Abstract
Comorbidity between borderline personality disorder (BPD) and other mental disorders is common. Although no specific pharmacological treatments have been approved for the treatment of BPD, many drugs, including antidepressants such as selective serotonin reuptake inhibitors (SSRIs), mood stabilizers, second-generation antipsychotics, and even benzodiazepines, are routinely prescribed off label. Nonetheless, recommendations for off-label drugs in these patients are highly varied, with a notable lack of agreement among clinical guidelines. The most common reason for pharmacological treatment and polypharmacy in these patients is comorbidity with other psychiatric disorders. In this context, we reviewed major clinical guidelines and the available data on pharmacotherapy in patients with BPD to develop practical recommendations to facilitate decision-making in routine clinical practice, thus helping clinicians to select the optimal therapeutic approach in patients with BPD who have comorbid disorders. This review confirmed that no clear recommendations for the pharmacological treatment are available in clinical guidelines. Therefore, based on the available evidence, we have developed a series of recommendations for pharmacotherapy in patients with BPD who present the four most common comorbidities (affective, anxiety, eating, and drug use disorders). Here, we discuss the recommended treatment approach for each of these comorbid disorders. The prescription of medications should be considered only as an adjunct to BPD-specific psychotherapy. Polypharmacy and the use of unsafe drugs (i.e., with a risk of overdose) should be avoided. Our review highlights the need for more research to provide more definitive guidance and to develop treatment algorithms.
Similar content being viewed by others
Comorbidity with other mental disorders is common in individuals with borderline personality disorder (BPD). Pharmacotherapy is substantially more common than recommended in clinical guidelines. |
Several approaches are proposed to guide the pharmacological management of patients with BPD with the most common comorbidities (affective, anxiety, eating, and drug use disorders). |
The prescription of medications should only be considered as an adjunct to BPD-specific psychotherapy. Polypharmacy and unsafe drugs should be avoided. |
Several different treatment algorithms and therapeutic recommendations are provided for use in routine clinical practice to treat patients with BPD and comorbidities. |
1 Introduction
Borderline personality disorder (BPD) is a serious mental illness with an estimated community prevalence of 2.7% [1,2,3]. In individuals seeking treatment at outpatient mental health clinics, the prevalence is approximately 10%, with rates as high as 20% in psychiatric inpatients [2, 3]. BPD is a heterogeneous disorder that may include emotion dysregulation (intense, rapidly changing emotions), impulsivity (with dysfunctional behaviors such as self-harm, drug abuse, or binge eating), and unstable identity and interpersonal relationships. Not surprisingly, this clinical heterogeneity is often associated with many other mental disorders and somatic conditions [1].
Other mental disorders are common in patients with BPD, as evidenced by the high comorbidity rates reported in numerous cross-sectional and longitudinal studies [2,3,4,5]. The findings of an epidemiological study in the USA suggested that BPD is rarely diagnosed alone, with high lifetime prevalence rates in these patients for anxiety disorders (84.8%), mood disorders (82.7%), substance use disorders (SUD; 78.2%), and eating disorders (ED; 33.7%) [4, 5]. Similarly, several other mental disorders also present high rates of comorbidity with BPD, including posttraumatic stress disorder (PTSD), attention deficit hyperactivity disorder (ADHD), and bipolar disorder [5]. However, it is important to consider that the symptoms of BPD frequently overlap with several disorders that share the same features. For example, while impulsivity with drug abuse or binge eating is a key marker of BPD, it is also a common symptom in other disorders [2].
In patients with BPD, co-occurring psychiatric disorders are often chronic, and may be associated with severely impaired social and occupational functioning that requires social support; moreover, they are often difficult to treat [2, 6]. Since the first randomized control trial (RCT) of psychotherapy for patients with BPD was performed in 1993 [7], more than ten different manualized psychotherapies for BPD have been evaluated [8]. Of those psychological interventions, five—dialectical behavioral therapy (DBT), mentalization-based treatment (MBT), schema focused therapy (SFT), transference-focused psychotherapy (TFP), and systems training for emotional predictability and problem solving (STEPPS)—have been established as evidence-based treatments (EBT) for BPD. To date, the two approaches that have received the most attention, as evidenced by the number of clinical trials performed, are DBT and MBT [8]. To better manage the complex comorbidities associated with BPD, several evidence-based psychotherapeutic approaches have been adapted for use in this challenging patient profile, especially those with comorbid SUDs, EDs, and PTSD [8].
Unfortunately, not all individuals have access to these intensive, highly specialized treatments, which are difficult to implement in most health care facilities due to insufficient resources [8,9,10,11]. In this context, it is not surprising that many clinicians routinely prescribe drugs for the treatment of patients with BPD, despite the weak evidence supporting the value of pharmacotherapy to improve core BPD symptoms, interpersonal impairment, and functional difficulties [12].
No psychotropic drugs have been officially approved for the specific treatment of BPD. Although some studies have been performed, most of these are small, with relatively short treatment periods and a wide range of different measures. In addition, most RCTs excluded patients with comorbidities. In short, the evidence to support pharmacotherapy in this setting is weak [8, 12].
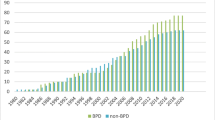
In routine clinical practice, many drugs are commonly prescribed “by default” in patients with BPD, as evidenced by data from the USA and some European countries, where ≥ 80% of patients with BPD are on pharmacotherapy, and 50% are taking three or more drugs [12,13,14,15,16,17,18]. Although some clinical guidelines recommend pharmacotherapy to treat certain BPD symptoms, such as impulsivity, emotional disturbances, or cognitive-perceptual symptoms, recent expert recommendations do not support the use of pharmacotherapy as a first-line treatment or for specific domains [2, 9, 19].
The main factor associated with pharmacological treatment or polypharmacy is comorbidity with other mental health disorders, most notably—and congruently—affective, anxiety, and eating disorders [14, 15, 20]. Nonetheless, pharmacotherapy in BPD patients is widespread, even in patients with no comorbidities. For example, one study involving a sample of 457 individuals with BPD found that close to 80% of comorbidity-free patients with BPD were also receiving pharmacological treatment (62.9% received antidepressants, 59.7% benzodiazepines, 22.6% mood stabilizers, and 27.4% antipsychotics) with 42% on polypharmacy [15].
Antidepressants, particularly selective serotonin reuptake inhibitors (SSRI) such as citalopram and fluoxetine, are the most commonly prescribed drugs for BPD, despite the lack of evidence to support their use [18, 20]. Gunderson et al. [21], found that the prescription of antidepressants in patients with BPD was most commonly associated with comorbidity for affective disorders (odds ratio 2.77). Although the use of benzodiazepines is not recommended due to their highly addictive nature and their potential for behavioral disinhibition, prescription rates nevertheless remain high, particularly in patients with affective and anxious disorders who do not present SUD [15, 18, 20].
The prescription of mood stabilizers, such as topiramate and valproate, in patients with BPD is associated with the presence of anxiety and eating disorders; by contrast, antipsychotics (mostly atypical ones such as quetiapine and olanzapine) are not associated with any axis I comorbidity [18, 20].
The pharmacological treatment of BPD has been evaluated in clinical guidelines and in several reviews [2, 12, 19]. However, no consensus on therapeutic indications has been reached. Importantly, none of those publications have addresses the specific question of the pharmacological treatment of comorbidities in BPD. This is relevant given that comorbidity with other mental disorders is common in patients with BPD, which partially explains why many individuals with BPD receive pharmacotherapy. Moreover, the specific drug that should be prescribed for a given comorbidity is not clear, in large part due to the weak evidence base. In this context, the aim of the present review was to better clarify this question. In addition, we aimed to develop practical recommendations for the pharmacological treatment of patients with the most common comorbidities. Below, we discuss each comorbid disorder separately, taking into account the course of these disorders in individuals with BPD over time.
2 Comorbid Mood Disorders
Mood disorders are one of the most common disorders in individuals with BPD. Up to 80% of patients with BPD present one or more episodes of major depressive disorder (MDD) in their lifetime and 10–30% of patients with MDD have co-occurring BPD [2, 3, 21, 22]. BPD is strongly associated with many mood disorders, especially MDD and dysthymia, with an odds ratio (OR) for any mood disorder of 14.93 [4]. Even in BPD patients without MDD, depressive symptoms and transient “micro-depressions” are common and difficult to clinically differentiate from MDD [23]. Skodol et al. [24] found that having BPD was the most robust predictor of persistent MDD; that study also found that when both of these disorders co-occur, the MDD episodes last longer and the interepisodic interval may be shorter. Improvement in MDD is often predicted by a prior decrease in BPD symptoms; by contrast, the reverse is not necessarily true: improvements in MDD are not always followed by a reduction in BPD symptoms [21]. Longitudinal studies suggest that treatment for BPD may yield positive results in both disorders and that remission of BPD is a predictor of MDD remission [25].
In patients with comorbid BPD and MDD, the available clinical evidence for pharmacological treatment is insufficient to establish any reliable recommendations. Despite these limitations, we have developed a practical treatment algorithm and recommendations, based on our review of the evidence and our clinical experience (Fig. 1). In clinical practice, the first step is to try to differentiate between “micro-depressions” in BPD, which are a common component of BPD psychopathology, and MDD, which is a clinically distinct entity. Table 1 presents several practical hallmarks that may indicate the presence of micro-depressions in BPD. In these patients, depressive symptoms are usually transient and stress related, rarely last for more than a few days, and are usually precipitated by stress and interpersonal factors. However, given the transitory nature of these micro-depressions, the presence of depressive symptoms in a cross-sectional assessment could suggest MDD, but also symptom duration is a key factor to consider [23]. In any case, it is essential to prioritize BPD-appropriate psychotherapy, rather than polypharmacy alone.
Algorithm for the management of patients with borderline personality disorder and comorbid major depressive disorder. AD, antidepressants; APS, antipsychotics; BPD, borderline personality disorder; DBT, dialectical behavioral therapy; EBT, evidence-based treatment; MBT, mentalization-based treatment; MDD, major depressive disorder; SFT, schema-focused therapy; SSRI, selective serotonin reuptake inhibitor; STEPPS, systems training for emotional predictability and problem solving; TCA, tricyclic antidepressants; TFP, transference-focused psychotherapy
As Fig. 1 and Table 2 show, the recommended first-line treatment for a patient with BPD with a mild–moderate MDD episode is BPD-specific psychotherapy. Some clinical guidelines on the treatment of MDD episodes (regardless of the presence or not of BPD) also recommend psychotherapeutic interventions for mild-to-moderate depression as a first-line treatment; however, the routine use of antidepressants should be avoided due to the poor risk–benefit ratio [26]. If the MDD episode is severe or fails to respond to psychotherapy, pharmacotherapy can be considered. The mood disorder should be first treated with antidepressants following the recommendations of clinical guidelines for MDD [26,27,28].
A wide range of antidepressants, including SSRIs, selective norepinephrine reuptake inhibitors (NRIs), selective serotonin and norepinephrine reuptake inhibitors (SNRIs), and others, are available to treat depressive episodes [26]. SSRIs such as fluoxetine, sertraline, citalopram, or escitalopram seem to be the first and most common option prescribed by clinicians for BPD [18, 20]. Antidepressants with an unsafe profile, such as tricyclic antidepressants (TCAs) or monoamine oxidase inhibitors (MAOIs), are not recommended due to the risk of overdose, lower tolerability profiles, and potential adverse reactions [2, 8].
Although mood stabilizers (e.g., lithium, valproate) are commonly prescribed in combination with antipsychotics in patients with MDD as adjunctive strategies [26, 28], there is a notable lack of studies investigating the effectiveness of this approach in patients with comorbid BPD and MDD. Nevertheless, valproate in combination with antidepressants could be efficacious for treatment-resistant MDD and has also shown some beneficial effects in patients with BPD [12, 27]. Lamotrigine was also found to have beneficial effects in treatment-resistant MDD [26,27,28,29,30]. Two small preliminary studies have suggested that this drug may have an effect on impulsivity, anger, and behavioral dyscontrol in BPD [12]. However, the large (n = 276) randomized clinical trial carried out by Crawford et al. [31] in patients with BPD found no evidence to support the use of lamotrigine (400 mg/day) for the treatment of BPD symptoms. Similarly, the findings of a recent Cochrane systematic review did not support the use of lamotrigine for people with personality disorders [12].
Finally, several meta-analyses have found that atypical antipsychotics such as aripiprazole, quetiapine, olanzapine, and risperidone may be efficacious as an adjunctive treatment for individuals with MDD [26]. Some studies also suggest that these atypical antipsychotics may be useful in the treatment of patients with BPD [12]. Therefore, these second-generation antipsychotics could also be useful as adjunctive strategies for individuals with BPD and severe or resistant MDD.
Clearly, pharmacological treatment in patients with comorbid BPD and MDD is important. However, we must also keep in mind that in BPD, drug therapy should only be considered an adjunct to psychological therapy [2]. In addition, the effects of prescription drugs need to be monitored closely; if they are not effective and/or induce excessive side effects, their use should be discontinued. If the response to pharmacological treatment is poor, the ineffective treatment should be discontinued. Additionally, every effort should be made to avoid combining several different antidepressants. Finally, polypharmacy should be avoided whenever possible, as should the use of unsafe drugs that have a risk of overdose (e.g., tricyclic antidepressants) [2].
Although antidepressant treatment can be helpful in patients with comorbid BPD and MDD, it also carries some risks, most notably those associated with polypharmacy (more than half of patients with BPD take three or more psychotropic medications) [18]. Although the main reason for pharmacological treatment or polypharmacy in BPD is comorbidity with psychiatric disorders, it is important to underscore the fact that most patients are medicated, even those with no comorbidities [15, 18]. A second risk is related to patient preferences for pharmacotherapy rather than psychotherapy. Several meta-analyses have shown that the optimal first-line treatment for this condition is BPD-specific psychological therapy, and these findings are reflected in the recommendations of most clinical guidelines [2, 8, 9]. Unfortunately, specialized psychotherapy for BPD is often not available, which explains why pharmacotherapy is sometimes used—inappropriately—as an alternative [9].
In short, in patients with BPD and comorbid MDD, antidepressant treatment should only be offered as an adjunct to psychological therapy. Interestingly, both BPD and MDD may respond to BPD-specific psychotherapy, which underscores the importance of prioritizing this treatment approach over polypharmacy [2, 23, 32].
3 Comorbid Anxiety Disorders
Lifetime comorbidity between BPD and anxiety disorders is high (84.8%) and patients with BPD are 14 times more likely to present an anxiety disorder [especially panic disorder with agoraphobia, generalized anxiety disorder (GAD), and PTSD] [4, 5]. Some studies suggest that anxiety disorders are relatively unstable over time in patients with BPD, with a tendency to decrease significantly after 10 years (although recurrence rates are high) [5].
Anxiety disorders can be treated with psychotherapy, pharmacotherapy, or a combination of both [33]. The treatment plan should be chosen only after careful consideration of individual factors such as patient preferences, previous treatment attempts, and illness severity [33]. In patients with comorbid BPD and anxiety, the best approach may be to start psychotherapy, which all the main evidence-based treatment guidelines agree should be the first-line treatment for BPD [2, 10]. The psychological intervention with the highest level of evidence for the treatment of anxiety disorders is CBT [33]. Nonetheless, MBT or DBT, with specific modules such as emotional regulation, mindfulness, and distress tolerance, could be also a useful psychological intervention for the treatment of anxiety symptoms in BPD [11, 34].
When psychotherapy is unavailable or not as effective as expected, or if the patient expresses a preference for pharmacotherapy, drug therapy should be considered. However, the patient must be fully informed about both the risks and benefits of the available pharmacological alternatives. SSRIs and SNRIs are recommended as first-line drug therapy for anxiety disorders, mainly because drugs these are associated with fewer adverse effects than other therapeutic options such as TCAs or MAOIs [35, 36]. Due to their efficacy and lack of major side effects, the SSRIs (escitalopram, citalopram, fluoxetine, sertraline, fluvoxamine, and paroxetine) and one SNRI (venlafaxine) have received the highest grade of recommendation [36].
For patients with comorbid BPD and anxiety disorder, treatment with SSRIs or SNRIs should only be recommended when combined with BPD-specific psychotherapy. If the patient fails to respond to standard treatments, several alternative strategies (e.g., atypical antipsychotics or anticonvulsants) can be considered, but never as first-line treatment and always keeping in mind the need to avoid polypharmacy and its attendant risks [9, 11, 35]. Despite the common use of low-dose atypical antipsychotics (e.g., quetiapine or olanzapine) and anticonvulsants (e.g., pregabaline or gabapentine) as adjunctive treatments, these are not recommended in current guidelines as a first-line strategy (except for pregabalin for GAD) [36].
All clinical guidelines advise against the use of benzodiazepines due to their addictive potential as well as their capacity to increase suicidal tendencies and disinhibition (2). In real-world clinical practice, however, benzodiazepines are commonly prescribed for the treatment of BPD [11, 15, 33]. The prescription of benzodiazepines in this patient population is likely attributable to several different factors, including comorbidity with anxiety disorders, patient demand for sedatives, the tendency of many psychiatrists to treat specific symptoms in these patients, and the clinical management of exacerbations in emergency departments, where benzodiazepines are prescribed to rapidly alleviate anger [15, 35].
4 Comorbid Eating Disorders
Eating disorders also present high rates of comorbidity with BPD. In a meta-analysis that examined the prevalence of personality disorders among individuals with EDs, BPD was present in 28% of patients with bulimia nervosa (BN), 25% of those with anorexia nervosa (AN) binge-eating/purging subtype (AN–BP), and 10.8% of patients with AN restrictive subtype (AN–R) [36]. Similarly, the prevalence of EDs (of any type) among individuals with BPD is elevated, ranging from 14% to 53%; the most common ED in these patients is eating disorder not otherwise specified (EDNOS) [5]. Fortunately, the available data suggest that comorbidity rates between BPD and ED decrease significantly over time, with one study showing that most individuals with BPD who met criteria for ED experienced remission over time [5].
Anorexia nervosa is a serious condition associated with high rates of morbidity and mortality. In patients with severe AN comorbid with BPD, the general recommendations in clinical guidelines for AN should be followed in terms of treatment setting, day hospital treatment, psychotherapy, or nutritional management independently of BPD comorbidity [39]. As all the clinical guidelines point out, there is a notable lack of evidence to support pharmacotherapy for AN, and most guidelines strongly recommend caution when prescribing drugs in this patient population due to the risk of medical complications. Nonetheless, some guidelines suggest that short-term treatment with SSRIs or low-dose antipsychotics (especially olanzapine) may be justified in certain cases, such as in patients with a critically low body mass index [39, 40].
For individuals with BPD and less severe, non-life-threatening EDs (AN, BN, or EDNOS), the disorder should be managed concurrently with BPD-specific treatment, preferably coordinated by the BPD therapist [2]. Nevertheless, Carmona I Farrés et al. [41] suggested that comorbidity between BPD and EDs predicted early dropout from DBT skills training. In this regard, effective adaptations of DBT have been developed for individuals with comorbid BPD and ED, which could improve treatment retention in these patients [2, 41]. For individuals who have difficulty accessing first-line psychotherapy or who do not respond to therapy, second-line psychotherapy may be helpful. Although the current evidence base is weak, psychotropic medications, which may affect appetite and body weight, could be prescribed as an adjunct to psychotherapy [39, 40]. This pharmacological treatment includes antidepressants (SSRIs; e.g., fluoxetine), antipsychotics (e.g., quetiapine), psychostimulants (e.g., lisdexamfetamine), and anticonvulsants (e.g., topiramate) [37].
5 Comorbid Substance Use Disorders
BPD is generally characterized by greater impulsivity and a preference for short-term rewards. This inability to focus on the long term predisposes patients to develop SUD [5]. The overall lifetime prevalence of SUD in patients with BPD is approximately 78% [2,3,4]. However, longitudinal studies show that despite the high prevalence of SUD in this patient population, prevalence rates tend to decrease over time [5].
The first-line treatment for patients with comorbid BPD and SUD is psychological therapy, although it is important to note that the presence of comorbid SUD increases the risk of early dropout from psychotherapy for BPD [2, 41, 42]. Specific treatment manuals designed to lower the risk of treatment dropout and improve efficacy have been developed for patients with comorbid BPD and SUD [40]. In these patients, there are several potentially effective treatment options, including a version of DBT adapted specifically for BPD patients with comorbid SUD (DBT–SUD), dynamic deconstructive psychotherapy, and schema therapy for addiction (Dual Focus Schema Therapy; DFST) [42,43,44,45].
In cases of severe substance use, the treatment of the SUD should be prioritized over BPD, especially when psychotherapy is not effective or when the patient expresses a preference to receive treatment for the SUD, which may include hospitalization and/or pharmacological treatment. However, patients should be informed about the limited evidence for the efficacy of pharmacological treatment, as well as the risks and benefits of the various pharmacological alternatives. Studies have shown that patients with alcohol use disorder (AUD) and BPD comorbidity benefit from pharmacotherapy to the same extent as patients with a dependence disorder without this comorbidity [46]. Consequently, treatments for AUD, which include disulfiram, naltrexone, and acamprosate for relapse prevention, should always be offered to these patients [42, 46]. Other off-label medications, such as anticonvulsants (e.g., pregabaline, gabapentine, or topiramate) or atypical antipsychotics (e.g., quetiapine or olanzapine), may be considered [46]. Prescription of these drugs should be done cautiously, keeping in mind the need to avoid polypharmacy and to limit the use of sedatives.
6 Conclusions
Comorbidity with other mental disorders is common in individuals with BPD. The prevalence of these comorbid disorders tends to decrease gradually over time in parallel with the clinical improvement of the typical symptoms that characterize BPD. No drugs have yet been approved specifically for the treatment of BPD. Nonetheless, various medications are routinely prescribed off label for this condition despite the lack of agreement among clinical guidelines. Comorbidity between BPD and other psychiatric disorders is considered to be the main factor associated with both pharmacological treatment and polypharmacy in these patients.
Our review of the evidence leads us to make the following conclusions and clinical recommendations for the management of patients with BPD and a comorbid disorder: (1) psychotherapy should be the first-line treatment for all individuals with BPD, regardless of whether a comorbidity is present or not; (2) while some drugs can be helpful, their main role is as an adjunct to BPD-specific psychotherapy; (3) off-label drug prescription and polypharmacy is common in BPD despite the lack of robust evidence; (4) patients who receive BPD-specific psychotherapy usually require fewer medications, which can help to reduce polypharmacy; (5) BPD-specific treatment should be prioritized over the treatment of comorbidities, except for severe episodes of MDD, severe substance use, or life-threatening AN; (6) pharmacotherapy may be useful in severe cases, or when psychotherapy is ineffective, but it is important to avoid polypharmacy and sedatives. Likewise, the patient should be informed about the possible adverse side effects of these drugs and about alternative medications. Doing so allows the patient to take an active role in decision-making, which is important given the uncertainty surrounding the optimal treatment approach (2).
Finally, we need the identification of new pharmacological targets in the treatment of BPD and new drug candidates to treat BPD and comorbidities with potential beneficial effects, such as psychedelic-assisted psychotherapy approaches [47, 48]. New clinical trials and naturalistic studies are needed to clarify the role of pharmacotherapy in the treatment of BPD, particularly in patients with comorbid conditions. Despite the relatively weak evidence base, we believe that clinicians will find the recommendations and algorithms proposed here for the pharmacological treatment of individuals with BPD and comorbidities to be of value for the clinical management of these patients.
References
American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 5th edn. 2022. American Psychiatric Publishing. https://doi.org/10.1176/appi.books.9780890425787.
Bohus M, Stoffers-Winterling J, Sharp C, et al. Borderline personality disorder. Lancet. 2021;398(10310):1528–40. https://doi.org/10.1016/S0140-6736(21)00476-1.
Trull TJ, Jahng S, Tomko RL, et al. Revised NESARC personality disorder diagnoses: gender, prevalence, and comorbidity with substance dependence disorders. J Pers Disord. 2010;24(4):412–26. https://doi.org/10.1521/pedi.2010.24.4.412.
Tomko RL, Trull TJ, Wood PK, et al. Characteristics of borderline personality disorder in a community sample: comorbidity, treatment utilization, and general functioning. J Pers Disord. 2014;28(5):734–50. https://doi.org/10.1521/pedi_2012_26_093.
Shah R, Zanarini MC. Comorbidity of borderline personality disorder: current status and future directions. Psychiatr Clin N Am. 2018;41(4):583–93. https://doi.org/10.1016/j.psc.2018.07.009.
Alvarez-Tomás I, Soler J, Bados A, et al. Long-term course of borderline personality disorder: a prospective 10-year follow-up study. J Pers Disord. 2017;31(5):590–605. https://doi.org/10.1521/pedi_2016_30_269.
Linehan M. Cognitive-behavioral treatment of borderline personality disorder. New York: Guilford Press; 1993.
Choi-Kain LW, Finch EF, Masland SR, Jenkins JA, Unruh BT. What works in the treatment of borderline personality disorder. Curr Behav Neurosci Rep. 2017;4(1):21–30. https://doi.org/10.1007/s40473-017-0103-z.
Gunderson J, Masland S, Choi-Kain L. Good psychiatric management: a review. Curr Opin Psychol. 2018;21:127–31. https://doi.org/10.1016/j.copsyc.2017.12.006.
Storebø OJ, Stoffers-Winterling JM, Völlm BA, et al. Psychological therapies for people with borderline personality disorder. Cochrane Database Syst Rev. 2020;5(5):CD012955. https://doi.org/10.1002/14651858.CD012955.pub2.
Soler J, Casellas-Pujol E, Fernández-Felipe I, et al. “Skills for pills”: the dialectical-behavioural therapy skills training reduces polypharmacy in borderline personality disorder. Acta Psychiatr Scand. 2022;145(4):332–42. https://doi.org/10.1111/acps.13403.
Stoffers-Winterling JM, Storebø OJ, Pereira Ribeiro J, et al. Pharmacological interventions for people with borderline personality disorder. Cochrane Database Syst Rev. 2022;11(11):CD012956. https://doi.org/10.1002/14651858.CD012956.pub2.
Zanarini MC, Frankenburg FR, Reich DB, et al. Rates of psychotropic medication use reported by borderline patients and axis II comparison subjects over 16 years of prospective follow-up. J Clin Psychopharmacol. 2015;35(1):63–7. https://doi.org/10.1097/JCP.0000000000000232.
Crawford MJ, Kakad S, Rendel C, et al. Medication prescribed to people with personality disorder: the influence of patient factors and treatment setting. Acta Psychiatr Scand. 2011;124(5):396–402. https://doi.org/10.1111/j.1600-0447.2011.01728.x.
Martín-Blanco A, Ancochea A, Soler J, et al. Changes over the last 15 years in the psychopharmacological management of persons with borderline personality disorder. Acta Psychiatr Scand. 2017;136(3):323–31. https://doi.org/10.1111/acps.12767.
Riffer F, Farkas M, Streibl L, et al. Psychopharmacological treatment of patients with borderline personality disorder: comparing data from routine clinical care with recommended guidelines. Int J Psychiatry Clin Pract. 2019;23(3):178–88. https://doi.org/10.1080/13651501.2019.1576904.
Paton C, Crawford MJ, Bhatti SF, et al. The use of psychotropic medication in patients with emotionally unstable personality disorder under the care of UK mental health services. J Clin Psychiatry. 2015;76(4):e512–8. https://doi.org/10.4088/JCP.14m09228.
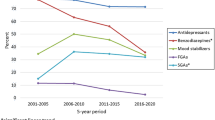
Pascual JC, Martín-Blanco A, Soler J. Twenty-year trends in psychopharmacology treatment of outpatients with borderline personality disorder: a cross-sectional naturalistic study in Spain. CNS Drugs. 2021;35(9):1023–32. https://doi.org/10.1007/s40263-021-00852-7.
National Collaborating Centre for Mental Health (UK). Borderline personality disorder: treatment and management. British Psychological Society (UK); 2009. PMID: 21796831.
Pascual JC, Martín-Blanco A, Soler J, et al. A naturalistic study of changes in pharmacological prescription for borderline personality disorder in clinical practice: from APA to NICE guidelines. Int Clin Psychopharmacol. 2010;25(6):349–55. https://doi.org/10.1097/YIC.0b013e32833e23ed.
Gunderson JG, Morey LC, Stout RL, et al. Major depressive disorder and borderline personality disorder revisited: longitudinal interactions. J Clin Psychiatry. 2004;65(8):1049–56. https://doi.org/10.4088/jcp.v65n0804.
Corruble E, Ginestet D, Guelfi J. Comorbidity of personality disorders and unipolar major depression: a review. J Affect Disord. 1996;37:157–70. https://doi.org/10.1016/0165-0327(95)00091-7.
Rao S, Broadbear J. Borderline personality disorder and depressive disorder. Australas Psychiatry. 2019;27(6):573–7. https://doi.org/10.1177/1039856219878643.
Skodol AE, Grilo CM, Keyes KM, et al. Relationship of personality disorders to the course of major depressive disorder in a nationally representative sample. Am J Psychiatry. 2011;168(3):257–64. https://doi.org/10.1176/appi.ajp.2010.10050695.
Zanarini MC, Frankenburg FR, Hennen J, et al. Axis I comorbidity in patients with borderline personality disorder: 6-year follow-up and prediction of time to remission. Am J Psychiatry. 2004;161(11):2108–14. https://doi.org/10.1176/appi.ajp.161.11.2108.
Plöderl M, Hengartner MP. Guidelines for the pharmacological acute treatment of major depression: conflicts with current evidence as demonstrated with the German S3-guidelines. BMC Psychiatry. 2019;19:265. https://doi.org/10.1186/s12888-019-2230-4.
Bauer M, Severus E, Köhler S, et al. World Federation of Societies of Biological Psychiatry (WFSBP) guidelines for biological treatment of unipolar depressive disorders. part 2: maintenance treatment of major depressive disorder-update 2015. World J Biol Psychiatry. 2015;16(2):76–95. https://doi.org/10.3109/15622975.2014.1001786.
Kennedy SH, Lam RW, McIntyre RS, et al. Canadian Network for Mood and Anxiety Treatments (CANMAT) 2016 clinical guidelines for the management of adults with major depressive disorder: Section 3. Pharmacological treatments. Can J Psychiatry. 2016;61(9):540–60. https://doi.org/10.1177/0706743716659417.
Parikh SV, Quilty LC, Ravitz P, et al. Canadian Network for Mood and Anxiety Treatments (CANMAT) 2016 clinical guidelines for the management of adults with major depressive disorder: section 2. Psychological treatments. Can J Psychiatry. 2016;61(9):524–39. https://doi.org/10.1177/0706743716659418.
Ceresa A, Esposito CM, Buoli M. How does borderline personality disorder affect management and treatment response of patients with major depressive disorder? A comprehensive review. J Affect Disord. 2021;281:581–9. https://doi.org/10.1016/j.jad.2020.11.111.
Crawford MJ, Sanatinia R, Barrett B, et al. The clinical effectiveness and cost-effectiveness of lamotrigine in borderline personality disorder: a randomized placebo-controlled trial. Am J Psychiatry. 2018;175(8):756–64. https://doi.org/10.1176/appi.ajp.2018.17091006.
Elices M, Soler J, Feliu-Soler A, et al. Combining emotion regulation and mindfulness skills for preventing depression relapse: a randomized-controlled study. Borderline Personal Disord Emot Dysregul. 2017;4:13. https://doi.org/10.1186/s40479-017-0064-6.
Bandelow B, Werner AM, Kopp I, et al. The German guidelines for the treatment of anxiety disorders: first revision. Eur Arch Psychiatry Clin Neurosci. 2022;272(4):571–82. https://doi.org/10.1007/s00406-021-01324-1.
Harned MS, Korslund KE, Linehan MM. A pilot randomized controlled trial of dialectical behavior therapy with and without the dialectical behavior therapy prolonged exposure protocol for suicidal and self-injuring women with borderline personality disorder and PTSD. Behav Res Ther. 2014;55:7–17. https://doi.org/10.1016/j.brat.2014.01.008.
Simonsen S, Bateman A, Bohus M, et al. European guidelines for personality disorders: past, present and future. Borderline Person Disord Emot Dysregul. 2019;21(6):9. https://doi.org/10.1186/s40479-019-0106-3.
Katzman MA, Bleau P, Blier P, et al. Canadian clinical practice guidelines for the management of anxiety, posttraumatic stress and obsessive-compulsive disorders. BMC Psychiatry 2014;14(Suppl 1):S1. https://doi.org/10.1186/1471-244X-14-S1-S1.
Pascual JC, Córcoles D, Castaño J, et al. Hospitalization and pharmacotherapy for borderline personality disorder in a psychiatric emergency service. Psychiatr Serv. 2007;58(9):1199–204. https://doi.org/10.1176/ps.2007.58.9.1199.
Sansone RA, Levitt JL, Sansone LA. The prevalence of personality disorders among those with eating disorders. Eat Disord. 2005;13(1):7–21. https://doi.org/10.1080/10640260590893593.
Resmark G, Herpertz S, Herpertz-Dahlmann B, Zeeck A. Treatment of anorexia nervosa-new evidence-based guidelines. J Clin Med. 2019;8(2):153. https://doi.org/10.3390/jcm8020153.
Hilbert A, Hoek HW, Schmidt R. Evidence-based clinical guidelines for eating disorders: international comparison. Curr Opin Psychiatry. 2017;30(6):423–37. https://doi.org/10.1097/YCO.0000000000000360.
Carmona I, Farrés C, Pascual JC, Elices M, et al. Factors predicting early dropout from dialectical behaviour therapy in individuals with borderline personality disorder. Actas Esp Psiquiatr. 2018;46(6):226–33 (PMID: 30552812).
Kienast T, Stoffers J, Bermpohl F, Lieb K. Borderline personality disorder and comorbid addiction. Dtsch Arztebl Int. 2014;111(16):280–6. https://doi.org/10.3238/arztebl.2014.0280.
Dimeff LA, Linehan MM. Dialectical behavior therapy for substance abusers. Addict Sci Clin Pract. 2008;4(2):39–47. https://doi.org/10.1151/ascp084239.
Gregory RJ, DeLucia-Deranja E, Mogle JA. Dynamic deconstructive psychotherapy versus optimized community care for borderline personality disorder co-occurring with alcohol use disorders: a 30-month follow-up. J Nerv Ment Dis. 2010;198:292–8. https://doi.org/10.1097/NMD.0b013e3181d6172d.
Ball SA. Manualized treatment for substance abusers with personality disorders: dual focus schema therapy. Addict Behav. 1998;23(6):883–91. https://doi.org/10.1016/s0306-4603(98)00067-7.
Reus VI, Fochtmann LJ, Bukstein O, et al. The american psychiatric association practice guideline for the pharmacological treatment of patients with alcohol use disorder. Am J Psychiatry. 2018;175(1):86–90. https://doi.org/10.1176/appi.ajp.2017.1750101.
Mithoefer MC, Mithoefer AT, Feduccia AA, et al. 3,4-methylenedioxymethamphetamine (MDMA)-assisted psychotherapy for post-traumatic stress disorderin military veterans, firefighters, and police officers: a randomised, double-blind, dose-response, phase 2 clinical trial. Lancet Psychiatry. 2018;5(6):486–97. https://doi.org/10.1016/s2215-0366(18)30135-4.
Domínguez-Clavé E, Soler J, Pascual JC, et al. Ayahuasca improves emotion dysregulation in a community sample and in individuals with borderline-like traits. Psychopharmacology. 2019;236(2):573–80. https://doi.org/10.1007/s00213-018-5085-3.
Acknowledgements
We would like to thank Bradley Londres (biomedical editor and translator at Londres Biomedical Editing) for professional English language editing of the final version of the manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
This study was supported by the Centro de Investigación Biomédica en Red de Salud Mental (CIBERSAM) and by a grant from Instituto de Salud Carlos III (PI21/00505) and co-financed by the European Regional Development Fund (ERDF). Open Access Funding provided by Universitat Autonoma de Barcelona.
Conflict of interest
Juan C. Pascual, Laia Arias, and Joaquim Soler declare they have no conflicts of interest.
Ethics approval
This study adhered to the principles outlined in the Declaration of Helsinki.
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Availability of data and material
Not applicable.
Code availability
Not applicable.
Authors’ contributions
All three authors contributed equally to designing and writing this manuscript and approved the final version for submission and agree to be accountable for the work.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Pascual, J.C., Arias, L. & Soler, J. Pharmacological Management of Borderline Personality Disorder and Common Comorbidities. CNS Drugs 37, 489–497 (2023). https://doi.org/10.1007/s40263-023-01015-6
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40263-023-01015-6