchi DGJ, Polak TB, Janssen JJWM, Ossenkoppele GJ, Estey EH, et al. The wider perspective: twenty years of clinical trials in myelodysplastic syndromes. Br J Haematol. 2022;196(2):329–35.
Azemar M, Djahansouzi S, Jäger E, Solbach C, Schmidt M, Maurer AB, et al. Regression of cutaneous tumor lesions in patients intratumorally injected with a recombinant single-chain antibody-toxin targeted to ErbB2/HER2. Breast Cancer Res Treat. 2003;82:155–64.
Di Lorenzo G, D’Aniello C, Buonerba C, Federico P, Rescigno P, Puglia L, et al. Peg-filgrastim and cabazitaxel in prostate cancer patients. Anticancer Drugs. 2013;24:84–9.
Heidenreich A, Scholz HJ, Rogenhofer S, Arsov C, Retz M, Müller SC, et al. Cabazitaxel plus prednisone for metastatic castration-resistant prostate cancer progressing after docetaxel: results from the German compassionate-use programme. Eur Urol. 2013;63:977–82.
Wissing MD, van Oort IM, Gerritsen WR, van den Eertwegh AJ, Coenen JL, Bergman AM, et al. Cabazitaxel in patients with metastatic castration-resistant prostate cancer: results of a compassionate use program in the Netherlands. Clin Genitourin Cancer. 2013;11:238-250.e1.
Wissing MD, Van Oort IM, Gerritsen WR, van den Eertwegh AJ, Coenen JL, Bergman AM, et al. Final quality of life and safety data for patients with metastatic castration-resistant prostate cancer treated with cabazitaxel in the UK Early Access Programme (EAP) (NCT01254279). Asia Pac J Clin Oncol. 2013;13:975–83.
Heidenreich A, Bracarda S, Mason M, Ozen H, Sengelov L, Van Oort I, et al. Safety of cabazitaxel in senior adults with metastatic castration-resistant prostate cancer: results of the European compassionate-use programme. Eur J Cancer. 2014;50:1090–9.
Castellano D, Antón Aparicio LM, Esteban E, Sánchez-Hernández A, Germà JR, Batista N, et al. Cabazitaxel for metastatic castration-resistant prostate cancer: safety data from the Spanish expanded access program. Expert Opin Drug Saf. 2014;13:1165–73.
Parente P, Ng S, Parnis F, Guminski A, Gurney H. Cabazitaxel in patients with metastatic castration-resistant prostate cancer: safety and quality of life data from the Australian early access program. Asia Pac J Clin Oncol. 2017;13:391–9.
Treatments and vaccines for COVID-19 | European Medicines Agency [Internet]. [cited 2023 Jan 8]. Available from: https://www.ema.europa.eu/en/human-regulatory/overview/public-health-threats/coronavirus-disease-covid-19/treatments-vaccines-covid-19.
Know Your Treatment Options for COVID-19 | FDA [Internet]. [cited 2023 Jan 8]. Available from: https://www.fda.gov/consumers/consumer-updates/know-your-treatment-options-covid-19.
Scepura B, Chan M, Kim T, Boehmer J, Goldberg KB, Pazdur R. Oncology expanded access and FDA’s Project facilitate. Oncologist. 2021;26:e1880–2.
Kalil AC. Treating COVID-19-off-label drug use, compassionate use, and randomized clinical trials during pandemics. JAMA. 2020;323(19):1897–8.
BASG. Information on named patient use (Heilversuch) in Austria—definition and framework. Vienna; 2015.
Bakker E, Plueschke K, Jonker CJ, Kurz X, Starokozhko V, Mol PGM. Contribution of real-world evidence in european medicines agency's regulatory decision making. Clin Pharmacol Ther. 2023;113(1):135–51.
Purpura CA, Garry EM, Honig N, Case A, Rassen JA. The role of real-world evidence in FDA-approved new drug and biologics license applications. Clin Pharmacol Ther. 2022;111(1):135–44.
Polak TB, Fernandez LH. The ethics of expanded access research. JAMA. 2023;329:1057.
Budhai A, Wu AA, Hall L, Strauss D, Paradiso S, Alberigo J, et al. How did we rapidly implement a convalescent plasma program? Transfusion. 2020;60:1348–55.
Joyner MJ, Carter RE, Senefeld JW, Klassen SA, Mills JR, Johnson PW, et al. Convalescent plasma antibody levels and the risk of death from Covid-19. N Engl J Med. 2021;384:1015–27.
Kunze KL, Johnson PW, van Helmond N, Senefeld JW, Petersen MM, Klassen SA, et al. Mortality in individuals treated with COVID-19 convalescent plasma varies with the geographic provenance of donors. Nat Commun. 2021;12:4864.
Liu M, Chen Z, Dai MY, Yang JH, Chen XB, Chen D, et al. Lessons learned from early compassionate use of convalescent plasma on critically ill patients with COVID-19. Transfusion. 2020;60:2210–6.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
CAU-dG has received unrestricted grants from Boehringer Ingelheim, Astellas, Celgene, Sanofi, Janssen-Cilag, Bayer, Amgen, Genzyme, Merck, Glycostem Therapeutics, Astra Zeneca, Roche, and Merck. TBP works part-time for expanded access service provider myTomorrows, in which he holds stock and stock options (< 0.01%). He is contractually free to publish, and the service provider is not involved in any of his past or ongoing research, nor in this manuscript. DGJC received payments for lectures for Takeda, and conference visit support from Servier, all outside the submitted work. JS, SSA, NK, and JVR do not report any conflicts of interest.
Funding
CAU-dG, JvR and TBP work on a Dutch government grant from HealthHolland. For this grant, they research legal, ethical, policy, and statistical issues of evidence generation in expanded access programs (EMCLSH20012). HealthHolland is a funding vehicle for the Dutch Ministry of Economic Affairs and Climate Policy that addresses the Dutch Life Sciences & Health sector.
Ethics approval
This research does not meet the criteria to qualify as medical research with human subjects and is hence exempt from ethics approval in the Netherlands.
Informed consent
This research does not include research with (human) subjects and therefore does not require informed consent.
Data availability
All code to replicate our findings can be found on the GitHub of the main authorFootnote 2. Aggregated data are available upon reasonable request.
Author contributions
TBP conceived the idea for this review. TBP, DGJC, SSA, JS, and NK collected and labeled the data. TBP and JvR performed the statistical analysis. TBP drafted the manuscript. DGJC, JvR, and CAU-dG critically revised the manuscript. All authors approved the final version of the manuscript.
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Code availability
Not applicable.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Polak, T.B., Cucchi, D.G.J., Schelhaas, J. et al. Results from Expanded Access Programs: A Review of Academic Literature. Drugs 83, 795–805 (2023). https://doi.org/10.1007/s40265-023-01879-4
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40265-023-01879-4