Abstract
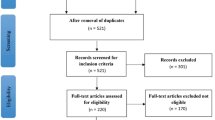
Kratom (Mitragyna speciosa) leaves contain the mu opioid partial agonists mitragynine and 7-hydroxymitragynine. The US Drug Enforcement Agency considers it a ‘drug of concern’, and the US FDA is reviewing kratom, but there is a paucity of information regarding health effects. Liver injury is often cited as a potential health consequence, however the same few case reports are repeatedly referenced, without a broader context. Furthermore, reports have largely lacked standardized causality assessment methods. The objective is to evaluate causality in kratom liver injury, through a comprehensive scoping review of human cases, and by reviewing epidemiologic, animal, and mechanistic reports that relate to kratom liver injury. Hepatotoxicity causality was systematically examined using the Roussel Uclaf Causality Assessment Method (RUCAM) for case reports. Biopsy findings, potential pathophysiologic mechanisms, and management options are discussed. This review identified 26 case reports and abstracts, in addition to 7 cases reported from the Drug-Induced Liver Injury Network, 25 in FDA databases, and 27 in internet user forums. Latency periods to symptom onset had a median of 20.6 days and mean of 21 days (range 2–49). Common presenting signs and symptoms were abdominal discomfort, jaundice, pruritis, and dark urine. Histologic findings were predominantly cholestatic, although, biochemically, the condition was heterogenous or mixed; the median R ratio was 3.4 and the mean was 4.6 (range 0.24–10.4). Kratom likely causes liver injury based on the totality of low-quality human evidence, and, in the context of epidemiologic, animal, and mechanistic studies. It remains unclear which subgroups of users are at heightened risk.
Similar content being viewed by others
References
Kruegel AC, Madalee GM, Kapoor A, Váradi A, Majumdar S, Filizola M, et al. Synthetic and receptor signaling explorations of the mitragyna alkaloids: mitragynine as an atypical molecular framework for opioid receptor modulators. J Am Chem Soc. 2016;138(21):6754–64.
Warner ML, Kaufman NC, Grundmann O. The pharmacology and toxicology of kratom: from traditional herb to drug of abuse. Int J Legal Med. 2016;130(1):127–38.
Smith KE, Lawson T. Prevalence and motivations for kratom use in a sample of substance users enrolled in a residential treatment program. Drug Alcohol Depend. 2017;180:340–8.
Post S, Spiller HA, Chounthirath T, Smith GA. Kratom exposures reported to United States poison control centers: 2011–2017. Clin Toxicol. 2019;57(10):847–54.
Trakulsrichai S, Tongpo A, Sriapha C, Wongvisawakorn S, Rittilert P, Kaojarern S, et al. Kratom abuse in ramathibodi Poison Center, Thailand: a five-year experience. J Psychoact Drugs. 2013;45(5):404–8.
Griffin OH, Webb ME. The scheduling of kratom and selective use of data. J Psychoact Drugs. 2018;50(2):114–20.
US FDA. FDA and Kratom. https://www.fda.gov/news-events/public-health-focus/fda-and-kratom. Accessed 25 Apr 2019.
US Drug Enforcement Administration. Kratom. https://www.dea.gov/factsheets/kratom. Accessed 1 Nov 2019.
Mosedale M, Watkins PB. Drug-induced liver injury: advances in mechanistic understanding that will inform risk management. Clin Pharmacol Ther. 2017;101(4):469–80.
Naranjo CA, Busto U, Sellers EM, Sandor P, Ruiz I, Roberts EA, et al. A method for estimating the probability of adverse drug reactions. Clin Pharmacol Ther. 1981;30(2):239–45.
Maria VA, Victorino RM. Development and validation of a clinical scale for the diagnosis of drug-induced hepatitis. Hepatology. 1997;26(3):664–9.
Takikawa H, Takamori Y, Kumagi T, Onji M, Watanabe M, Shibuya A, et al. Assessment of 287 Japanese cases of drug induced liver injury by the diagnostic scale of the International Consensus Meeting. Hepatol Res. 2003;27(3):192–5.
Hayashi PH. Drug-induced liver injury network causality assessment: criteria and experience in the United States. Int J Mol Sci. 2016;17(2):201.
Danan G, Benichou C. Causality assessment of adverse reactions to drugs—I. A novel method based on the conclusions of international consensus meetings: application to drug-induced liver injuries. J Clin Epidemiol. 1993;46(11):1323–30.
Rockey DC, Seeff LB, Rochon J, Freston J, Chalasani N, Bonacini M, et al. Causality assessment in drug-induced liver injury using a structured expert opinion process: comparison to the Roussel-Uclaf causality assessment method. Hepatology. 2010;51(6):2117–266.
Benichou C, Danan G, Flahault A. Causality assessment of adverse reactions to drugs—II. An original model for validation of drug causality assessment methods: case reports with positive rechallenge. J Clin Epidemiol. 1993;46(11):1331–6.
Danan G, Teschke R. RUCAM in drug and herb induced liver injury: the update. Int J Mol Sci. 2016;17(1):14–46.
Danan G, Teschke R. Roussel uclaf causality assessment method for drug-induced liver injury: present and future. Front Pharmacol. 2019;10:853.
García-Cortés M, Stephens C, Lucena MI, Fernández-Castañer A, Andrade RJ. Causality assessment methods in drug induced liver injury: strengths and weaknesses. J Hepatol. 2011;55(3):683–91.
Shapiro MA, Lewis JH. Causality assessment of drug-induced hepatotoxicity: promises and pitfalls. Clin Liver Dis. 2007;11(3):477–505.
Rochon J, Protiva P, Seeff LB, Fontana RJ, Liangpunsakul S, Watkins PB, et al. Reliability of the Roussel Uclaf causality assessment method for assessing causality in drug-induced liver injury. Hepatology. 2008;48(4):1175–83.
Teschke R, Frenzel C, Schulze J, Eickhoff A. Herbal hepatotoxicity: challenges and pitfalls of causality assessment methods. World J Gastroenterol. 2013;19(19):2864–82.
Suwanlert S. A study of kratom eaters in Thailand. Bull Narc. 1975;27(3):21–7.
Ahmad K, Aziz Z. Mitragyna speciosa use in the northern states of Malaysia: a cross-sectional study. J Ethnopharmacol. 2012;141(1):446–50.
Singh D, Müller CP, Murugaiyah V, Hamid SBS, Vicknasingam BK, Avery B, et al. Evaluating the hematological and clinical-chemistry parameters of kratom (Mitragyna speciosa) users in Malaysia. J Ethnopharmacol. 2018;214:197–206.
Cumpston KL, Carter M, Wills BK. Clinical outcomes after Kratom exposures: a poison center case series. Am J Emerg Med. 2018;36(1):166–8.
Kapp FG, Maurer HH, Auwärter V, Winkelmann M, Hermanns-Clausen M. Intrahepatic cholestasis following abuse of powdered kratom (Mitragyna speciosa). J Med Toxicol. 2011;7(3):227–31.
Dorman C, Wong M, Khan A. Cholestatic hepatitis from prolonged kratom use: a case report. Hepatology. 2015;61(3):1086–7.
Riverso M, Chang M, Soldevila-Pico C, Lai J, Liu X. Histologic characterization of kratom use-associated liver Injury. Gastroenterol Res. 2018;11(1):79–82.
Griffiths CL, Gandhi N, Olin JL. Possible kratom-induced hepatomegaly: a case report. J Am Pharm Assoc. 2018;58(5):561–3.
Mousa MS, Sephien A, Gutierrez J, OʼLeary C. N-Acetylcysteine for acute hepatitis induced by kratom herbal tea. Am J Ther. 2018;25(5): e550–e1.
Antony A, Lee TP. Herb-induced liver injury with cholestasis and renal injury secondary to short-term use of kratom (Mitragyna speciosa). Am J Ther. 2019;26(4):e546–e547.
Osborne CS, Overstreet AN, Rockey DC, Schreiner AD. Drug-induced liver injury caused by kratom use as an alternative pain treatment amid an ongoing opioid epidemic. J Investig Med High Impact Case Rep. 2019;7:1–5.
Fernandes CT, Iqbal U, Tighe SP, Ahmed A. Kratom-induced cholestatic liver injury and its conservative management. J Investig Med High Impact Case Rep. 2019;7:2324709619836138.
Aldyab M, Ells PF, Buib R, Chapmanc TD, Lee H. Kratom-induced cholestatic liver injury mimicking anti-mitochondrial antibody-negative primary biliary cholangitis: a case report and review of literature. Gastroenterol Res. 2019;12(4):211–5.
Tayabali K, Bolzon C, Foster P, Patel J, Kalim MO. Kratom: a dangerous player in the opioid crisis. J Commun Hosp Internal Med Perspect. 2018;8(3):107–10.
Drago JZ, Lane B, Kochav J, Chabner B. The harm in kratom. Oncologist. 2017;22(8):1010–1.
Kupferschmidt H. Toxic hepatitis after Kratom (Mitragyna sp.) consumption. Clin Toxicol. 2011;49(6):532.
Kesar V, Michel A, Weisberg I. Mitragyna Speciosa (Kratom)-induced cholestatic hepatitis in abstracts Submitted for the 78th Annual Scientific Meeting of the American College of Gastroenterology. Am J Gastroenterol. 2013;108:S106–S161161.
Bernier M, Allaire M, Lelong-Boulouard V, Rouillon C, Boisselier R. Inserm. Kratom (Mitragyna speciosa) “phyto-toxicomania": about a case of acute hepatitis. Fundam Clin Pharmacol. 2017;31:19–211.
Shah SR, Basit SA, Orlando FL. Kratom-induced severe intrahepatic cholestasis: a case report. Am J Gastroenterol. 2017;112:S1190.
Ricardo J, Conte J, Alkayali T, Salem AI, Gastroenterology S. Mo1466-Kratom induced cholestatic hepatitis. Gastroenterology. 2019;156(6):S1316.
Bøgevig S, Breindal T, Christensen MB, Nielsen T, Hoegberg LCG. Severe liver injury caused by recommended doses of the food supplement kratom. Clin Toxicol. 2019;57(6):527.
Rivera R, Sharma R, Shah A. Liver toxicity following abuse of kratom (Mitragyna speciosa): 753. Am J Gastroenterol. 2011;106:S284.
Pronesti V, Sial M, Talwar A, Aoun E. Cholestatic liver injury caused by kratom ingestion: 2426. Am J Gastroenterol. 2019;114:S1344.
Kaur R, Siedlecki C, Jafri SM. A case of kratom induced cholestasis. J Gen Intern Med. 2019;34(2):S425–S426426.
Desai P, Ramachandra K, Shah M. Kratom induced hepatotoxicity and the role of N-acetyl cysteine. Abstract from conference: Southern Regional Meeting 2019. J Investig Med High Impact Case Rep. 2019;67(2):606.
Arens A, Gerona R, Meier K, Smollin C. Acute cholecystitis associated with Kratom abuse. Clin Toxicol. 2015;53(7):661.
Mackenzie C, Thompson M. Salmonella contaminated Kratom ingestion associated with fulminant hepatic failure requiring liver transplantation. Clin Toxicol. 2018;56(19):947.
De Francesco E, Lougheed C, Mackenzie C. Kratom-induced acute liver failure. Can J Hosp Pharm. 2019;72(1):69.
Sullivan SN. Acute cholestatic hepatitis due to kratom. Unpublished manuscript. 10.13140/RG.2.1.3651.7366. 2016.
LiverTox, NIH. Summary of case 6972. https://livertox.niddk.nih.gov/Home/ReferenceCases/kratom/6972. Accessed 25 Apr 2019.
LiverTox, NIH. Summary of case 8332. https://livertox.niddk.nih.gov/Home/ReferenceCases/kratom/8332. Accessed 25 Apr 2019.
Aithal GP, Watkins PB, Andrade RJ, Larrey D, Molokhia M, Takikawa H, et al. Case definition and phenotype standardization in drug-induced liver injury. Clin Pharmacol Ther. 2011;89(6):806–15.
Navarro VJ, Odin J, Ahmad J, Hayashi PH, Fontana RJ, Conjeevaram HS, et al. Increasing episodes of hepatotoxicity in the drug induced liver injury network associated with kratom, a botanical product with opioid-like activity. Hepatology. 2019;70(1):138A.
CFSAN Adverse Event Reporting System (CAERS). Data files, January 2004–June 2018. https://www.fda.gov/food/complianceenforcement/ucm494015.htm. Accessed 25 Apr 2019.
FDA Adverse Event Reporting System (FAERS). Public dashboard. https://www.fda.gov/drugs/guidancecomplianceregulatoryinformation/surveillance/adversedrugeffects/ucm070093.htm. Accessed 25 Apr 2019.
Erowid Experience Vaults: Kratom Reports (also Mitragyna speciosa). https://www.erowid.org/experiences/subs/exp_Kratom.shtml. Accessed 1 Apr 2019.
Bluelight Forum. https://www.bluelight.org/xf/forums. Accessed 1 Apr 2019.
Macko E, Weisbach JA, Douglas B. Some observations on the pharmacology of mitragynine. Arch Int Pharmacodyn Ther. 1972;198(1):145–61.
Harizal SN, Mansor SM, Hasnan J, Tharakan JKJ, Abdullah J. Acute toxicity study of the standardized methanolic extract of Mitragyna speciosa Korth in rodent. J Ethnopharmacol. 2010;131(2):404–9.
Kamal MS, Ghazali AR, Yahya NA. Acute toxicity study of standardized Mitragyna speciosa korth aqueous extract in Sprague dawley rats. J Plant Stud. 2012;1:2.
Sabetghadam A, Ramanathan S, Sasidharan S, Mansor SM. Subchronic exposure to mitragynine, the principal alkaloid of Mitragyna speciosa, in rats. J Ethnopharmacol. 2013;146(3):815–23.
Fakurazi S, Rahman SA, Hidayat MT, Ithnin H, Moklas MAM, Arulselvan P. The combination of mitragynine and morphine prevents the development of morphine tolerance in mice. Molecules. 2013;18(1):666–81.
Sakaran R, Othman F, Jantan I, Thent ZC, Das S. Effect of subacute dose of Mitragyna speciosa Korth crude extract in female sprague dawley rats. J Med Bioeng. 2014;3:2.
Ali SRE, Moklas MAM, Taib CNM. DREAM and C-fos proteins expression after treatment with malaysian Mitragyna speciosa. Res J Pharm Biol Chem Sci. 2014;5(5):32.
Ilmie MU, Jaafar H, Mansor SM, Abdullah JM. Subchronic toxicity study of standardized methanolic extract of Mitragyna speciosa Korth in Sprague-Dawley Rats. Front Neurosci. 2015;9:189.
Haslan H, Suhaimi FH, Das S. Mitragyna speciosa-induced hepatotoxicity-treated effectively by piper betle: scope as a future antidote. Asian J Pharm Clin Res. 2018;11(3):43–6.
Guenther E, Musick M, Davis T. Faseb. Reversal of hepatomegaly following cessation of Kratom Consumption in C57BL/6 male and female mice. FASEB J. 2019;33(Suppl 1):765–8.
Manda VK, Avula B, Dale OR, Ali Z, Khan IA, Walker LA, et al. PXR mediated induction of CYP3A4, CYP1A2, and P-gp by Mitragyna speciosa and its alkaloids. Phytother Res. 2017;31(12):1935–45.
Wang YM, Chai SC, Brewer CT, Chen T. Pregnane X receptor and drug-induced liver injury. Expert Opin Drug Metab Toxicol. 2014;10(11):1521–32.
Lammert C, Bjornsson E, Niklasson A, Chalasani N. Oral medications with significant hepatic metabolism at higher risk for hepatic adverse events. Hepatology. 2010;51(2):615–20.
Trakulsrichai S, Sathirakul K, Auparakkitanon S, Krongvorakul J, Sueajai J, Noumjad N, et al. Pharmacokinetics of mitragynine in man. Drug Des Dev Ther. 2015;9:2421–9.
Ya K, Tangamornsuksan W, Scholfield CN, Methaneethorn J, Lohitnavy M. Pharmacokinetics of mitragynine, a major analgesic alkaloid in kratom (Mitragyna speciosa): a systematic review. Asian J Psychiatry. 2019;43:73–82.
Saidin NA, Randall T, Takayama H. Malaysian Kratom, a phyto-pharmaceutical of abuse: studies on the mechanism of its cytotoxicity. Toxicology. 2008;1(253):19–20.
Oliveira AS, Fraga S, Carvalho F. Chemical characterization and in vitro cyto-and genotoxicity of ‘legal high’ products containing Kratom (Mitragyna speciosa). Forensic Toxicol. 2016;34(2):213–26.
Philipp AA, Wissenbach DK, Zoerntlein SW, Klein ON, Kanogsunthornrat J, Maurer HH. Studies on the metabolism of mitragynine, the main alkaloid of the herbal drug Kratom, in rat and human urine using liquid chromatography-linear ion trap mass spectrometry. J Mass Spectrom. 2009;44(8):1249–61.
Azizi J, Ismail S, Mansor SM. Mitragyna speciosa Korth leaves extracts induced the CYP450 catalyzed aminopyrine-N-demethylase (APND) and UDP-glucuronosyl transferase (UGT) activities in male Sprague-Dawley rat livers. Drug Metab Drug Interact. 2013;28(2):95–105.
Haron M, Ismail S. Effects of mitragynine and 7-hydroxymitragynine (the alkaloids of Mitragyna speciosa Korth) on 4-methylumbelliferone glucuronidation in rat and human liver microsomes and recombinant human uridine 5’-diphospho-glucuronosyltransferase isoforms. Pharmacogn Res. 2015;7:4.
Azizi J, Ismail S, Mordi MN, Ramanathan S, Said MIM, Mansor SM. In vitro and in vivo effects of three different Mitragyna speciosa korth leaf extracts on phase II drug metabolizing enzymes—glutathione transferases (GSTs). Molecules. 2010;15(1):432–41.
Rusli N, Amanah A, Kaur G, Adenan MI, Sulaiman SF, Wahab HA, et al. The inhibitory effects of mitragynine on P-glycoprotein in vitro. Naunyn Schmiedeberg's Arch Pharmacol. 2019;392(4):481–96.
Kotsampasakou E, Ecker GF. Predicting drug-induced cholestasis with the help of hepatic transporters-an in silico modeling approach. J Chem Inf Model. 2017;57(3):608–15.
Gijbels E, Vinken M. Mechanisms of drug-induced cholestasis. In: M Vinken (ed) Experimental cholestasis research. methods in molecular biology. New York: Humana Press; 2019.
Zafarullah M, Li WQ, Sylvester J, Ahmad M. Molecular mechanisms of N-acetylcysteine actions. Cell Mol Life Sci. 2003;60(1):6–20.
Paumgartner G, Beuers U. Ursodeoxycholic acid in cholestatic liver disease: mechanisms of action and therapeutic use revisited. Hepatology. 2002;36(3):525–31.
Dalton HR, Fellows HJ, Stableforth W, Joseph M, Thurairajah PH, Warshow U, et al. The role of hepatitis E virus testing in drug-induced liver injury. Aliment Pharmacol Ther. 2007;26(10):1429–35.
Davern TJ, Chalasani N, Fontana RJ, Hayashi PH, Protiva P, Kleiner DE, et al. Acute hepatitis E infection accounts for some cases of suspected drug-induced liver injury. Gastroenterology. 2011;141(5):1665–72.e1.
Acknowledgments
The authors would like to thank Laurie Halmo, MD, for contributions to the manuscript.
Funding
This report did not receive any specific funding.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Jonathan Schimmel and Richard C. Dart declare no conflicts of interest.
Rights and permissions
About this article
Cite this article
Schimmel, J., Dart, R.C. Kratom (Mitragyna Speciosa) Liver Injury: A Comprehensive Review. Drugs 80, 263–283 (2020). https://doi.org/10.1007/s40265-019-01242-6
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40265-019-01242-6