Abstract
Introduction and Objective
Given the high prevalence of antibiotic prescription during pregnancy in France and previous studies suggesting an increased risk of infection in offspring with such exposures, our study aimed to investigate the association between prenatal exposure to systemic antibiotics and serious infections in full-term infants during their first year of life.
Methods
We conducted a retrospective population-based cohort study on singleton, full-term liveborn non-immunocompromised infants, using the French National Health Data System (SNDS) between 2012 and 2021. Systemic antibiotic dispensing in ambulatory care settings during pregnancy defined the exposure. Outcomes concerned serious infections (i.e., infections requiring hospitalization) in offspring identified between 3 and 12 months of life, hence excluding infections of maternal origin. Adjusted odds ratios (aORs) were estimated using logistic regression with multivariate models to control for potential confounders.
Results
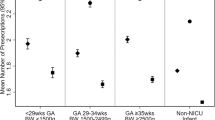
Of 2,836,630 infants included, 39.6% were prenatally exposed to systemic antibiotics. Infants prenatally exposed to antibiotics had a higher incidence of serious infections compared with unexposed infants {aOR 1.12 [95% confidence interval (95% CI) 1.11–1.13]}. Similar associations were observed according to the timing of exposure during pregnancy, antibiotic class, and site of infections. The strongest association was observed when infants were prenatally exposed to three or more antibiotic courses during pregnancy [aOR 1.21 (95% CI 1.19–1.24)]. Limitations include residual confounders, such as genetic susceptibility to infections and the role of the underlying pathogen agent.
Conclusion
Prenatal exposure to systemic antibiotics is very common and is associated with a weak yet significant associations with subsequent serious infectious events during the first year of life. While our study revealed associations, it is important to note that causation cannot be established, given the acknowledged limitations, including potential confounding by indication.



Similar content being viewed by others
References
Sinha A, Yokoe D, Platt R. Epidemiology of neonatal infections: experience during and after hospitalization. Pediatr Infect Dis J. 2003;22(3):244–50. https://doi.org/10.1097/01.inf.0000055060.32226.8a.
Ferreras-Antolín L, Oligbu G, Okike IO, Ladhani S. Infection is associated with one in five childhood deaths in England and Wales: analysis of national death registrations data, 2013–15. Arch Dis Child. 2020;105(9):857–63. https://doi.org/10.1136/archdischild-2019-318001.
Troeger C, Blacker B, Khalil IA, Rao PC, Cao J, Zimsen SRM, et al. Estimates of the global, regional, and national morbidity, mortality, and aetiologies of lower respiratory infections in 195 countries, 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet Infect Dis. 2018;18(11):1191–210. https://doi.org/10.1016/S1473-3099(18)30310-4.
Tregoning JS, Schwarze J. Respiratory viral infections in infants: causes, clinical symptoms, virology, and immunology. Clin Microbiol Rev. 2010;23(1):74–98. https://doi.org/10.1128/CMR.00032-09.
Behrooz L, Balekian DS, Faridi MK, Espinola JA, Townley LP, Camargo CA. Prenatal and postnatal tobacco smoke exposure and risk of severe bronchiolitis during infancy. Respir Med. 2018;140:21–6. https://doi.org/10.1016/j.rmed.2018.05.013.
Bush NR, Savitz J, Coccia M, Jones-Mason K, Adler N, Boyce WT, et al. Maternal stress during pregnancy predicts infant infectious and noninfectious illness. J Pediatr. 2021;228:117-125.e2. https://doi.org/10.1016/j.jpeds.2020.08.041.
Gauthier TW, Drews-Botsch C, Falek A, Coles C, Brown LAS. Maternal alcohol abuse and neonatal infection. Clin Exp Res. 2005;29(6):1035–43. https://doi.org/10.1097/01.alc.0000167956.28160.5e.
Goshen S, Novack L, Erez O, Yitshak-Sade M, Kloog I, Shtein A, et al. The effect of exposure to particulate matter during pregnancy on lower respiratory tract infection hospitalizations during first year of life. Environ Health. 2020;19(1):90. https://doi.org/10.1186/s12940-020-00645-3.
Miller JE, Goldacre R, Moore HC, Zeltzer J, Knight M, Morris C, et al. Mode of birth and risk of infection-related hospitalisation in childhood: a population cohort study of 7.17 million births from 4 high-income countries. PLoS Med. 2020;17(11): e1003429. https://doi.org/10.1371/journal.pmed.1003429.
Tsao NW, Sayre EC, Hanley G, Sadatsafavi M, Lynd LD, Marra CA, et al. Risk of preterm delivery and small-for-gestational-age births in women with autoimmune disease using biologics before or during pregnancy: a population-based cohort study. Ann Rheum Dis. 2018;77(6):869–74. https://doi.org/10.1136/annrheumdis-2018-213023.
Williams EJ, Embleton ND, Bythell M, Ward Platt MP, Berrington JE. The changing profile of infant mortality from bacterial, viral and fungal infection over two decades. Acta Paediatr. 2013;102(10):999–1004. https://doi.org/10.1111/apa.12341.
Nakitanda AO, Kieler H, Odsbu I, Rhedin S, Almqvist C, Pasternak B, et al. In-utero antibiotic exposure and subsequent infections in infancy: a register-based cohort study with sibling analysis. Am J Obstet. 2023;5(4): 100860. https://doi.org/10.1016/j.ajogmf.2023.100860.
Miller JE, Wu C, Pedersen LH, de Klerk N, Olsen J, Burgner DP. Maternal antibiotic exposure during pregnancy and hospitalization with infection in offspring: a population-based cohort study. Int J Epidemiol. 2018;47(2):561–71. https://doi.org/10.1093/ije/dyx272.
Zhou P, Zhou Y, Liu B, Jin Z, Zhuang X, Dai W, et al. Perinatal antibiotic exposure affects the transmission between maternal and neonatal microbiota and is associated with early-onset sepsis. mSphere. 2020;5(1):e00984-e1019. https://doi.org/10.1128/mSphere.00984-19.
Jess T, Morgen CS, Harpsøe MC, Sørensen TIA, Ajslev TA, Antvorskov JC, et al. Antibiotic use during pregnancy and childhood overweight: a population-based nationwide cohort study. Sci Rep. 2019;9(1):11528. https://doi.org/10.1038/s41598-019-48065-9.
Korpela K, Dikareva E, Hanski E, Kolho KL, de Vos WM, Salonen A. Cohort profile: Finnish health and early life microbiota (HELMi) longitudinal birth cohort. BMJ Open. 2019;9(6): e028500. https://doi.org/10.1136/bmjopen-2018-028500.
Stearns JC, Simioni J, Gunn E, McDonald H, Holloway AC, Thabane L, et al. Intrapartum antibiotics for GBS prophylaxis alter colonization patterns in the early infant gut microbiome of low risk infants. Sci Rep. 2017;7(1):16527. https://doi.org/10.1038/s41598-017-16606-9.
Gonzalez-Perez G, Hicks AL, Tekieli TM, Radens CM, Williams BL, Lamousé-Smith ESN. Maternal antibiotic treatment impacts development of the neonatal intestinal microbiome and antiviral immunity. J Immunol. 2016;196(9):3768–79. https://doi.org/10.4049/jimmunol.1502322.
Collado MC, Rautava S, Aakko J, Isolauri E, Salminen S. Human gut colonisation may be initiated in utero by distinct microbial communities in the placenta and amniotic fluid. Sci Rep. 2016;6(1):23129. https://doi.org/10.1038/srep23129.
Rutayisire E, Huang K, Liu Y, Tao F. The mode of delivery affects the diversity and colonization pattern of the gut microbiota during the first year of infants’ life: a systematic review. BMC Gastroenterol. 2016;16(1):86. https://doi.org/10.1186/s12876-016-0498-0.
Kim H, Choe YJ, Cho H, Heo JS. Effect of prenatal antibiotic exposure on neonatal outcomes of preterm infants. Pediatr Infect Vaccine. 2021;28(3):149. https://doi.org/10.14776/piv.2021.28.e21.
Cunha AJLA, Santos AC, Medronho RA, Barros H. Use of antibiotics during pregnancy is associated with infection in children at four years of age in Portugal. Acta Paediatr. 2021;110(6):1911–5. https://doi.org/10.1111/apa.15733.
Demailly R, Escolano S, Quantin C, Tubert-Bitter P, Ahmed I. Prescription drug use during pregnancy in France: a study from the national health insurance permanent sample. Pharmacoepidemiol Drug Saf. 2017;26(9):1126–34. https://doi.org/10.1002/pds.4265.
Bérard A, Abbas-Chorfa F, Kassai B, Vial T, Nguyen KA, Sheehy O, et al. The French Pregnancy Cohort: medication use during pregnancy in the French population. PLoS One. 2019;14(7): e0219095. https://doi.org/10.1371/journal.pone.0219095.
Tubiana S, Sibiude J, Herlemont P, et al. Trends in anti-infective use during pregnancy in France between 2010 and 2019: a nationwide population-based study. Br J Clin Pharmacol. 2023;89(5):1629–39. https://doi.org/10.1111/bcp.15638.
Glasgow TS, Young PC, Wallin J, Kwok C, Stoddard G, Firth S, et al. Association of intrapartum antibiotic exposure and late-onset serious bacterial infections in infants. Pediatrics. 2005;116(3):696–702. https://doi.org/10.1542/peds.2004-2421.
Wright AJ, Unger S, Coleman BL, Lam PP, McGeer AJ. Maternal antibiotic exposure and risk of antibiotic resistance in neonatal early-onset sepsis: a case–cohort study. Pediatr Infect Dis J. 2012;31(11):1206–8. https://doi.org/10.1097/INF.0b013e31826eb4f9.
Pedersen TM, Stokholm J, Thorsen J, Mora-Jensen ARC, Bisgaard H. Antibiotics in pregnancy increase children’s risk of otitis media and ventilation tubes. J Pediatr. 2017;183:153-158.e1. https://doi.org/10.1016/j.jpeds.2016.12.046.
Cohen R, Gutvirtz G, Wainstock T, Sheiner E. Maternal urinary tract infection during pregnancy and long-term infectious morbidity of the offspring. Early Hum Dev. 2019;136:54–9. https://doi.org/10.1016/j.earlhumdev.2019.07.002.
Kim JH, Lee J, Kim DH, Park JY, Lee H, Kang HG, et al. Maternal antibiotic exposure during pregnancy is a risk factor for community-acquired urinary tract infection caused by extended-spectrum beta-lactamase-producing bacteria in infants. Pediatr Nephrol. 2022;37(1):163–70. https://doi.org/10.1007/s00467-021-05163-z.
Bezin J, Duong M, Lassalle R, Droz C, Pariente A, Blin P, et al. The national healthcare system claims databases in France, SNIIRAM and EGB: owerful tools for pharmacoepidemiology. Pharmacoepidemiol Drug Saf. 2017;26(8):954–62. https://doi.org/10.1002/pds.4233.
Blotière PO, Weill A, Dalichampt M, Billionnet C, Mezzarobba M, Raguideau F, et al. Development of an algorithm to identify pregnancy episodes and related outcomes in health care claims databases: n application to antiepileptic drug use in 4.9 million pregnant women in France. Pharmacoepidemiol Drug Saf. 2018;27(7):763–70. https://doi.org/10.1002/pds.4556.
Collins A, Weitkamp JH, Wynn JL. Why are preterm newborns at increased risk of infection? Arch Dis Child Fetal Neonatal Ed. 2018;103(4):F391–4. https://doi.org/10.1136/archdischild-2017-313595.
Ukah UV, Aibibula W, Platt RW, Dayan N, Reynier P, Filion KB. Time-related biases in perinatal pharmacoepidemiology: systematic review of observational studies. Pharmacoepidemiol Drug Saf. 2022;31(12):1228–41. https://doi.org/10.1002/pds.5504.
Sahli L, Lapeyre-Mestre M, Derumeaux H, Moulis G. Positive predictive values of selected hospital discharge diagnoses to identify infections responsible for hospitalization in the French national hospital database. Pharmacoepidemiol Drug Saf. 2016;25(7):785–9. https://doi.org/10.1002/pds.4006.
Meyer A, Taine M, Drouin J, Weill A, Carbonnel F, Dray-Spira R. Serious infections in children born to mothers with inflammatory bowel disease with in utero exposure to thiopurines and anti-tumor necrosis factor. Clin Gastroenterol Hepatol. 2022;20(6):1269-1281.e9. https://doi.org/10.1016/j.cgh.2021.07.028.
Prevention of group B streptococcal early-onset disease in newborns: ACOG Committee Opinion, number 797. Obstet Gynecol. 2020;135(2):e51–72. https://doi.org/10.1097/AOG.0000000000003668 (Erratum in: Obstet Gynecol. 2020;135(4):978–979. PMID: 31977795).
National Collaborating Centre for Women's and Children's Health (UK). Antibiotics for Early-Onset Neonatal Infection: Antibiotics for the Prevention and Treatment of Early-Onset Neonatal Infection. London: RCOG Press; 2012. (PMID: 23346609).
Palosse-Cantaloube L, Hurault-Delarue C, Beau AB, Montastruc JL, Lacroix I, Damase-Michel C. Risk of infections during the first year of life after in utero exposure to drugs acting on immunity: population-based cohort study. Pharmacol Res. 2016;113:557–62. https://doi.org/10.1016/j.phrs.2016.09.028.
Ghosn W. Indicateurs écologiques synthétiques du niveau socio-économique pour la recherche en Santé. 2018. https://www.cepidc.inserm.fr/sites/default/files/2020-11/Note_indices_socioeco-2.pdf. Accessed 25 June 2023.
Albrecht M, Arck PC. Vertically transferred immunity in neonates: mothers, mechanisms and mediators. Front Immunol. 2020;11:555. https://doi.org/10.3389/fimmu.2020.00555.
Levy O. Innate immunity of the newborn: basic mechanisms and clinical correlates. Nat Rev Immunol. 2007;7(5):379–90. https://doi.org/10.1038/nri2075.
Ygberg S, Nilsson A. The developing immune system—from foetus to toddler: eveloping immune systemfrom foetus to toddler. Acta Paediatr. 2012;101(2):120–7. https://doi.org/10.1111/j.1651-2227.2011.02494.x.
Nyangahu DD, Jaspan HB. Influence of maternal microbiota during pregnancy on infant immunity. Clin Exp Immunol. 2019;198(1):47–56. https://doi.org/10.1111/cei.13331.
Romano-Keeler J, Weitkamp JH. Maternal influences on fetal microbial colonization and immune development. Pediatr Res. 2015;77(1–2):189–95. https://doi.org/10.1038/pr.2014.163.
Mueller NT, Bakacs E, Combellick J, Grigoryan Z, Dominguez-Bello MG. The infant microbiome development: mom matters. Trends Mol Med. 2015;21(2):109–17. https://doi.org/10.1016/j.molmed.2014.12.002.
Mishra A, Lai GC, Yao LJ, Aung TT, Shental N, Rotter-Maskowitz A, et al. Microbial exposure during early human development primes fetal immune cells. Cell. 2021;184(13):3394-3409.e20. https://doi.org/10.1016/j.cell.2021.04.039.
Rackaityte E, Halkias J. Microbial exposure during early human development primes fetal immune cells. Front Immunol. 2020;11:588. https://doi.org/10.3389/fimmu.2020.00588.
Goenka A, Kollmann T. Development of immunity in early life. J Infect. 2015;71(Suppl1):S112–20. https://doi.org/10.1016/j.jinf.2015.04.027.
Loewen K, Monchka B, Mahmud SM, ’t Jong G, Azad MB. Prenatal antibiotic exposure and childhood asthma: a population-based study. Eur Respir J. 2018;52(1):1702070. https://doi.org/10.1183/13993003.02070-2017.
Wu P, Feldman AS, Rosas-Salazar C, James K, Escobar G, Gebretsadik T, et al. Relative importance and additive effects of maternal and infant risk factors on childhood asthma. PLoS One. 2016;11(3): e0151705. https://doi.org/10.1371/journal.pone.0151705.
Stokholm J, Sevelsted A, Bønnelykke K, Bisgaard H. Maternal propensity for infections and risk of childhood asthma: a registry-based cohort study. Lancet Respir Med. 2014;2(8):631–7. https://doi.org/10.1016/S2213-2600(14)70152-3.
Ng SC, Peng Y, Zhang L, Mok CK, Zhao S, Li A, et al. Gut microbiota composition is associated with SARS-CoV-2 vaccine immunogenicity and adverse events. Gut. 2022;71(6):1106–16. https://doi.org/10.1136/gutjnl-2021-326563.
Lacroix I, Damase-Michel C, Lapeyre-Mestre M, Montastruc J. Prescription of drugs during pregnancy in France. Lancet. 2000;356(9243):1735–6. https://doi.org/10.1016/s0140-6736(00)03209-8.
de Jonge L, de Walle HEK, de Jong-van den Berg LTW, van Langen IM, Bakker MK. Actual use of medications prescribed during pregnancy: a cross-sectional study using data from a population-based congenital anomaly registry. Drug Saf. 2015;38(8):737–47. https://doi.org/10.1007/s40264-015-0302-z.
Størdal K, Lundeby KM, Brantsæter AL, Haugen M, Nakstad B, Lund-Blix NA, et al. Breast‐feeding and Infant Hospitalization for Infections: large cohort and sibling analysis. J Pediatr Gastroenterol Nutr. 2017;65(2):225–31. https://doi.org/10.1097/MPG.0000000000001539.
Victora CG, Bahl R, Barros AJD, França GVA, Horton S, Krasevec J, et al. Breastfeeding in the 21st century: epidemiology, mechanisms, and lifelong effect. Lancet. 2016;387(10017):475–90. https://doi.org/10.1016/S0140-6736(15)01024-7.
Tsao NW, Lynd LD, Sayre EC, Sadatsafavi M, Hanley G, De Vera MA. Use of biologics during pregnancy and risk of serious infections in the mother and baby: a Canadian population-based cohort study. BMJ Open. 2019;9(2): e023714. https://doi.org/10.1136/bmjopen-2018-023714.
Muenchhoff M, Goulder PJR. Sex differences in pediatric infectious diseases. J Infect Dis. 2014;209(suppl 3):S120–6. https://doi.org/10.1093/infdis/jiu232.
Carroll KN, Gebretsadik T, Minton P, Woodward K, Liu Z, Miller EK, et al. Influence of maternal asthma on the cause and severity of infant acute respiratory tract infections. J Allergy Clin Immunol. 2012;129(5):1236–42. https://doi.org/10.1016/j.jaci.2012.01.045.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
No funding was received for conducting this study.
Conflict of interest
All authors have no example conflicts of interest to disclose.
Availability of data and material
Data sharing is not applicable to this article, as the datasets used are based on pseudoanonymized data that are protected by agreements with the French Data Protection Commission (CNIL; Commission Nationale de l’Informatique et Liberté).
Ethics approval
This study was approved by the French Data Protection Commission (CNIL; Commission Nationale de l’Informatique et Liberté; agreement DE-2015-192) and the French Committee for the Protection of Healthcare Data (CERESS; Comité spécifique de Recherche sur les Données de Santé). In agreements with French regulations, observational studies conducted on anonymous medico-administrative data do not require an ethics committee approval.
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Code availability
Code is available upon reasonable request to the authors.
Author contributions
M. Tisseyre conceptualized and designed the study, collected data, carried out the initial analyses, analyzed the results, drafted the initial manuscript, and critically revised the manuscript. M. Collier designed the data collection instruments, carried out the initial analyses, and critically reviewed the manuscript. N. Beeker designed the data collection instruments and critically reviewed the manuscript. F. Kaguelidou and JM. Treluyer reviewed the study design, analyzed the results, and critically reviewed the manuscript for important intellectual content. L. Chouchana conceptualized and designed the study, analyzed the results, drafted the initial manuscript, and critically reviewed and revised the manuscript. All authors approved the final manuscript as submitted and agree to be accountable for all aspects of the work.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Tisseyre, M., Collier, M., Beeker, N. et al. In Utero Exposure to Antibiotics and Risk of Serious Infections in the First Year of Life. Drug Saf 47, 453–464 (2024). https://doi.org/10.1007/s40264-024-01401-z
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40264-024-01401-z